FOI 24/25-0223
Document 15
Research Request – Efficacy of Rehabilitation Training
Machines
Brief
Efficacy of Rehabilitation Training Machines (Motomed/Active passive trainer/FES
Cycling):
- Evidence of use in populations such as SCI, MS, stroke, Parkinson’s disease and
cerebral palsy
- Evidence of benefits including health outcomes and carryover into functional benefits
- Dosages trialled and recommended
- Any comparisons made to standard treatment regimes
Date 03/06/2020
Requester Maureen Ss47F - personal privacy
Researcher Jane Ss47F - personal privacy
Cleared by Jane Ss47F - personal privacy
P a g e |
1
Page 1 of 39

FOI 24/25-0223
Document 15
Table of Contents
Summary ................................................................................................................................................. 3
1. Efficacy of Rehabilitation Training Machines .................................................................................. 4
1.1 Multiple Sclerosis .......................................................................................................................... 4
1.1.1 MOTOmed and/or Active Passive Trainer ............................................................................. 4
1.1.2 FES cycling .............................................................................................................................. 5
1.1.3 Conventional Exercise Training Programs.............................................................................. 5
1.2 Spinal Cord Injury ........................................................................................................................ 13
1.2.1 MOTOmed and/or Active Passive Trainer ........................................................................... 13
1.2.2 FES cycling ............................................................................................................................ 13
1.2.3 Conventional Exercise Training Programs............................................................................ 14
1.3 Stroke .......................................................................................................................................... 22
1.3.1 MOTOmed and/or Active Passive Trainer ........................................................................... 22
1.3.2 FES cycling ............................................................................................................................ 23
1.4 Parkinson’s disease ..................................................................................................................... 28
1.4.1 MOTOmed and/or Active Passive Trainer ........................................................................... 28
1.4.2 FES cycling ............................................................................................................................ 28
1.5 Cerebral Palsy .............................................................................................................................. 32
1.5.1 MOTOmed and/or Active Passive Trainer ........................................................................... 32
1.5.2 FES cycling ............................................................................................................................ 32
1.5.3 Conventional Exercise Training Programs............................................................................ 32
Reference List ........................................................................................................................................ 38
Please note:
The research and literature reviews col ated by our TAT Research Team are not to be shared
external to the Branch. These are for internal TAT use only and are intended to assist our advisors
with their reasonable and necessary decision making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates require
further information on access or planning matters they are to cal the TAPS line for advice.
P a g e |
2
Page 2 of 39

FOI 24/25-0223
Document 15
Summary
MOTOmed and/or Active Passive Trainer
-Quality of research is generally of medium-high quality across stroke, SCI, Parkinson’s
disease and cerebral palsy. Although, many studies conclude that further research is needed
which included larger control ed samples and utilise consistent outcomes measures and
interventions.
-Results vary between conditions as different outcome measures are used, however, there
is evidence to suggest that these rehabilitation trainers can increase cardiovascular,
musculoskeletal and neurological outcomes.
- Long term health and functional related outcomes were rarely reported. The longest
intervention duration reported was 12 weeks
- Dosages vary significantly. On average, studies investigated interventions which lasted 20-
30 minutes, 2-3 times a week
-Refer to individual disorders for separate research on MOTOmed and/or Active Passive
Trainers
-Very few studies investigated the devices in a home setting
FES cycling
-Quality of research into FES cycling for multiple sclerosis and cerebral palsy was low to very
low. There is a paucity of evidence looking at FES cycling for those with Parkinson’s disease
with only a single subject design study discovered. Stork and spinal cord injury had greater –
quality research evidence ranging from medium to high.
-Research from all diseases showed mixed results across cardiorespiratory and functional
performance, as well as musculoskeletal and psychological outcomes. For example, some
studies found reduced spasticity in those with SCI and others did not. See individual diseases
for exact findings.
-Differences in the duration and effort of intervention, as wel as outcome measures used
led to significant heterogeneity and inability to directly compare results within and between
diseases
- Significant variation in dosages ranging from 10-90 minutes, 2-7 times per week over 2 to
24 weeks.
- Long term health and functional related outcomes were rarely reported. The longest
intervention duration reported was 24 weeks.
-Very few studies investigated the devices in a home setting
Where possible, conventional exercise training programs are also provided if a systematic
review existed on the topic. This allows for some comparison to regular physical therapy
interventions that are currently delivered to these cohorts of patients.
P a g e |
3
Page 3 of 39

FOI 24/25-0223
Document 15
1. Efficacy of Rehabilitation Training Machines
1.1 Multiple Sclerosis
1.1.1 MOTOmed and/or Active Passive Trainer
A single randomised controlled trial (RCT) [1] has investigated the effectiveness of a neuro-
physiotherapy programme based on feedback cycling for improving gait in patients with
multiple sclerosis (MS) using a
MOTOmed device.
This study included 61 patients with mild to moderate MS. Half performed one 30 minute
session per week for three months using the MOTOmed Viva2 Movement Trainer in
addition to a personalised exercise program to be completed at home. The control group
only received the personalised at home exercise program.
No significant differences in walking speed or cadence (steps per minute) between groups.
Intervention group showed statistical y significant improvements in Functional Ambulatory
Performance (FAP) across all time intervals. Stride length significantly improved in the
intervention group across al time intervals and between baseline and final measurement in
the control group.
Quality = Medium
- Results suggest that visual biofeedback cycling training may be a viable. However, larger
studies are required with different treatment intervals to determine efficacy
An RCT by Barclay et al. (2019) [2] evaluated the feasibility of a progressive, four week lower
limb cycling programme using
active passive trainers (APT's) on spasticity, cardiovascular
fitness, function and quality of life in people with moderate to severe MS.
• Intervention group
- 30 min of APT cycling (2 min passive warm up, 26 min active cycling and 2 min
passive cool down)
- 20 sessions (5 days per week for four weeks in addition to usual care)
• Control group
-Individualised therapy programme, delivered Monday to Friday
• Performed in a clinical setting
Results
• Average power output, distance cycled and speed improved in the intervention
group but this did not translate to statistical changes in the outcome measures.
• Improvements were shown across both groups for physical health and mental
health. Effect Size = 0.93 intervention and 0.46 control
• Cardiovascular health = Medium effect size in intervention (0.36) compared to
control group (0.07)
Quality = Medium
- Smal sample size and intervention group also underwent usual care so difficult to separate effect
of the intervention.
P a g e |
4
Page 4 of 39

FOI 24/25-0223
Document 15
1.1.2 FES cycling
Two systematic reviews [3, 4] examining the outcomes of people with MS with mobility
impairment following Functional Electrical Stimulation (FES) cycling have been conducted.
Both reviews found that intervention duration ranged from 10-60 minutes, 2-3 times per
week over 2 to 24 weeks. The majority were performed in clinical settings (89%).
Stimulation parameters for most trials involved a pulse width of 200–300 μ sec at a
frequency of 20–50 Hz and a cycling cadence of 10–50 rpm. All stimulated the quadriceps,
hamstrings, and gluteal muscle groups, with the exception of one trial.
•
Cardiorespiratory performance (VO2 max, peak aerobic capacity, peak work rate,
power generation) = No improvement
•
Functional performance (2-min walk test, 25-foot walk test, 10m walk test or 12
item MS walking scale)
= No significant improvement
•
Musculoskeletal outcomes = No improvement in lower body strength (knee and hip
parameters) or long term improvements in spasticity
- Significant reduction in spasticity directly post FES
•
Psychological outcomes = No improvement in Quality of Life (QOL) or mental health
scores
- High levels of participant satisfaction
•
Adverse events = 10 adverse events reported across studies including skin irritation,
increased spasticity, bowel dysfunction and fatigue
Quality – Low
These reviews included studies of low quality (pre-post studies with no control group,
retrospective and case studies) and a single RCT which didn’t perform blinding or achieve a
sufficient sample size which introduces bias and limits generalisability. This precludes any
definitive conclusions regarding the efficacy of FES cycling for MS.
1.1.3 Conventional Exercise Training Programs
Two systematic reviews examining the benefits of ‘exercise training’ in patients with MS
have been conducted.
1) Latimer-Cheung et al. (2013) [5] investigated patients with mild-moderate MS and
performed a meta-analysis and combined the below interventions;
-Ergometer
-Technogym equipment
-Resistance training with simultaneous electrostimulation
-Static bike
-Plyometric exercises
-Walking
-Balancing
-Stretching
-Swimming
P a g e |
5
Page 5 of 39

FOI 24/25-0223
Document 15
-Treadmill
-Calisthenics
-Yoga
-Therabands
Results
-Consistent and strong evidence that aerobic and resistance exercise performed 2 times per
week at a moderate intensity increases physical capacity and muscular strength,
respectively.
- Evidence supporting the benefits of exercise on mobility and fatigue is promising, there is
insufficient evidence to definitively establish the prescriptive amounts, intensities, or types
of exercise to improve these outcomes.
-Not enough good-quality evidence to date supporting the benefits of exercise for improving
Health related QOL outcomes.
-No evidence that FES cycling is effective for increasing strength.
Quality – High
Inclusion of high quality RCTs (29/54). Consistent finding and ability to perform a meta-
analysis shows homogeneity in outcome measures
2) Edwards et al. (2017) [6] investigated studies which included participants with severe MS
(severe mobility issues). The number of studies were limited compared to those which
investigate mild-moderate MS.
Results
Mixed results across all outcomes for all treatment types
•
Conventional exercise training: no statistical y significant improvements in any of
the outcomes
•
Conventional resistance exercise training
-Significant improvements in muscular strength, muscle endurance, balance, fatigue
symptoms, and QOL when combined with neuromuscular electrical stimulation
•
Bodyweight support treadmil training
-Mixed results (some positive others no change) across outcomes on level of
disability, knee extensor strength, walking, endurance, walking speed, gait
kinematics, balance and agility, fatigue, QOL
•
Total body recumbent stepper training (one study)
-No change in disability or physical function reported. Fatigue significantly reduced
after the intervention.
Quality – Medium
Significant heterogeneity led to
inability to perform meta-analysis. Further research is
necessary to determine the most efficacious and effective exercise approaches for
individuals with MS with severe mobility disability due to the limited amount of quality
evidence
P a g e |
6
Page 6 of 39

FOI 24/25-0223
Document 15
Table 1
Author
Study aim
Method/participants Treatment/Intervention/
Outcome/summary
Quality of evidence
(year) and
characteristics
Setting
country
Low/Medium/
High
Multiple Sclerosis
Hochspung To analyse the
RCT (double-blind)
-During the study period,
No significant differences in walking speed or
Medium
et al.
effectiveness of a
none of the participants
cadence were observed between stages in any
(2017) [1]
neuro-physiotherapy 61 patients with mild received other types of
of the groups
-Lack of follow-up and
programme based
to moderate MS
physiotherapy.
the small size prevent
on feedback cycling
Functional Ambulatory Performance (FAP)
generalisation of
for improving gait in Inclusion criteria: (
1)
Intervention group
- intervention group showed statistically
results.
patients with MS.
referral by
- stationary bicycle with a
significant changes between stages 0 and 1 (
P <
neurologist
coordination feedback
.014) and between stages 0 and 2 (
P < .002)
-Significant
(
2) diagnosis of
programme to work on lower - no such differences were observed in the
improvements
definite MS
limb strength asymmetry
control group
only in FAP and stride
according to the
using 75% of the maximum
length
McDonald criteria at
resistance
Stride length
least 2 years
- one 30-minute session per
- significant differences in stride length
-12 sessions not enough
previously;
week for 3 months using the
between stages 0 and 2 (
P < .001) and between for long term results
(
3) EDSS score
MOTOmed Viva2 Movement
stages 1 and 2 (
P < .002)
between 2 and 6
Trainer
- controls only displayed significant differences -Results show that
(
4) age between 20
- personalised exercise
in stride length between stages 0 and 2 (
P <
visual biofeedback
and 70 years; (
5)
programme to be completed
.004)
cycling training
clinical stability
at home
may be a viable,
during the 3 months
effective treatment in
previous to
Control group
patients with MS but
recruitment; (
6) no
- personalised exercise
larger studies are
cognitive impairment programme to be completed
required.
according to the
at home
P a g e |
7
Page 7 of 39

FOI 24/25-0223
Document 15
Mini-Mental State
Examination
Barclay et
To evaluate the
Randomised Trial
Clinic setting
15 intervention and 9 control
Medium
al. (2019)
feasibility of a
[2]
progressive, four
not powered to show
APT group (intervention): - 30 -Improvements were noted in the majority of
-Small sample
week lower limb
statistically
min of APT cycling (2 min
outcome measures, although no statistically
-Very few clinical or
cycling programme
significant changes
passive warm up, 26 min
significant group differences were found.
significant effects
using
active passive
active cycling and 2 min
-Intervention group also
trainers (APT's) on
Inclusion:
passive cool down)
-The average power output, distance cycled
underwent usual care
spasticity,
(a) Confirmed
-20 sessions (Five days per
and speed improved in the intervention
so difficult to separate
cardiovascular
diagnosis of MS, (b)
week for four weeks in
group but this did not translate to statistical
effects of the
fitness, function and aged over 18, (c)
addition to usual care)
changes in the outcome measures.
intervention from the
quality of life in
expanded Disability
intensive therapy
people with
Status Scale (EDSS) of
Usual care:
-lack of objective change in spasticity
moderate to severe
between 6.0 and 8.5. Individualised therapy
MS.
programme, delivered
-Improved walking speed in 7/16 participants in
Exclusion:
Monday to Friday, and could
the intervention group compared to 2 in the
(a) Significant
include PT, OT, SLT and
control
cognitive
Psychology.
impairment, (b) co-
Improvements were shown across both
morbidities which
physical health (PH) and mental health (MH). ES
would preclude them
= 0.93 intervention and 0.46 control
taking part in
exercise, (c) visual
Medium effect in intervention (0.36) for
Impairment, (d)
cardiovascular health and negligible (0.07) for
unable to be seated
control
appropriately in a
wheelchair for 30
min.
Scally et al. To systematically
Systematic Review
Intervention duration ranged
Cardiorespiratory performance
Low
(2020) [3]
examine the
between 2 and 24 weeks
outcomes of people
(1) human
Functional performance
Low quality (study
with MS with
participants with
8 studies in clinic setting
-No significant changes in 2-min walk test, 25-
design and sample
mobility impairment definite diagnosis of
1 in home
foot walk test, 10m walk test or 12 item MS
sizes) of the literature
MS
walking scale
base precludes any
P a g e |
8
Page 8 of 39

FOI 24/25-0223
Document 15
following
FES cycling (2) aged 18 years and Average 2-3 sessions per
definitive conclusions
intervention.
over
week
Musculoskeletal outcomes
regarding the efficacy of
(3) average EDSS 6.0
-No improvement in lower body strength (knee FES cycle training in
or above, or an
Min 10-60 minutes per
and hip parameters)
improving
equivalent mobility
session
- Significant reduction in spasticity directly post cardiovascular health in
impairment
FES
MS and higher EDSS
(4) evaluate FES
- No long term improvements in spasticity
scores.
cycling as an
intervention study
Psychological outcomes
RCT’s did not blind
-No improvement in QOL or mental health
participants or
5 pre-post studies
scores
providers and not
with no control
sufficient power to
group, 2 randomised
Adverse events
detect a difference.
controlled trials
10 adverse events reported across studies
(RCTs), 1
including skin irritation, increased spasticity,
FES cycle training
retrospective study
bowel dysfunction and fatigue
appears to be well
and 1 case study.
tolerated in MS with
mobility impairment,
with no serious adverse
events.
Pilutti et al. Summary of the
Systematic Review
Intervention
Safety and tolerability
Low
(2019) [4]
current evidence for
-Preliminary evidence supports the safety and
FES cycling as an
Acute and chronic
-Durations ranged between 2 tolerability of FES cycling exercise
limited but promising
exercise training
FES cycling as an
and 24 weeks
evidence for the
modality in persons
exercise modality in
Acute effects
application of FES
with MS
persons with MS
-Sessions delivered 2–3×/
-Studies support the potential for modification
cycling exercise among
week for between 10 and 60
of
persons with MS who
8 included studies,
min/session.
muscle spasticity, cycling kinematics, and
have moderate-to-
only 1 RCT
cardiorespiratory metabolism with
severe disability.
-Stimulation parameters for
single sessions of FES cycling
Samples were small
most trials involved a pulse
- Acute benefits may, with chronic exposure to
High-quality RCTs of FES
(n = 1–14)
width of 200–300 μ sec at a
FES cycling, result in long-term adaptations
cycling exercise are now
frequency of 20–50 Hz and a
needed to establish the
participants had
cycling cadence of 10–50 rpm. Chronic effects
safety and efficacy of
-All stimulated the
- potential for strength adaptations with
this promising modality
quadriceps, hamstrings, and
P a g e |
9
Page 9 of 39

FOI 24/25-0223
Document 15
Moderate-to-severe
gluteal muscle groups, with
FES cycling likely depends on the specific
for people living with
disability (EDSS range the exception of one trial
muscle groups that are peripherally
MS
reported = 4.0–7.5).
Stimulated
- changes in body composition in response to
FES cycling exercise in persons
with MS are unclear
- no effect of FES
cycling delivered between 2 and 24 weeks on
spasticity
-No improvements in QOL
-High levels of participant satisfaction
Latimer-
To conduct a
Systematic Review
Clinic and Home
54 included studies
High
Cheung et
systematic review of
al. (2013)
evidence
Both randomised and -Ergometer
There was consistent and strong evidence that
-More than half of
[5]
surrounding the
non-randomised
-Technogym equipment
aerobic and resistance exercise performed 2
included studies were
effects of
exercise
studies included (29
-Resistance training with
times per week at a moderate intensity
RCTs of moderate-high
training on physical
high level RCT)
simultaneous
increases physical capacity and muscular
quality
fitness, mobility,
electrostimulation
strength, respectively. While the evidence
fatigue, and Health
Diagnosis of MS
-Static bike
supporting the benefits of exercise on mobility
related quality of life (mild-moderate)
-Plyometric exercises
and fatigue is promising, there is insufficient
in adults with
Focus on: fitness,
-Walking
evidence to definitively establish the
multiple sclerosis
mobility, fatigue or
-Balancing
prescriptive amounts, intensities, or types of
(MS).
health related quality -Stretching
exercise to improve these outcomes. There is
of life benefits
-Swimming
not enough good-quality evidence to date
-Treadmill
supporting the benefits of exercise for
-Calisthenics
improving HRQOL outcomes.
-Yoga
-Therabands
There is no evidence that electrical
stimulation-assisted cycling is effective for
increasing strength.
Edwards et Provide a summary
Systematic Review
conventional exercise training Further research is necessary to determine the
Medium
al. (2017)
of the potential
(aerobic and resistance
most efficacious and effective exercise
[6]
benefits of
exercise
randomized and
exercise) (n= 5)
approaches for individuals with
-Small samples
training in persons
nonrandomized
MS with severe mobility disability due to the
with MS with severe controlled trials, and
limited amount of quality evidence.
P a g e |
10
Page 10 of 39

FOI 24/25-0223
Document 15
mobility disability,
pre-post intervention body-weight support
-Mixed results across all
and a future
designs
treadmill training (BWSTT) (n=
Conventional exercise training
outcomes for al
research agenda for
7)
- no statistically significant improvements in
treatment types
developing effective Diagnosis of MS
any of the outcomes
-Significant
strategies for
(severe mobility
total-body recumbent stepper
heterogeneity led to
managing disability
issues)
training (TBRST) (n = 1)
Conventional resistance exercise training
inability to perform
through exercise
-Significant improvements in muscular
meta-analysis
training.
Functional clectrical
strength, muscle endurance, balance, fatigue
stimulation assisted cycling (n symptoms, and QOL when combined with
= 5)
neuromuscular electrical stimulation
-Low level evidence
Bodyweight support treadmil training
-Mixed results (some positive others no
change) across outcomes on level of disability,
knee extensor strength, walking, endurance,
walking speed, gait kinematics, balance and
agility, fatigue, QOL
Total body recumbent stepper training (one
study)
-No change in disability or physical function
reported.
-Symptoms of fatigue were significantly
reduced after the intervention
Electrical stimulation assisted cycling
(functional electrical stimulation (FES) and
neuromuscular electrical stimulation (NMES)
cycling)
- Two studies reported significant
improvements in physical fitness assessed as
thigh circumference and muscle oxygen
consumption (mVO2)
-No significant improvements in physical
function
P a g e |
11
Page 11 of 39

FOI 24/25-0223
Document 15
-Mixed evidence for the effects of ESAC on
spasticity, walking speed, and other
participatory outcomes
P a g e |
12
Page 12 of 39

FOI 24/25-0223
Document 15
1.2 Spinal Cord Injury
1.2.1 MOTOmed and/or Active Passive Trainer
Phadke et al. (2019) [7] performed a systematic review to assess the effectiveness of
passive leg cycling interventions on cardiovascular, neuromuscular, and musculoskeletal
outcomes post spinal cord injury (SCI).
Devices utilised in included studies: Ergo-Dom, FNS leg cycle, ERGYS 1 leg cycle, Sevo-
dynamically controlled recumbent ergometer and MOTOmed cycle.
Intervention duration
Single intervention:
5 to 100 minutes per session
Multiple sessions - frequency of the exercise sessions ranged from one to three times per
day, 20 to 90 minutes per session, 2 to 6 days per week, and 6 to 12 weeks total duration
Results
-Two included RCTs reported significant benefits of multiple sessions of passive cycling on
cardiovascular (improved leg blood flow velocity),
musculoskeletal (improved joint range of
motion and markers of muscle hypertrophy), and
neurological outcomes (improved
spasticity and reflex excitability)
-No clear picture emerged with single session studies, with about half the studies showing a
statistically significant improvement in acute responses in
cardiovascular (blood flow
velocity) and
neurological outcomes (short interval intra-cortical inhibition and spasticity),
while the rest reported no change.
Quality – Medium
Only 11 included studies of which only 2 were RCT. More evidence is required to understand
the best parameters for single and multiple sessions of passive cycling.
1.2.2 FES cycling
Multiple literature and systematic reviews have been conducted relating to FES cycling as a
treatment for patients with spinal cord injury (SCI) [8-11]. Two were of higher quality and
will be summarised here [8, 9]. The remaining two were low quality narrative/literature
reviews [10, 11] and can be found in Table 2.
1) Alashram et al. (2020) [8] investigated the effects of the FES-cycling on the lower
extremities spasticity in patients with SCI and found:
• Significant reduction in Modified Ashworth Scale (assess muscle tone and level of
spasticity) and Numerical-Rating-Scale spasticity scores (reduce spasticity) after FES-
cycling post-treatment, and at three and six months fol ow ups (P < 0.05).
• Intervention details were not reported in some of the selected studies so unable to
identify the treatment effect size and the effective treatment protocol
Quality – Medium
P a g e |
13
Page 13 of 39

FOI 24/25-0223
Document 15
Several low quality studies included due to the paucity of evidence. Small sample sizes and
heterogeneity of studies meant a meta-analysis was not conducted.
2) Thomaz et al. (2019) [9] evaluated the effect of electrical stimulation (ES) on skeletal
muscle volume and spasticity in individuals with SCI, however, only results for FES
cycling were retrieved.
- Intervention: 30-45 minutes, 3-4x per week
- Overall effect on muscle volume was statistical y significant in patients with acute
SCI (mean difference: 0.86; 95% CI: 0.04 to 1.69; p < 0.04).
- Non-significant (mean difference: 0.55; 95% CI: −0.31 to 1.41; p = 0.21) effect for
spasticity of the lower limb.
Quality – High
High quality RCTs
1.2.3 Conventional Exercise Training Programs
Hicks et al. (2011) [12] conducted a systematic review of evidence surrounding the effects of
exercise on physical fitness in people with SCI. Broad range of study types included covering
resistance training, arm ergometry, wheelchair exercise and FES, step training and strength
training.
Intervention: Al studies performed the desired intervention 2-5x a week, over a range of 5-
12 weeks (one study performed over 26 weeks)
Results
Overall, Exercise is effective in increasing physical capacity and muscular strength among
people with chronic SCI. There is no evidence to suggest that exercise is harmful to this
population.
See Table 2 for outcomes on Power Output, Aerobic capacity, Muscle strength, Body weight,
Muscle mass Wheelchair propulsion and skil s, Walking and Standing across intervention
types
Quality – Medium
Inclusion of very low quality (level 5) studies may impact results. Although results were
relatively consistent across studies.
P a g e |
14
Page 14 of 39

FOI 24/25-0223
Document 15
Table 2
Author
Study aim
Method/
Treatment/
Outcome/summary
Quality of
(year) and
participants
Intervention/
evidence
country
characteristics
Setting
Low/Medium
/High
Spinal Cord Injury
Phadke et
To assess the
Systematic
Cycling training
Outcome measures used to assess the effects of cycling
Medium
al. (2019).
effectiveness of
Review
parameters
[7]
passive leg
-Two RCTs reported significant benefits of multiple sessions of passive
Evidence from
cycling
Inclusion:
Single intervention: cycling on
cardiovascular (improved leg blood flow velocity),
this systematic
interventions
passive leg
5 to 100 minutes
musculoskeletal (improved joint range of motion and markers of muscle
review indicates
on
cycling
per session
hypertrophy), and
neurological outcomes (improved spasticity and reflex
that multiple
cardiovascular, prospectively in
excitability)
sessions of
neuromuscular, adult
Multiple sessions -
-No clear picture emerged with single session studies, with about half the
passive leg
and
participants
frequency of the
studies showing a statistically significant improvement in acute responses
cycling showed
musculoskeleta (age ≥18 years)
exercise sessions
in
cardiovascular (blood flow velocity) and
neurological outcomes (short
some form of
l outcomes post with SCI
ranged from one to interval intra-cortical inhibition and spasticity), while the rest reported no
beneficial
SCI, and to
three times per
change.
changes across
describe
11 included
day, 20 to 90
-The studies reviewed here showed a diversity of cycling protocols and
cardiovascular,
intensity,
studies
minutes per
outcomes across multiple body systems.
musculoskeletal,
duration, and
(2 RCT, 1 cross-
session, 2 to 6 days
and neurological
type of passive over trial, 8 pre- per week, and 6 to
systems
leg cycling post post)
12 weeks total
SCI
duration.
-More evidence
is required to
Devices used
understand the
Ergo-Dom, FNS leg
best parameters
cycle, ERGYS 1 leg
for single and
cycle, Sevo-
multiple sessions
dynamically
of passive
controlled
cycling.
recumbent
ergometer,
P a g e |
15
Page 15 of 39

FOI 24/25-0223
Document 15
Motomed cycle
Comparisons
No intervention,
FES cycling, resting,
Active + FES cycling,
Alashram
to investigate
Systematic
See note on
-The selected studies demonstrated a significant
Medium
et al.
the effects of
Review
intervention details reduction in the Modified Ashworth Scale (assess muscle tone and level of
(2020) [9]
the FES-cycling
in
spasticity) and Numerical-Rating-Scale spasticity scores (reduce spasticity)
-2 high quality
on the lower
- individuals
outcome/summary after FES-cycling post-treatment, and at three and six months follow ups
studies but
extremities
with
section
(P < 0.05).
remaining were
spasticity in
SCI
low-quality and
patients with
-examined
-Comparison study found significant reduction in the spasticity in the
included due to
SCI.
lower
experimental FES-cycling group (P = 0.02) than in the standard care control the paucity of
extremities
group.
studies
spasticity.
published about
-One reported AE relating to an increase in spasticity and a bowel accident this issue.
2 randomised
cross-over trials
-Intervention details were not reported in some
-Small samples
6 pilot studies
of the selected studies such as: frequency of treatment, treatment time
2 cohort studies
period, session duration, number of electrodes, pulse type, type of FES-
- Heterogeneity
cycling system, pulse width, frequency, and RPM. So unable to identify the
of studies meant
161 total
treatment effect size and the effective treatment protocol.
a meta-analysis
participants
was not
conducted.
Thomaz et
Evaluate the
Systematic
Treatment (relating ES is effective at promoting a discrete, but significant increase in skeletal
High
al. (2019)
effect of
Review and
to FES cycling
muscle volume in patients with SCI with a subsequent reduction in atrophy
[9]
electrical
Meta-Analysis
studies)
and an effect on muscle volume that is similar in patients with complete
studies included
stimulation (ES)
and incomplete injuries.
in this meta-
on skeletal
Only RCT
30 minutes 3x per
analysis were
muscle volume included
week
-ES on muscle volume of the lower limbs, the overall effect was statistically homogeneous
and spasticity
significant in patients with acute SCI (mean difference: 0.86; 95% CI: 0.04 to and evaluated a
in individuals
Patients with
30-45 minutes 4x
1.69; p < 0.04).
respectable
with
SCI
per week
number of
participants
P a g e |
16
Page 16 of 39

FOI 24/25-0223
Document 15
spinal cord
Intervention =
-ES for spasticity of the lower limb, the overall effect was non-significant
injury
ES
(mean difference: 0.55; 95% CI: −0.31 to 1.41; p = 0.21).
Comparison =
other
intervention or
no intervention
7 included
studies
Deley et al. To discuss
Narrative
Unclear duration,
FES allows the participation of greater muscle mass through hybrid
Low
(2015) [10] some evidence-
Review
dosage etc
exercises (FES–cycling associated with arms ergometer or FES–rowing).
based
-Lack of
physiological
Poor search
These different forms of exercise are associated with major benefits to all
methodological
and
strategy (only
systems of the body—muscular, cardiovascular and pulmonary—and
explanation of
methodological PubMed and
induce important training adaptations when used regularly.
studies included
considerations
Google Scholar)
for optimal use
FES appears to be a beneficial and safe method for training in paraplegic
-Narrative review
of FES for
Study types
individuals
and no
training in
included are not
quantitative
paraplegia.
reported
FES rowing appears to provide the greatest outcomes
analysis
Particular
attention is
All in clinical
-Poor outcome
given to the
setting
reporting or
comparison of
intervention
the different
FES methods
Mayson et
To review the
Literature
Interventions
FES cycling is safe for youth with SCI
Low
al. (2014)
evidence on
Review
included FES
[11]
FES cycling
cycling, Passive leg
Based on RCT: FES cycling can positively influence
Due to the
intervention in <21 years with
cycling and ES only
VO2, as wel as quadriceps muscle strength and
limited number
youth with SCI
SCI
Volume. However, ES alone may be more beneficial in reducing cholesterol of intervention
5 studies
levels and increasing thigh muscle volume
publications,
6 included
performed 1 hour
five of which
studies
sessions 3x/ week
involved the
for 6 months
P a g e |
17
Page 17 of 39

FOI 24/25-0223
Document 15
-4 RCT (one
same small
study spread
1 study 30 minutes
sample,
across 4
sessions 3x/ week
it is impossible to
publications)
for 9 months
recommend
-1 case series
optimal
-1 prospective
FES cycling
parameters for
case series
parameters
use of FES cycling
-Applied to:
in children and
Total 40
quadriceps,
adolescents with
participants
hamstrings, gluteal
SCI.
muscles
-Frequency: 33 Hz
-Pulse duration:
150,
200, 250 or 300 μs
-Amplitude: <140
mA
-Resistance
adjusted
by 0.14 nm to
maintain
50 rpm
Hicks et al. To conduct a
Systematic
Include at least one
Power Output
Medium
(2011) [12] systematic
Review
of the fitness
Combined resistance and arm ergometry exercise:
review of
measures below:
-Level 1 and 4 studies have shown the combination
Exercise is
evidence
Physical activity -strength, oxygen
of resistance and aerobic training to improve
effective in
surrounding
or exercise
uptake/consumptio power output of the upper limbs.
increasing
the effects of
training
n, power output,
-
Benefits when performed 2-3x per week over 12 weeks
physical capacity
exercise on
intervention in
peak work capacity,
and muscular
physical fitness persons
body composition,
Wheelchair exercise:
strength among
in people with
diagnosed with
exercise
This single level 4 study showed non-significant
people with
spinal cord
an SCI
performance or
improvements in upper limb power output.
chronic SCI.
injury (SCI).
(paraplegia or
functional
tetraplegia).
performance.
Aerobic capacity
There is no
Arm ergometry exercise:
evidence to
P a g e |
18
Page 18 of 39

FOI 24/25-0223
Document 15
69 included studies -All level 4 studies, arm ergometry has been
suggest that
Case studies,
on chronic SCI
shown to be very effective in improving aerobic capacity.
exercise is
experimental
-3x per week showed benefits after 5 weeks
harmful to this
and quasi
population.
experimental
Wheelchair ergometry exercise:
designs were
-Level 4 and 5 studies. Most show improvements in aerobic capacity
included.
following 3x per week training for as little as 4 weeks.
Combined resistance and arm ergometry exercise:
-Level 4 trials produced conflicting results; two studies (one level 4 study,
and the RCT) showed significant improvement in aerobic capacity fol owing
training 3x per week for 7 and 12 weeks, while the other (level 4 study)
showed no improvement fol owing 3x per week training for 6 weeks.
Resistance training exercise:
-Although resistance training is not traditionally
used to improve aerobic capacity, a single level 4 study
yielded significant improvements in aerobic
capacity. Further, the magnitude of improvement
was comparable to that seen in most other exercise
studies.
Functional electrical stimulation:
- In these level 4 and 5 studies, FES exercise has shown to be very effective
in improving aerobic capacity in as little as 4–6 weeks.
-Exercise schedule 2-3x per week is sufficient for improvement.
Muscle strength
Combined resistance and arm ergometry exercise:
- Level 4, pre–post training studies consistently show
that participation in any form of exercise training that ‘overloads’ the
muscle will result in increases in muscle strength.
-Training frequencies of 3x per week, the level 1
RCT demonstrated significant improvements in
muscle strength with a frequency of 2x per week.
-Training intensities ranged between 50–80% 1RM.
P a g e |
19
Page 19 of 39

FOI 24/25-0223
Document 15
Functional electrical stimulation:
-Level 4, pre–post training studies utilizing FES show
that muscle strength can significantly increase in
the paralyzed muscles
-3x per week over 8 weeks of training
-There is level 1 evidence that FES-assisted arm ergometry training is more
effective in improving triceps strength than arm ergometry alone.
Body weight
Resistance and aerobic exercise:
All of these level 4 studies reported non-significant
increases or decreases in body weight and utilized
a training frequency of 3_ per week with an
intensity ranging from 40 to 80% max. HR.
Functional electrical stimulation
-Level 4 studies reported non-significant increases or decreases in body
weight.
-Frequency of training was 3-5x per week.
Muscle mass
Resistance exercise
-One level 4 study of vibration exercise reported
significant increases in fat free mass with training
-5x per week for 12 weeks
-No other significant changes in lean tissue mass were reported.
Functional electrical stimulation:
A level 2 study reported significant increases in
quadriceps cross-sectional area with a treadmill
training frequency of 2x per week for 26 weeks.
Wheelchair propulsion and skil s
Resistance and aerobic exercise:
P a g e |
20
Page 20 of 39

FOI 24/25-0223
Document 15
-Significant improvements in maximum power output during wheelchair
propulsion were reported
-Most studies trained 3x per week, at moderate–heavy intensities.
Walking
Step training:
-Findings were mixed. Most found significant improvements in overground
walking following body weight supported treadmill training (BWSTT) both
with and without FES.
-Changes in treadmill training parameters emerged in most, but not all
studies, depending on the parameters measured.
-Training ranged from 2 -5x per week; intensity varied
considerably and was often individually determined.
Strength training
-Improvements in overground walking (significance not reported) were
noted after 12 weeks of training, 2–3x per week at 70–85% of 1RM.
Standing
Step training:
This level 5 study showed progressive BWSTT,
3x per week, led to improvements in the ability to stand with a walker.
P a g e |
21
Page 21 of 39

FOI 24/25-0223
Document 15
1.3 Stroke
1.3.1 MOTOmed and/or Active Passive Trainer
1) A systematic review investigating the effectiveness of the MOTOmed trainer was
performed by Shen et al. (2018) [13]. Al included studies were RCTs and a total of 1099
participants were recruited.
Intervention duration
- 20 minutes in 11 studies
- 30 minutes in 6 studies
- 40 minutes in 1
- Unclear in 1 study
- Average 1-2 times per day and 5-7 days per week
- Over 4 to 12 weeks
Al studies compared conventional rehabilitation to MotoMed + conventional rehabilitation.
Results
- MOTOmed movement therapy effectively improves mobility and activities of daily living in
stroke patients with hemiplegia.
- Fugl-Meyer Assessment (assess motor functioning, balance, sensation and joint
functioning)
Z = 7.33,
P < 0.0001
-Modified Ashworth Scale (muscle tone)
Z = 9.19,
P < 0.00001
-Berg Balance Scale
Z = 8.39,
P < 0.00001
- Functional Ambulation Category
Z = 9.61,
P < 0.00001
-10m walk test
Z = 4.49,
P < 0.00001
-Barthel Index (activities of daily living)
Z = 15.6,
P < 0.00001
Quality – High
Consistent findings across al included RCTs
2) A narrative literature review of the efficacy and safety of passive exercise interventions
was conducted by Brenner (2018) [14].
Continuous Passive Motion (CPM) and Motorized-
cycle ergometers were reviewed.
Results
CPM exercise
-Can significantly reduce physiological symptoms such as oedema, muscle stiffness and/or
spasticity.
-Shoulder joint stability can be increased fol owing 4 weeks of training, 5 × /week/ 25 min
per session (plus warm-up and cool-down)
Motorised-cycle ergometers
-Duration of training programs ranged from 3 to 5 weeks
P a g e |
22
Page 22 of 39

FOI 24/25-0223
Document 15
-Improvements in motor control, trunk stability and cognition were reported fol owing this
type of passive exercise training
-Regular passive arm exercise led to an increase in the range of motion in the affected arm
- No standard protocols or best practice guidelines exist for either modality in stroke
Quality – Low
Smal number of included studies of moderate-low quality. More information is required on
the type of device, the frequency and duration of each exercise session as wel as the
intensity and how long the therapy should be continued (i.e., length of treatment).
1.3.2 FES cycling
1) A high quality systematic review by Shariat et al. (2019) [15] has investigated the
effectiveness of different protocols of cycling with/without FES on functional mobility after
stroke.
Intervention: Cycling with/without FES to the lower limbs
- Frequency: 1 to 7 sessions per week
- Session length: 10 to 90 minutes
- Duration of interventions: 3 to 16 weeks (for cycling alone 3–72 weeks and for
cycling with FES about 4 weeks)
-Total dose of the stimulation: between 4 and 16 hours.
Comparison: cycling alone, cycling with FES, control, placebo, or other interventions
Outcomes: Balance, walking speed, mobility
Study design: Al included studies were RCTs
Results
• Walking speed: Effect size (ES) 0.30 (95% CI, 0.05 – 0.55) P <0.02
• Walking ability: ES 0.41 (95% CI, 0.11 – 0.71) P <0.007
• Cycling vs control on balance: ES 0.32; 95% CI, 0.06 – 0.57, P <0.01
• Cycling with FES vs control on balance: ES 1.48; 95% CI, 0.99 –1.97,
P < 0.00001
Quality – High
-Cycling with FES has a significant and positive effect on balance compared to cycling
without FES
-Additional studies are needed comparing FES cycling directly with other modalities of
exercise such as balance training, strength training, power training or combinations to
determine its relative efficacy
-No outcomes for functional mobility such as fal s and fal -related injuries
2) An additional RCT comparing a standard rehabilitation program to MOTOmed cycle + FES
and found that the intervention and control group both improved on al outcome measures,
however, the intervention group had significantly less shoulder pain. Full summary of the
study by Karaahmet et al. (2018) [16] can be found in Table 3.
P a g e |
23
Page 23 of 39

FOI 24/25-0223
Document 15
Table 3
Author
Study aim
Method/participants
Treatment/Intervention/S Outcome/summary
Quality of evidence
(year) and
characteristics
etting
country
Low/Medium/High
Stroke
Shen et al.
To estimate the
Systematic Review
Duration of MotoMed
The main finding of this systematic review
High
(2018) [13] effectiveness of
therapy:
and meta-analysis is that MOTOmed
MOTOmed®
Only RCTs included (all
- 20 minutes in 11 studies
movement therapy effectively improves
Inclusion of only
movement therapy
performed in China)
- 30 minutes in 6 studies
mobility and activities of daily living in stroke
RCTs. Consistent
in increasing
- 40 minutes in 1
patients with hemiplegia.
findings across all
mobility and
19 Trials including 1099
- Unclear in 1 study
activities of daily
patients
Significant effects in favour of Motomed for:
living in stroke
- 1-2 times per day and 5-7 - Fugl-Meyer Assessment (assess motor
patients with
Stroke with hemiplegia
days per week
functioning, balance, sensation and joint
hemiplegia.
- Lasting 4 to 12 weeks
functioning )
Z = 7.33,
P < 0.0001
Age range 46.5-83.4
All studies compared
-Modified Ashworth Scale (muscle tone)
Z =
conventional
9.19,
P < 0.00001
rehabilitation to MotoMed
+ conventional
-Berg Balance Scale
Z = 8.39,
P < 0.00001
rehabilitation
- Functional Ambulation Category
Z = 9.61,
P
< 0.00001
-10m walk test
Z = 4.49,
P < 0.00001
-Barthel Index (activities of daily living)
Z =
15.6,
P < 0.00001
Brenner
To investigate the
Literature Review
See results/outcomes
CPM exercise
Low
(2018) [14] efficacy and safety
-Can significantly reduce physiological
of passive exercise
1. Continuous Passive Motion
symptoms such as oedema, muscle stiffness
Non-systematic
interventions for
(CPM)
and/or spasticity.
search strategy.
P a g e |
24
Page 24 of 39

FOI 24/25-0223
Document 15
patients with
-Shoulder joint stability can be increased
hemiplegia with a
2. Motorized-cycle
following 4 weeks of training, 5 × /week/ 25
Small number of
focus on those
ergometers
min per session (plus warm-up and cool-
included studies of
interventions that
down)
moderate-low
could be used in the
quality
home setting
Motorised-cycle ergometers
More information is
-Two studies investigated passive leg-cycle
required on the type
and one on arm ergometer exercise on
of device, the
functional measures
frequency and
-Duration of training programs ranged from 3 duration of each
to 5 weeks
exercise session as
-Improvements in motor control, trunk
well as the intensity
stability and cognition were reported
and how long the
following this type of passive exercise training therapy should be
-Regular passive arm exercise led to an
continued (i.e.,
increase in the range of motion in the
length of
affected arm
treatment).
--No adverse effects were reported in the
literature, can perform at home
- No standard protocols or best practice
guidelines exist for either modality in stroke
Shariat et
To quantify the
Systematic Review
Frequency: 1 to 7 sessions Walking speed: ES 0.30 (95% CI, 0.05 – 0.55) P
High
al. (2019)
effectiveness of
per week
<0.02
[15]
different protocols
1. Participants: Human
-Literature suggests
of cycling
subjects post-stroke (Adults
Session length: 10 to 90
that more studies
with/without
≥18 within 5 years after
minutes
Walking ability: ES 0.41 (95% CI, 0.11 – 0.71) P are needed
functional electrical
stroke).
<0.007
comparing FES
stimulation on
2. Intervention: Cycling
Duration of interventions:
cycling directly with
functional mobility
with/without functional
3 to 16 weeks (for cycling
Cycling vs control on balance: ES 0.32; 95% CI, other modalities of
after stroke.
electrical stimulation (FES) to
alone 3–72 weeks and for
0.06 – 0.57, P <0.01
exercise such as
the lower limbs
cycling with FES about 4
balance training,
3. Comparison: cycling alone,
weeks)
Cycling with FES vs control on balance: ES
strength training,
cycling with FES,
1.48; 95% CI, 0.99 –1.97,
P < 0.00001
P a g e |
25
Page 25 of 39

FOI 24/25-0223
Document 15
control, placebo, or other
Total dose of the
power training or
interventions
stimulation between 4 and Long term effects and the most effective
combinations,
4. Outcomes: Balance,
16 hours.
protocols are unclear due to study
to determine its
walking speed, mobility
heterogeneity
relative efficacy
5. Study design:
Randomized
-Electrical stimulation
clinical trial
varied across studies as
-Cycling is superior
the frequency ranged from
to control for
14 trials including 680
20
improving walking
participants who completed
to 60 Hz and pulse width
speed, walking
final fol ow up
from 300 to 450 ms.
ability, and balance.
Mean age 42.5 to 85 years
control intervention
-Cycling with FES has
- 10 studies used sham
a significant and
stimulation
positive effect on
- 4 studies participants
balance compared
received no stimulation
to cycling without
FES.
-Although more
research is needed,
patients post stroke
with lower limb
disability could use
cycling with FES as
part of their
rehabilitation
program.
-No outcomes for
functional mobility
such as falls and fal -
related injuries
Karaahmet To determine the
RCT
-Both groups were trained The only significant finding was that severity
Medium
et al.
effects of FES-cycling
with a standard
of shoulder pain decreased in the FES-cycling
(2018) [16] on shoulder pain and
rehabilitation program
group compared to the control
P a g e |
26
Page 26 of 39

FOI 24/25-0223
Document 15
subluxation, and
-Age between 18 and 80
(range of motion,
Insufficient sample
secondarily to
years, -First stroke
stretching and
All other measures improved significantly
size to observe the
evaluate the
strengthening exercises)
between baseline and post-test for both
effects of FES
improvement of
Exclusion: sensory aphasia,
program
intervention and control groups
training
upper extremity
recurrent stroke or bilateral
-5x a week lasting 30 min
motor function in
hemiplegia, vasomotor
each
patients with
instability, lower motor
-20 sessions
acute–subacute
neuron disorder, limitation/
stroke
instability/dislocation of the
Intervention group
shoulder joints, severe
- Motomed cycle-
spasticity, and uncontrol ed
ergometer used
epilepsy
- Surface electrodes
applied to anterior and the
21 participants (12
posterior deltoid, biceps,
intervention, 9 control)
and triceps muscles
- Pulse width of 300 μs
and a stimulation
frequency of 20 Hz
- 5-min warm-up of
passive cycling, a 15-min
training of FES-cycling, and
a 5-min cool-down of
passive cycling
P a g e |
27
Page 27 of 39

FOI 24/25-0223
Document 15
1.4 Parkinson’s disease
1.4.1 MOTOmed and/or Active Passive Trainer
A literature review summarising the state of the evidence of
forced exercise's impact on
individuals with Parkinson’s disease (PD) has been conducted by Miner et al (2020) [17].
Included studies utilised MOTOmed, Theracycle or a Tandem Bike.
Intervention
- On average, the intervention was delivered;
• 3 times per week
• 5-10 minute warm up at an average pedalling rate of 40-50 rpm
• 30-40 minute forced exercise session (average 80-90 rpm)
• 5-10 minute cool down
• Over 8-12 weeks
Results
Acute effects
- Forced exercise has the potential to cause similar therapeutic effects as antiparkinsonian
medication to improve motor symptoms of PD.
- Last for up to 48hr
Effects on motor function
-Best when used to treat rigidity, bradykinesia, and tremor
Physical fitness
-Muscular strength improved by>30% in the upper and lower body (only one study)
Mobility performance
-difficult to draw conclusions on the effects of forced exercise on mobility performance in
individuals with PD as most of the results were confounded by a ceiling effect in the
outcome measures selected
Incorporating forced exercise as an adjunctive treatment could provide significant added
benefit to task specific training, or gait and balance training for individuals with PD.
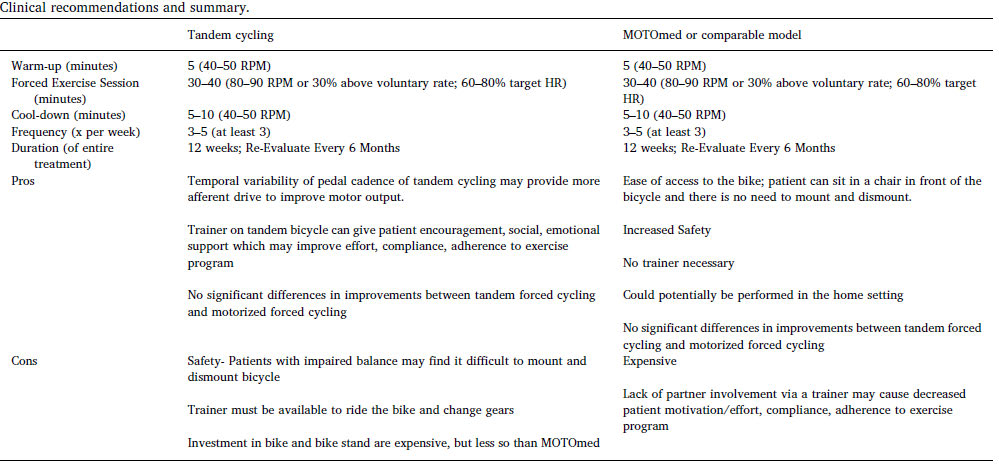
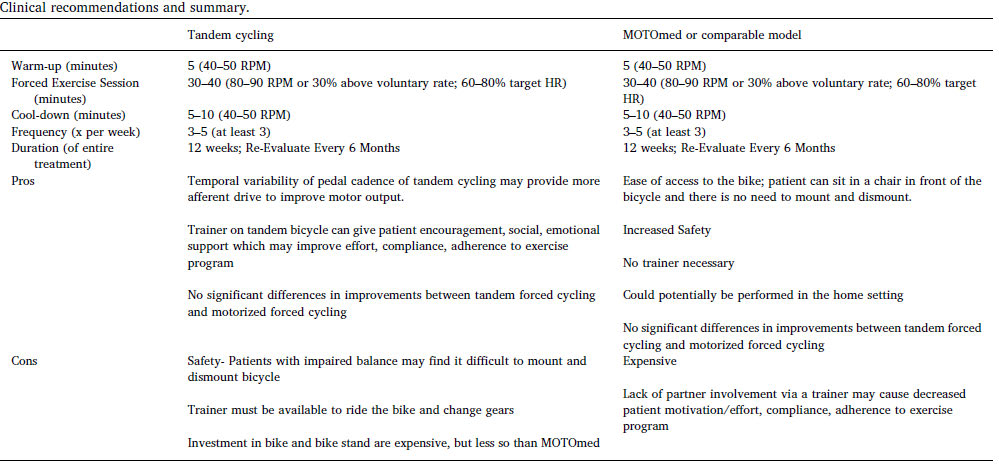
Clinical recommendations summary comparing Tandem cycling to MotoMed (or equivalent)
can be found in Figure 1.
Quality – Moderate
- Various methodological flaws which limit the generalizability
-longer term follow-up studies with larger sample sizes are needed to inform the ability of
forced exercise to alter the trajectory of PD
1.4.2 FES cycling
There is a paucity of research in this area. Findings from a single subject design study [18] can be
found in Table 4. No conclusions can be drawn from the findings provided.
P a g e |
28
Page 28 of 39

FOI 24/25-0223
Document 15
Table 4
Author
Study aim
Method/participants Treatment/Intervention Outcome/summary
Quality of evidence
(year) and
characteristics
/Setting
country
Low/Medium/High
Parkinson’s Disease
Miner at
to summarize the
Review
Treatment frequency
Clinical recommendations summary comparing Tandem
Low
al.(2020)
state of the evidence
- 3 times per week
cycling to MotoMed (or equivalent) can be found in
[17]
of
forced exercise's
Unclear what the
- 5-10 minute warm up
Figure 1 below)
-Small numbers
impact on
search methodology
at an average pedalling
of patients
individuals with PD
was for this review.
rate of 40-50 rpm
Incorporating forced exercise as an adjunctive
- Include studies had
and to determine
No methods section
- 30-40 minute forced
treatment could provide significant added benefit to
various
the utility of this
exercise session (average task specific training, or gait and balance training for
methodological
intervention in the
Single subject, RCT,
80-90 rpm)
individuals with PD.
flaws which limit the
clinical decision
quasi-experimental
- 5-10 minute cool down
generalizability
making for this
-Duration 8-12 weeks
Acute effects
patient population.
MOTOmed
-Forced exercise has the potential to cause similar
-longer term follow-
Theracycle
therapeutic effects as antiparkinsonian medication to
up studies with
Tandem Bike
improve motor symptoms of PD.
larger sample sizes
-Last for up to 48hr
are needed to
inform the ability of
Effects on motor function
forced exercise to
-highlights the importance of individuals being actively
alter the trajectory
engaged in the
of disease
exercise intervention
progression related
-Best when used to treat rigidity,
to motor function
bradykinesia, and tremor
Physical fitness
-Muscular strength improved by>30% in the upper and
lower body (only one study)
P a g e |
29
Page 29 of 39

FOI 24/25-0223
Document 15
Mobility performance
-difficult to draw conclusions on the effects of forced
exercise on
mobility performance in individuals with PD as most of
the results were
confounded by a ceiling effect in the outcome measures
selected
Bellman et provides the results
Case study
Device
Results suggest that FES-assisted cycling using the
Very Low
al. (2016)
of an experiment
-stationary, recumbent
developed switched control er may improve the ability
[18]
conducted with one
Four able-bodied
exercise cycle
of people with PD to track a desired cadence
Only one participant
subject with PD to
male subjects 25–27
(AudioRider R400,
with PD. Only
establish feasibility
years old were
NordicTrack)
outcome measure is
of FES-assisted
recruited
cadence
cycling in this
from the University
Stimulation
population
of Florida,
-Frequency was fixed at
Significant
and one male subject 60 Hz
additional testing
with PD, 60 years old,
beyond the scope of
with a modified
Gluteal, quadriceps
this paper is needed
Hoehn and Yahr
femoris, and hamstrings
to determine clinical
disability score of 2.5
muscle groups
efficacy.
stimulated
P a g e |
30
Page 30 of 39

FOI 24/25-0223
Document 15
P a g e |
31
Page 31 of 39

FOI 24/25-0223
Document 15
1.5 Cerebral Palsy
1.5.1 MOTOmed and/or Active Passive Trainer
A single high quality, well powered RCT has been conducted by Damiano et al. (2017) [19].
The aim was to quantify and compare the effectiveness of a motor-assisted cycle
(MOTOmed) and a novel alternative (elliptical), in cerebral palsy (CP) to improve inter-limb
reciprocal coordination.
Intervention
Devices were randomised to participants and delivered to their homes
-Instructed to exercise above 40 rpm for 20 minutes, 5 days a week for 12 weeks.
Results
-Device cadence at self-selected and fast speeds for all participants improved markedly and
significantly as a result of training
-No significant changes were seen in gait speed for time or group, nor did parent-reported
functional mobility
-Knee extensor strength increased in both
Quality – Medium
Single study but excel ent sample size with positive findings. Training dose provided likely
insufficient for maximum results.
1.5.2 FES cycling
Several case studies and pilot work has been conducted on the feasibility and benefits of FES cycling
in CP [20-22].
Intervention
• Duration: most commonly used 30 minutes at a time for 3 times a week
• FES applied to the bilateral quadriceps and/or hamstrings
• One delivered intervention in the participants home [22]
Results
• Positive results for Modified Ashworth scale (MAS), cadence, power output, and
heart rates, quadriceps and hamstring strength, Timed “Up & Go” .
• Participants were able to tolerate the application of FES and complete testing
Quality – Low to Very Low
No control groups. Very smal sample (total of 5 participants).
1.5.3 Conventional Exercise Training Programs
The impact of resistance training on the motor functions of children with CP has been investigated in
a systematic review and meta-analysis by Collado-Garrido et al (2019) [23].
P a g e |
32
Page 32 of 39

FOI 24/25-0223
Document 15
Outcome measures
• Gross Motor Function Measure
• Lateral Step Up
• Time Up and Go
• Mobility Questionnaire
Results
• Large effect of 0.75 (95% CI 0.41-1.08) for duration ≤6 weeks compared to 7-12
weeks
• Large effect of 1.08 (95% CI = 0.52 to 1.64) when duration was less than 30 minutes
compared to 30-60 minutes and 60-90 minutes
• Large effect for fewer than three days a week. 1.59 (95% CI = 0.67 to 2.50),
compared to studies with sessions applied three days a week
• Larger effect when using the “functional exercises” protocol. 1.25 (95% CI = 0.46 to
2.04)
Quality – High
Majority RCT of high quality. Statistically significant positive effect on motor function in
favour of the use of resistance therapy in weakened musculature in children with CP
P a g e |
33
Page 33 of 39

FOI 24/25-0223
Document 15
Table 5
Author
Study aim
Method/
Treatment/
Outcome/summary
Quality of
(year) and
participants
Intervention/
evidence
country
characteristics
Setting
Low/Medium
/High
Cerebral Palsy
Damiano et To quantify and
RCT
assigned device
Device cadence at self-selected and fast speeds for all participants,
Medium
al. (2017)
compare
was delivered
improved markedly and significantly as a result of
[19]
effectiveness of a
27 children with to their home, and
training
Single study
motor-assisted cycle bilateral spastic they were
and a novel
CP, and a mean instructed to
No significant changes were seen
Positive across
alternative, an
age of 10.3
exercise above
in gait speed for time or group, nor did parent-reported functional
both groups
elliptical, in CP to
years
40 rpm for 20
mobility
improve inter-limb
minutes, 5 days a
Training dose is
reciprocal
Reached power week for 12 weeks. Knee extensor strength increased in both
insufficient
coordination
through intensive
MOTOMed
Each participant
speed-focused leg
was tested 3 times
training.
Elliptical
at 3-month
intervals,
Peng et al.
Review FES cycling
Case study
-FES sequentially
-Preliminary results showed all measured MAS scores decreased after
Very low
(2010) [20] system; the
applied to the
FES cycling
therapeutic benefits 3 children with
bilateral quadriceps
The results
of FESCE in subjects
quadriplegic CP and hamstrings to
implied that FES
with SCI; clinical
(mean age 3
achieve a rhythmic
cycling might
efficacy of FES in
years)
pedaling motion.
acutely alleviate
subjects with stroke;
-30 minutes, 3x per
spastic
a pilot study of
week
conditions of
FESCE in subjects
-Exercise protocol
children with CP.
with cerebral palsy
based on the
muscle status of
Will only review CP
their lower limbs
case
P a g e |
34
Page 34 of 39

FOI 24/25-0223
Document 15
-Gradual increase in
load
-Modified
Ashworth scale
(MAS), leg drop
pendulum test, and
myotonometric
measurements
were conducted
pre and post-test
Harrington to adapt methods
Pilot study
-Bilateral
-All participants were able to tolerate the application of FES and
Low
et al.
and assess the
quadriceps muscles complete testing
(2012) [21] feasibility of
four
were stimulated
applying FES cycling
participants
during the limb
-FES-assisted cycling resulted in increased cadence, power output, and
technology in
(2 male) with
extension phase of heart rates and decreased variability in cycling performance compared
adolescents
spastic CP
the cycling
with volitional cycling without FES assistance.
with CP, determine
between the
methods of
ages of 12–14
-2–4 sessions with
performing cycling
years
at least 24 hours
tests in adolescents
(mean 13
± 1.2
of rest between
with CP, and
years)
cycling sessions and
evaluate the
with all testing
immediate effects of tricycle-based
occurring within a
FES assistance on
system (a sport two-week period
cycling performance. tricycle
for each participant
(KMXKarts;
United
-Target for the
Kingdom)
constant load test
mounted on a
was set at 80% of
cycle trainer
the peak power
output
P a g e |
35
Page 35 of 39

FOI 24/25-0223
Document 15
Johnston et describes the effects
Mixed methods -Cycled with FES at -Quadriceps muscle strength improved by 22.2%
Very low
al. (2011)
of cycling with FES
case report
home for 30
[22]
(FES cycling) in an
minutes, 3 times
-Hamstring muscle strength improved by 18.5%,
Single case study
adult
49-year-old
per week, for 12
with CP.
man with
weeks
-Timed “Up & Go” Test time decreased from 11.9 to 9.0 seconds
Patient made
spastic diplegic
gains in body
CP
Volitional efforts
-Patient reported increased performance and satisfaction for self-
structure and
were augmented
identified goals and his score on the Medical Outcomes Study 36-Item function, activity,
by FES of the
Health Survey questionnaire increased from 62.1 to 77.6.
and participation
bilateral
quadriceps,
-Reported increased back pain
gastrocnemius, and
gluteal muscles.
Tested 4 weeks
after withdrawal
Collado-
To analyse, through
Systematic
“progressive
Intervention duration
High
Garrido et
a meta-analysis of
Review and
strength training”
-Large effect of 0.75 (95% CI 0.41-1.08) for duration ≤6 weeks
al. (2019)
published primary
Meta-Analysis
compared to 7-12 weeks
statistically
[23]
studies, the impact
functional
significant
of resistance therapy Controlled
training
-Large effect of 1.08 (95% CI = 0.52 to 1.64) when duration was less
positive effect on
Related to
on the parameters
(randomized or
than 30 minutes compared to 30-60 minutes and 60-90 minutes
motor function
resistance
of the motor
quasi-
static bicycle
in favour of the
training but function in children
randomized)
-Large effect for fewer than three days a week. 1.59 (95% CI = 0.67 to
use of resistance
not specific with CP
and non-
outcome measure
2.50), compared to studies with sessions applied three days a week
therapy in
to
controlled
-Gross Motor
weakened
Motomed,
clinical trials
Function Measure
-larger effect when using the “functional exercises” protocol with an
musculature in
APT, FES
- Lateral Step Up
SMD of 1.25 (95% CI = 0.46 to 2.04)
children with CP
cycling etc.
Intervention
-Time Up and Go
based on
-Mobility
resistance
Questionnaire
therapy
School-aged CP
patients (≤18
years)
P a g e |
36
Page 36 of 39

FOI 24/25-0223
Document 15
12 RCT and 3
non-
randomised
clinical trials
electrostimulati
on as resistance
therapy
P a g e |
37
Page 37 of 39

FOI 24/25-0223
Document 15
Reference List
1. Hochsprung A, Domínguez AG, Magni E, Uribe SE, García AM. Effect of visual
biofeedback cycling training on gait in patients with multiple sclerosis. Neurología
(English Edition). 2019 Apr 8.
2. Barclay A, Paul L, MacFarlane N, McFadyen AK. The effect of cycling using active-
passive trainers on spasticity, cardiovascular fitness, function and quality of life in
people with moderate to severe Multiple Sclerosis (MS); a feasibility study. Multiple
sclerosis and related disorders. 2019 Sep 1;34:128-34.
3. Scally JB, Baker JS, Rankin J, Renfrew L, Sculthorpe N. Evaluating functional electrical
stimulation (FES) cycling on cardiovascular, musculoskeletal and functional outcomes
in adults with multiple sclerosis and mobility impairment: A systematic review.
Multiple sclerosis and related disorders. 2020 Jan 1;37:101485.
4. Pilutti LA, Motl RW. Functional Electrical Stimulation Cycling Exercise for People with
Multiple Sclerosis. Current treatment options in neurology. 2019 Nov 1;21(11):54.
5. Latimer-Cheung AE, Pilutti LA, Hicks AL, Ginis KA, Fenuta AM, MacKibbon KA, Motl
RW. Effects of exercise training on fitness, mobility, fatigue, and health-related
quality of life among adults with multiple sclerosis: a systematic review to inform
guideline development. Archives of physical medicine and rehabilitation. 2013 Sep
1;94(9):1800-28.
6. Edwards T, Pilutti LA. The effect of exercise training in adults with multiple sclerosis
with severe mobility disability: a systematic review and future research directions.
Multiple sclerosis and related disorders. 2017 Aug 1;16:31-9.
7. Pilutti LA, Motl RW. Functional Electrical Stimulation Cycling Exercise for People with
Multiple Sclerosis. Current treatment options in neurology. 2019 Nov 1;21(11):54.
8. Alashram AR, Annino G, Mercuri NB. Changes in spasticity following functional
electrical stimulation cycling in patients with spinal cord injury: A systematic review.
The Journal of Spinal Cord Medicine. 2020 May 15:1-4.
9. Thomaz SR, Cipriano Jr G, Formiga MF, Fachin-Martins E, Cipriano GF, Martins WR,
Cahalin LP. Effect of electrical stimulation on muscle atrophy and spasticity in
patients with spinal cord injury–a systematic review with meta-analysis. Spinal cord.
2019 Apr;57(4):258-66.
10. Deley G, Denuziller J, Babault N. Functional electrical stimulation: cardiorespiratory
adaptations and applications for training in paraplegia. Sports Medicine. 2015 Jan
1;45(1):71-82.
11. Mayson TA, Harris SR. Functional electrical stimulation cycling in youth with spinal
cord injury: A review of intervention studies. The journal of spinal cord medicine.
2014 May 1;37(3):266-77.
12. Hicks AL, Ginis KM, Pelletier CA, Ditor DS, Foulon B, Wolfe DL. The effects of exercise
training on physical capacity, strength, body composition and functional
performance among adults with spinal cord injury: a systematic review. Spinal cord.
2011 Nov;49(11):1103-27.
P a g e |
38
Page 38 of 39

FOI 24/25-0223
Document 15
13. Shen C, Liu F, Yao L, Li Z, Qiu L, Fang S. Effects of MOTOmed movement therapy on
the mobility and activities of daily living of stroke patients with hemiplegia: a
systematic review and meta-analysis. Clinical rehabilitation. 2018 Dec;32(12):1569-
80.
14. Brenner I. Effects of Passive Exercise Training in Hemiplegic Stroke Patients: A Mini-
Review. Sports Med Rehabil J. 2018; 3 (3). 2018;1036.
15. Shariat A, Najafabadi MG, Ansari NN, Cleland JA, Singh MA, Memari AH, Honarpishe
R, Hakakzadeh A, Ghaffari MS, Naghdi S. The effects of cycling with and without
functional electrical stimulation on lower limb dysfunction in patients post-stroke: a
systematic review with meta-analysis. NeuroRehabilitation. 2019 Jan 1;44(3):389-
412.
16. Karaahmet OZ, Gurcay E, Unal ZK, Cankurtaran D, Cakci A. Effects of functional
electrical stimulation-cycling on shoulder pain and subluxation in patients with
acute–subacute stroke: a pilot study. International Journal of Rehabilitation
Research. 2019 Mar 1;42(1):36-40.
17. Miner DG, Aron A, DiSalvo E. Therapeutic effects of forced exercise cycling in
individuals with Parkinson's disease. Journal of the Neurological Sciences. 2020 Jan
9:116677.
18. Bel man MJ, Cheng TH, Downey RJ, Hass CJ, Dixon WE. Switched control of cadence
during stationary cycling induced by functional electrical stimulation. IEEE
Transactions on Neural Systems and Rehabilitation Engineering. 2015 Nov
13;24(12):1373-83.
19. Damiano DL, Stanley CJ, Ohlrich L, Alter KE. Task-specific and functional effects of
speed-focused elliptical or motor-assisted cycle training in children with bilateral
cerebral palsy: randomized clinical trial. Neurorehabilitation and neural repair. 2017
Aug;31(8):736-45.
20. Peng CW, Chen SC, Lai CH, Chen CJ, Chen CC, Mizrahi J, Handa Y. Clinical benefits of
functional electrical stimulation cycling exercise for subjects with central
neurological impairments. J. Med. Biol. Eng. 2011 Jan 1;31(1):1-1.
21. Harrington AT, McRae CG, Lee SC. Evaluation of functional electrical stimulation to
assist cycling in four adolescents with spastic cerebral palsy. International journal of
pediatrics. 2012 May 22;2012.
22. Johnston TE, Wainwright SF. Cycling with functional electrical stimulation in an adult
with spastic diplegic cerebral palsy. Physical Therapy. 2011 Jun 1;91(6):970-82.
23. Collado-Garrido L, Parás-Bravo P, Calvo-Martín P, Santibáñez-Margüel o M. Impact of
Resistance Therapy on Motor Function in Children with Cerebral Palsy: A Systematic
Review and Meta-Analysis. International journal of environmental research and
public health. 2019 Jan;16(22):4513.
P a g e |
39
Page 39 of 39