FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
Physiotherapy and exercise for progressive
neurological conditions
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research questions: What is considered best practice for the frequency and duration of physiotherapy and
exercise physiology for progressive neurological conditions?
Are there any contraindications for use of a delegated care model for these supports with
this population (e.g. using therapy assistants)?
What are the risks and contraindications of physiotherapy and exercise physiology based on
disease progression with these populations (i.e. is there a time when hands on therapy
should not be provided as risks outweigh benefits)?
Date: 29/4/2024
Requestor: s47F - personal privacy
Endorsed by: Shannon A
s47F - persona
Researcher: Aaron Hs47F - personal priva
Cleared by: Aaron Hs47F - personal priva
Physio and exercise for progressive conditions
Page 1 of 14
OFFICIAL
Page 1 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
1. Contents
Physiotherapy and Exercise physiology for progressive neurological conditions ....................... 1
1.
Contents ....................................................................................................................... 2
2.
Summary ...................................................................................................................... 3
3.
Previous TAPIB research .............................................................................................. 3
4.
Therapy assistants ........................................................................................................ 4
5.
Amyotrophic lateral sclerosis / motor neuron disease ................................................... 5
5.1 Frequency and duration ............................................................................................. 5
5.2 Risks .......................................................................................................................... 5
5.3 Stage of progression .................................................................................................. 5
6.
Parkinson’s Disease ..................................................................................................... 6
6.1 Frequency and duration ............................................................................................. 6
6.2 Risks .......................................................................................................................... 7
6.3 Stage of progression .................................................................................................. 8
7.
Multiple Sclerosis .......................................................................................................... 8
7.1 Frequency and duration ............................................................................................. 8
7.2 Risks .......................................................................................................................... 9
7.3 Stage of progression ................................................................................................ 10
8.
Muscular dystrophy ..................................................................................................... 10
8.1 Frequency and duration ........................................................................................... 10
8.2 Risks ........................................................................................................................ 11
8.3 Stage of progression ................................................................................................ 11
9.
References ................................................................................................................. 11
Physio and exercise for progressive conditions
Page 2 of 14
OFFICIAL
Page 2 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
2. Summary
This paper considers the use of physiotherapy and exercise interventions for people with
progressive neurological conditions including amyotrophic lateral sclerosis (ALS) and motor
neuron disease (MND), Parkinson’s disease (PD), multiple sclerosis (MS), and muscular
dystrophy (MD). This paper focusses on evidence of optimal frequency and duration of
physiotherapy and exercise interventions, risks associated with interventions, differing care for
early or late stages of progression and the use of therapy assistants through a delegated care
model.
No studies were found that address the role of therapy assistants in the delivery of
physiotherapy or exercise interventions for people with progressive neurological conditions.
Some evidence suggests that the use of therapy assistants in acute hospital settings and
general community settings is safe and effective. This evidence is uncertain and further
research is required.
There is limited evidence regarding optimal dosage of physiotherapy and exercise
interventions for people with progressive neurological conditions. Clinical practice guidelines
for PD and MS provided recommendations for frequency and duration of physiotherapy and
exercise interventions. However, it is likely that these recommendations are based primarily on
clinical judgement rather than published evidence. One 2023 systematic review was able to
determine that at least twice weekly sessions of more than 40 minutes is an effective dose of
exercise intervention for the improvement of balance in MS (Corrini et al, 2023). No other
studies could provide evidence-based dosage recommendations.
Where evidence is not clear, guidelines generally recommend that type, frequency, duration
and intensity of physiotherapy or exercise interventions should be determined individually
based on the needs and preferences of the person receiving treatment.
Despite some issues with the proper reporting of adverse events in experimental studies,
exercise interventions for people with progressive neurological conditions are generally
believed to be safe, provided that standard safety precautions are observed.
There is little evidence regarding safety and effectiveness of physiotherapy and exercise
interventions for people at late stages of progressive neurological conditions. Most research
focusses on people with mild to moderate symptom severity.
3. Previous TAPIB research
Other relevant TAPIB research papers include:
• RES 322 Manual therapy to address neuromusculoskeletal function
• RES 321 Osteopathy
• RES 318 Exercise physiology and stroke
• RES 289 Lokomat Therapy
Physio and exercise for progressive conditions
Page 3 of 14
OFFICIAL
Page 3 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
• RES 264 Chiropractic
• RES 233 Virtual reality as a support tool
• RES 191 Massage Therapy as a Treatment for Multiple Sclerosis
4. Therapy assistants
Therapy assistants are
support staff who complete clinical and non-clinical tasks under the supervision and
delegation of an allied health professional. Clinical tasks include any direct therapeutic
interventions provided to patients such as exercise therapy and education, while non-
clinical tasks may include administration duties (eg, completing paperwork for
equipment hire), maintenance of equipment and cleaning the clinical environment.
Because al ied health assistants cannot perform clinical tasks that involve diagnosing or
assessing patient health conditions, allied health professionals must perform a
comprehensive assessment of the patient and prescribe appropriate therapy prior to
delegating the allied health assistant to perform any clinical tasks. (Snowdon et al, 2024,
p.2).
In a survey of 232 UK-based physiotherapists, 81% of respondents indicated that they at least
sometimes delegate the supervision of prescribed exercises to therapy assistants
(Sarigiovannis et al, 2022). The authors also found that delegation of clinical tasks to therapy
assistants was more likely in less complex cases where there is a straightforward treatment
plan. There is a perception that increased reliance on therapy assistants may compromise the
quality or safety of the intervention (Snowdon et al, 2024). However, existing evidence
suggests that physiotherapy or exercise interventions delivered by a therapy assistant are
likely safe (Lau et al, 2024; Snowdon et al, 2020).
No studies were found that address the role of therapy assistants in the delivery of
physiotherapy or exercise interventions for people with progressive neurological conditions.
Where there is minimal research to date, there is a growing interest in the role of therapy
assistants in completing clinical physiotherapy tasks (Snowdon et al, 2024; Sarigiovannis et al,
2023). Current research mostly considers the addition of therapy assistants to usual care
rather than a model where physiotherapy or exercise interventions are primarily delivered by a
therapy assistant (Snowdon et al, 2024; Lau et al, 2024; Snowdon et al, 2020). Some evidence
points to the efficacy and safety of physiotherapy or exercise interventions delivered by
therapy assistants. Additional supervised exercise sessions may improve outcomes regardless
of whether it is delivered by a physiotherapist or therapy assistant (Snowdon et al, 2024; Lau
et al, 2024; Baumann et al, 2023a-b; Sarigiovannis et al, 2023; Sarigiovannis et al, 2022;
Sarigiovannis et al, 2021). Much of the research is based in a hospital setting and the roles of
physiotherapist and therapy assistant are frequently poorly reported, so results may not
generalise across all models of therapy assistance or patient cohorts (Sarigiovannis et al,
2021; Snowdon et al, 2020).
Physio and exercise for progressive conditions
Page 4 of 14
OFFICIAL
Page 4 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
5. Amyotrophic lateral sclerosis / motor neuron disease
5.1 Frequency and duration
We did not find any reviews able to determine optimal frequency or duration of exercise or
physiotherapy interventions for people with ALS/MND. One review (Zhou et al, 2022) showed
inconsistent evidence that more intensive exercise training could slow the decline in functional
capacity. However, the authors do not specify what they mean by ‘intensive’.
A 2023 meta-analysis including 17 studies was unable to determine optimal exercise dosage
due to the variability of intervention: “frequency ranged from 2×/week to 3×/day, up to 7
days/week, with repetitions of sets ranging from 20 to 25, intensity ranging from 30 to 60% of a
patient’s maximum value, and treatment duration ranging from 2 weeks to 2 years” (Donohue
et al, 2023, p.19). Meng et al (2020) and Papadopolou et al (2024) were similarly unable to
determine the most effective frequency, intensity, type, timing or duration of exercise-based
interventions.
5.2 Risks
Researchers report some reluctance to prescribe exercise for people with ALS/MND due to
possibility that exercise might lead to fatigue and faster progression of symptoms (MND
Australia, 2021). However, recent reviews have found no serious adverse events in studies of
exercise or physiotherapy intervention for people with ALS/MND (Papadopolou et al, 2024;
Donohue et al, 2023; Meng et al, 2020). Researchers suggest that physiotherapy or exercise-
based interventions are likely safe for people with ALS/MND.
5.3 Stage of progression
Minimal evidence is available for the efficacy of physiotherapy or exercise programs for people
with more advanced ALS/MND. Donahue et al (2023) find some low certainty evidence that
exercise programs are beneficial in early stages of disease progression. However, all of the
studies included in their review explore exercise intervention only on those with low to
moderate symptom severity.
Ireland’s
Guidelines for the physiotherapy management of Motor Neuron Disease (O’Callaghan, 2014), suggests physiotherapy treatment plans differentiate early, middle and
late stages of progression. During the late stage, strategies to maintain function and manage
symptoms may include:
• a stretching program
• active and passive range of movement exercises
• the use of assistive technology such as motomed or tilt table.
Physio and exercise for progressive conditions
Page 5 of 14
OFFICIAL
Page 5 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
While evidence is presented for the efficacy of exercise at the early stages of MND,
recommendations for strategies at the middle and late stages are based on clinical judgment
of the authors.
6. Parkinson’s Disease
6.1 Frequency and duration
There is no consensus on optimal frequency or duration of physiotherapy or exercise
interventions for people with Parkinson’s disease. Reviews report average frequency and
duration of interventions used in studies but are unable to determine best practice timing
(Ernst et al, 2024; El Hayek et al, 2023; Osborne et al, 2022; Grimes et al, 2019; NICE, 2017;
Keus et al, 2014).
El Hayek et al (2023) reviewed 46 studies to determine most effective types, timing, frequency,
duration, and outcomes of physiotherapy and exercise for people with Parkinson’s disease.
They found no significant difference between interventions and comparisons for frequency,
duration or number of sessions.
A 2024 Cochrane review of studies on exercise intervention for people with Parkinson’s
disease was unable to draw conclusions regarding the optimal frequency of exercise
intervention (Ernst et al ,2024). The authors observed a beneficial effect on functional mobility
and balance in studies lasting longer than 12 weeks. However, they did not observe a
significant effect of intervention duration on other outcomes.
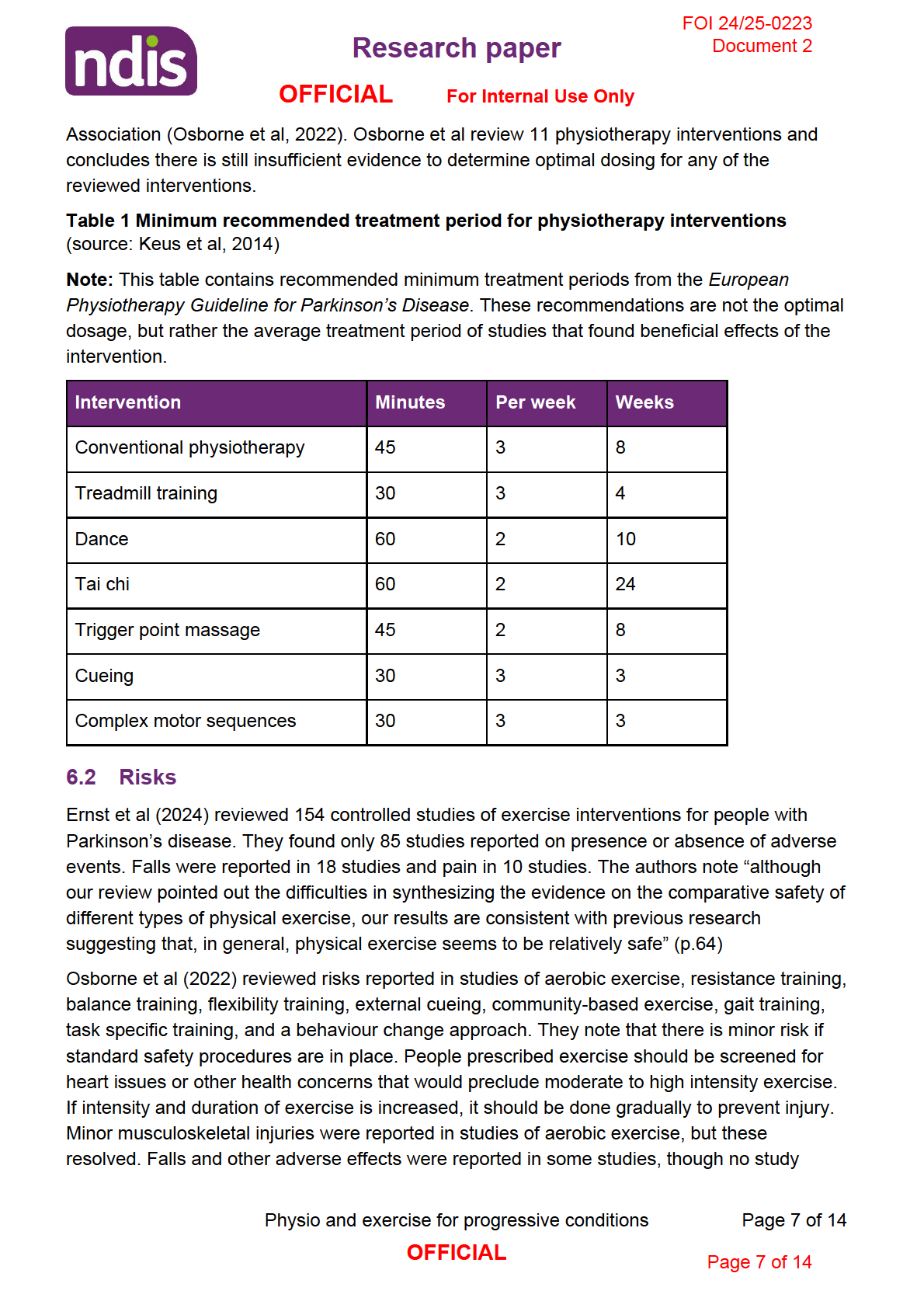
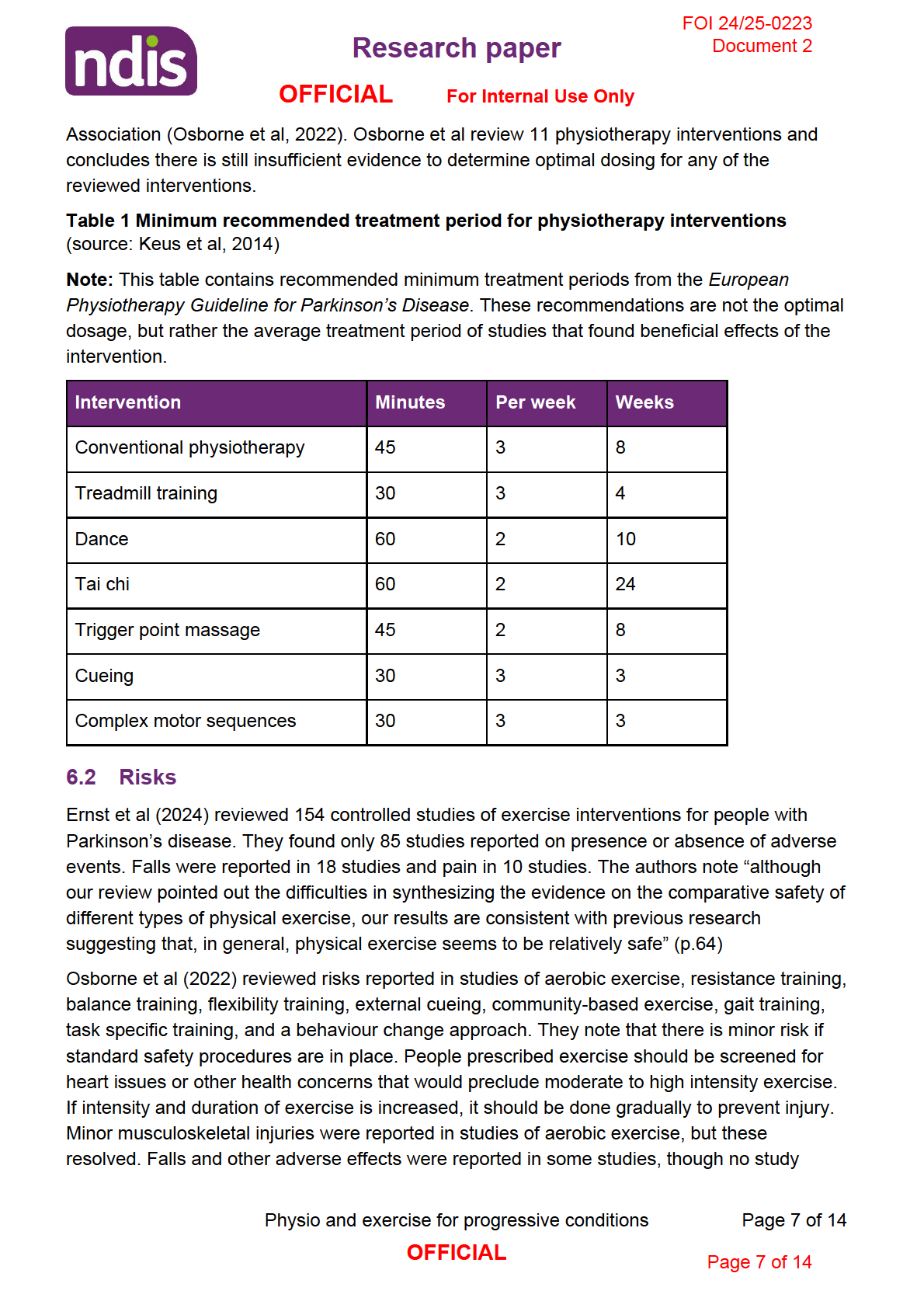
Of four clinical practice guidelines that recommend the use of physiotherapy, exercise or
physical activity for people with Parkinson’s disease, only one provides recommendations
regarding frequency and duration of activity (Osborne et al, 2022; Grimes et al, 2019; NICE,
2017; Keus et al, 2014). The
European Physiotherapy Guideline for Parkinson’s Disease (Keus et al, 2014) includes recommendations for minimum treatment period for seven
physiotherapy modalities (refer to Table 1). However, the Guideline Development Group
(GDG) responsible for the recommendations also note:
Evidence-based information on the optimal number of sessions a week, session time
and length of a treatment period are unavailable. These decisions wil depend on the
treatment goal, the selected intervention, the potential of the [person with Parkinson’s
disease] and the response to the treatment. GDG recommendations for minimum
treatment period, frequency and session duration for each intervention category
provided in this chapter are based on the averages of controlled clinical trials (CCTs)
supportive to the ‘for’ recommendations (Keus et al, 2014, p.64)
Further, the GDG suggests that the optimal treatment period, duration and intensity will most
likely never be determined due to the varied fitness levels, functional capacity and preferences
of people with Parkinson’s disease (Keus et al, 2014, p.72). This judgement is implicitly
supported by the most recent clinical guideline from the American Physical Therapy
Physio and exercise for progressive conditions
Page 6 of 14
OFFICIAL
Page 6 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
reported a more significant rate of adverse effects in the intervention group compared to the
control group.
6.3 Stage of progression
Li et al (2023) suggest that exercise interventions are beneficial for people at advanced stages
of Parkinson’s disease to maintain function and health. However, this suggestion was not
based on the results of their review, which found no evidence that exercise could limit
progression of symptoms for people at advanced stages.
Other reviews have also been unable to determine whether exercise interventions are effective
or safe for people at advanced at stages of Parkinson’s progression (stages 4 or 5 of the
Hoehn & Yahr scale). Ernst et al (2024) reviewed 154 studies and found most studies included
participants at stages 1 – 3. No studies included participants at stage 5, while only 17 studies
included participants at stage 4. Therefore, the authors note that their results may not apply to
people at advanced stages of Parkinson’s disease progression.
For most physiotherapy interventions reviewed by Osborne et al (2022), studies supporting the
intervention focussed on mostly those with mild to moderate symptoms covering Hoehn &
Yahr stages 1 to 3. Studies investigating external cueing and resistance, balance and flexibility
training included participants at stages 1 to 4. None of the recommendations made by
Osborne et al are relevant to people showing advanced stage 5 symptoms.
7. Multiple Sclerosis
7.1 Frequency and duration
A 2019 systematic review of clinical practice guidelines for exercise interventions for people
with Multiple Sclerosis found consistent dosage recommendations for aerobic and resistance
training:
The literature we summarized consistently indicated that moderate-intensity aerobic
training should be performed 2 to 3 days per week in 10- to 40-minute bouts. By
achieving these guidelines, people with MS can potentially improve their cardiovascular
fitness, mobility and symptoms of fatigue and depression. This should be complemented
by 2 to 3 days of weekly resistance training, from which anticipated benefits could
include: improved strength, balance, mobility, performance of activities of daily living,
and symptoms of fatigue (Kim et al, 2019, p.9).
These recommendations may be based on a combination of experimental evidence and
clinical judgement. However, considering the difficulty of deriving optimal dosage levels from
the current evidence, it is likely that the recommendations in Kim et al represent a professional
consensus rather than an evidence-based conclusion (Taul-Madsen et al, 2021; Edwards &
Pilutti, 2017).
Physio and exercise for progressive conditions
Page 8 of 14
OFFICIAL
Page 8 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
Corrini et al (2023) reviewed 20 randomised controlled trials looking at the effect of balance
training programs for people with Multiple Sclerosis. They found high quality evidence that
physiotherapy targeting balance has a moderate effect on improving balance as measured by
the Berg Balance Scale. In addition, their meta-analysis was able to show that sessions lasting
40 minutes or longer produced a significant and clinically meaningful improvement in balance
scores, while sessions lasting under 40 minutes did not produce statistically significant results.
The authors concluded that:
intense treatments lasting at least 40 [minutes] were associated with a better and more
clinically meaningful improvement, and greater results can be reached when
rehabilitation is provided over a short period (duration) and for a few sessions per week
(frequency) (Corrini et al, 2023, p.20).
7.2 Risks
Learmonth et al (2023) searched for information on relapse and adverse events after exercise
interventions for people with Multiple Sclerosis. They reviewed 40 randomised controlled trials
including 1780 participants. The authors found no significant difference in adverse events
between exercise intervention and comparison groups. The analysis
did not reveal any significant variability in risk of exercise training across the potentially
important factors of exercise type, delivery style (e.g. supervised, independent or
remotely supervised), participant disability level or the prescription of exercise consistent
with minimal exercise guidelines for persons with MS (Learmonth, 2023, p.1624).
While exercise interventions are generally considered safe for people with Multiple Sclerosis,
safety precautions and modifications may be required depending on the needs of the
individual. A 2019 systematic review of guidelines produced the following advice:
An exercise prescription for people with MS should promote a safe and individualized
exercise regimen. Thus, before prescribing an exercise routine, MS specific
symptoms/characteristics (i.e., fatigue and heat sensitivity) should be identified and
discussed, and the exercise prescription should include appropriate modifications. For
example, individuals with high heat sensitivity should exercise in a cool environment,
and a cooling fan should be readily available for the person during the exercise
sessions. When individuals experience symptom exacerbation, either daily variation in
symptoms or relapse, the exercise program may require modification or be temporarily
discontinued until the symptoms are stable. Risk of falling should be considered for
individuals with MS, and individuals with high risk of falls should perform both aerobic
and strength exercises in a seated position (e.g., recumbent bike, weight machines) and
under supervision (Kim et al, 2019, p.6)
Physio and exercise for progressive conditions
Page 9 of 14
OFFICIAL
Page 9 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
7.3 Stage of progression
Learmonth et al (2023) did not find any significant difference in risk or safety of exercise
interventions between levels of disability. However, it should also be noted that participants
with advanced stages of MS were minimally represented in the studies reviewed. Of 40
randomised controlled trials, only 3 were focussed on people with severe symptoms of Multiple
Sclerosis. In fact, most evidence for the efficacy of exercise intervention for people with
Multiple Sclerosis lacks generalisability for people with severe symptoms (Corrini et al, 2023;
Taul-Madsen et al, 2021; Kim et al, 2019; Edwards & Pilutti, 2017).
Two systematic reviews have examined the effectiveness of physiotherapy or exercise
interventions in people with Multiple Sclerosis (Binshalan et al, 2022; Edwards & Pilutti, 2017).
A 2017 review found limited and very low certainty evidence that exercise interventions could
improve fitness, function, balance, fatigue, mood and quality of life (Edwards & Pilutti, 2017).
The authors also suggest exercise interventions are safe for people with severe symptoms.
More recently, Binshalan et al (2022) found low quality evidence that robot assisted gait
therapy may be effective at improving walking speed and endurance in people with severe
symptoms of Multiple Sclerosis. The authors speculate on possible reasons robot assisted gait
therapy may be more effective than other modes of physiotherapy or exercise intervention:
Appropriate PT intervention programs must be tailored to the patient’s abilities with
sufficient stimulus to push present competence to produce effect [49]. Therefore, it
possible that RAGT is less demanding for severely disabled pwMS, who might not be
able to complete other forms of PT effectively (p.13).
8. Muscular dystrophy
8.1 Frequency and duration
Hammer et al (2022) is the most recent systematic review of physiotherapy or exercise
interventions for people with muscular dystrophy. They reviewed 12 studies with 282
participants and found exercise intervention may improve strength and endurance for people
with MD. No conclusions regarding frequency, duration or intensity were possible with the
available evidence.
A 2019 Cochrane review of exercise training in muscle disease (including MD), notes:
The most effective dose of exercise for people with muscle diseases is currently
unknown, making it difficult to prescribe exercise in this population. This is reflected in
the large variation in the frequency, duration and intensity of exercise prescribed (Voet
et al, 2019, p.42).
Physio and exercise for progressive conditions
Page 10 of 14
OFFICIAL
Page 10 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
8.2 Risks
The most recent review of physiotherapy or exercise interventions for MD noted that none of
the studies included in the review adequately reported on adverse events. However, the
authors noted that “intensive eccentric muscle exercise, where the muscle is both activated
and lengthened, in addition to high-resistance exercise, may exacerbate muscle damage and
should be avoided” (Hammer et al, 2022, p.2).
Voet et al (2019) report no evidence of safety concerns in appropriately structured exercise
programmes, though they also note that “included studies were small and the evidence was
largely low or low certainty; therefore, we can make no definitive statements regarding safety”
(p.42).
8.3 Stage of progression
No studies were able to discriminate benefits or risks of exercise based on severity of
symptoms or stage of progression.
9. References
Binshalan, T., Nair, K. P. S., & McNeil , A. (2022). The Effectiveness of Physiotherapy
Interventions for Mobility in Severe Multiple Sclerosis: A Systematic Review and Meta-
Analysis.
Multiple sclerosis international, 2022, 2357785.
https://doi.org/10.1155/2022/2357785
Baumann, A. N., Curtis, D. P., Chen, M., & Baldwin, K. D. (2023a). The Impact of the Addition
of a Physical Therapy Assistant to the Treatment Team for Management of Neck Pain:
A Retrospective Analysis of Outpatient Physical Therapy Clinics.
Cureus,
15(7),
e42751. https://doi.org/10.7759/cureus.42751
Baumann, A. N., Indermuhle, T., Oleson, C. J., Callaghan, M. E., Rogers, H., Pennacchio, C.,
Baldwin, K. D., & Leland, J. M., 3rd (2023b). Clinical Outcomes Associated With the
Addition of a Physical Therapist Assistant to a Rehabilitation Team When Treating
Musculoskeletal Shoulder Pain in the Outpatient Setting: A Retrospective Cohort Study.
Cureus,
15(7), e42680. https://doi.org/10.7759/cureus.42680
Corrini, C., Gervasoni, E., Perini, G., Cosentino, C., Putzolu, M., Montesano, A., Pelosin, E.,
Prosperini, L., & Cattaneo, D. (2023). Mobility and balance rehabilitation in multiple
sclerosis: A systematic review and dose-response meta-analysis.
Multiple sclerosis and
related disorders, 69, 104424. https://doi.org/10.1016/j.msard.2022.104424
Edwards, T., & Pilutti, L. A. (2017). The effect of exercise training in adults with multiple
sclerosis with severe mobility disability: A systematic review and future research
directions.
Multiple sclerosis and related disorders, 16, 31–39.
https://doi.org/10.1016/j.msard.2017.06.003
Physio and exercise for progressive conditions
Page 11 of 14
OFFICIAL
Page 11 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
El Hayek, M., Lobo Jofili Lopes, J. L. M., LeLaurin, J. H., Gregory, M. E., Abi Nehme, A. M.,
McCall-Junkin, P., Au, K. L. K., Okun, M. S., & Sal oum, R. G. (2023). Type, Timing,
Frequency, and Durability of Outcome of Physical Therapy for Parkinson Disease: A
Systematic Review and Meta-Analysis.
JAMA network open,
6(7), e2324860.
https://doi.org/10.1001/jamanetworkopen.2023.24860
Ernst, M., Folkerts, A. K., Gol an, R., Lieker, E., Caro-Valenzuela, J., Adams, A., Cryns, N.,
Monsef, I., Dresen, A., Roheger, M., Eggers, C., Skoetz, N., & Kalbe, E. (2024).
Physical exercise for people with Parkinson's disease: a systematic review and network
meta-analysis.
The Cochrane database of systematic reviews,
4(4), CD013856.
https://doi.org/10.1002/14651858.CD013856.pub3
Grimes, D., Fitzpatrick, M., Gordon, J., Miyasaki, J., Fon, E. A., Schlossmacher, M.,
Suchowersky, O., Rajput, A., Lafontaine, A. L., Mestre, T., Appel-Cresswell, S., Kalia,
S. K., Schoffer, K., Zurowski, M., Postuma, R. B., Udow, S., Fox, S., Barbeau, P., &
Hutton, B. (2019). Canadian guideline for Parkinson disease.
CMAJ : Canadian Medical
Association journal = journal de l'Association medicale canadienne,
191(36), E989–
E1004. https://doi.org/10.1503/cmaj.181504
Hammer, S., Toussaint, M., Vol sæter, M., Nesbjørg Tvedt, M., Drange Røksund, O., Reychler,
G., Lund, H., & Andersen, T. (2022). Exercise Training in Duchenne Muscular
Dystrophy: A Systematic Review and Meta-Analysis.
Journal of rehabilitation medicine,
54, jrm00250. https://doi.org/10.2340/jrm.v53.985
Keus, S., Munneke, M., Graziano, M., Paltamaa, J., Pelosin, E., Domingos, J., ... & Bloem, B.
(2014).
European physiotherapy guideline for Parkinson’s disease. The Netherlands:
KNGF/ParkinsonNet.
Kim, Y., Lai, B., Mehta, T., Thirumalai, M., Padalabalanarayanan, S., Rimmer, J. H., & Motl, R.
W. (2019). Exercise Training Guidelines for Multiple Sclerosis, Stroke, and Parkinson
Disease: Rapid Review and Synthesis.
American journal of physical medicine &
rehabilitation,
98(7), 613–621. https://doi.org/10.1097/PHM.0000000000001174
Kyriakatis, G. M., Lykou, P. M., Dimitriadis, Z., & Besios, T. (2023). Efficacy of remote exercise
and physiotherapy programs on depressive symptoms in people with multiple sclerosis -
A systematic review and meta-analysis.
Multiple sclerosis and related disorders, 79,
105067. https://doi.org/10.1016/j.msard.2023.105067
Lau, B., March, M. K., Harmer, A. R., Caruana, S., Mahony, C., & Dennis, S. (2024).
Experiences of Boosting Inpatient Exercise After HipFracture Surgery Using An
Alternative Workforce - A Qualitative Study.
BMC geriatrics,
24(1), 183.
https://doi.org/10.1186/s12877-024-04756-1
Learmonth, Y. C., P Herring, M., Russel , D. I., Pilutti, L. A., Day, S., Marck, C. H., Chan, B.,
Metse, A. P., & Motl, R. W. (2023). Safety of exercise training in multiple sclerosis: An
updated systematic review and meta-analysis.
Multiple sclerosis (Houndmil s,
Physio and exercise for progressive conditions
Page 12 of 14
OFFICIAL
Page 12 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
Basingstoke, England),
29(13), 1604–1631.
https://doi.org/10.1177/13524585231204459
Meng, L., Li, X., Li, C., Tsang, R. C., Chen, Y., Ge, Y., & Gao, Q. (2020). Effects of exercise in
patients with amyotrophic lateral sclerosis: a systematic review and meta-analysis.
American Journal of Physical Medicine & Rehabilitation,
99(9), 801-810.
https://doi.org/10.1097/PHM.0000000000001419
Motor Neuron Disease Australia. (2021).
Physical Activity and MND.
https://www.mndaustralia.org.au/mnd-connect/information-resources/physical-activity-
and-mnd
National Institute of Health and Care Excellence. (2017).
Parkinson’s disease in adults:
diagnosis and management [NG71]. https://www.nice.org.uk/guidance/ng71
O’Callaghan, G., Murray, D. & Vance, R. (2014). Guidelines for the physiotherapy
management of Motor Neuron Disease. Irish Hospice Foundation.
https://d2khofxhx95v1k.cloudfront.net/b1fdb917f1fea268a7a1b7b502dcd172.pdf
Osborne, J. A., Botkin, R., Colon-Semenza, C., DeAngelis, T. R., Gallardo, O. G., Kosakowski,
H., Martel o, J., Pradhan, S., Rafferty, M., Readinger, J. L., Whitt, A. L., & El is, T. D.
(2022). Physical Therapist Management of Parkinson Disease: A Clinical Practice
Guideline From the American Physical Therapy Association.
Physical therapy,
102(4),
pzab302. https://doi.org/10.1093/ptj/pzab302
Papadopoulou, M., Papapostolou, A., Dimakopoulos, R., Salakou, S., Koropouli, E.,
Fanouraki, S., Bakola, E., Moschovos, C., & Tsivgoulis, G. (2024). Non-
Pharmacological Interventions on Pain in Amyotrophic Lateral Sclerosis Patients: A
Systematic Review and Meta-Analysis.
Healthcare (Basel, Switzerland),
12(7), 770.
https://doi.org/10.3390/healthcare12070770
Sarigiovannis, P., Foster, N. E., Jowett, S., & Saunders, B. (2023). Developing a best practice
framework for musculoskeletal outpatient physiotherapy delegation: the MOPeD mixed-
methods research study protocol.
BMJ open,
13(3), e072989.
https://doi.org/10.1136/bmjopen-2023-072989
Sarigiovannis, P., Foster, N. E., Jowett, S., & Saunders, B. (2022). Delegation of workload
from musculoskeletal physiotherapists to physiotherapy assistants/support workers: A
UK online survey.
Musculoskeletal science & practice, 62, 102631.
https://doi.org/10.1016/j.msksp.2022.102631
Sarigiovannis, P., Jowett, S., Saunders, B., Corp, N., & Bishop, A. (2021). Delegation by Al ied
Health Professionals to Al ied Health Assistants: a mixed methods systematic review.
Physiotherapy, 112, 16–30. https://doi.org/10.1016/j.physio.2020.10.002
Snowdon, D. A., Wang, Y. T., Cal isaya, M. L., Col yer, T. A., Jol iffe, L., Johns, N., Vincent, P.,
Pragash, N., & Taylor, N. F. (2024). Staying Active with Multimorbidity In Acute hospital
settings (StAMInA) trial: protocol for a feasibility randomised controlled trial of al ied
Physio and exercise for progressive conditions
Page 13 of 14
OFFICIAL
Page 13 of 14

FOI 24/25-0223
Research paper
Document 2
OFFICIAL
For Internal Use Only
health assistant mobility rehabilitation for patients with multimorbidity.
BMJ open,
14(1),
e078843. https://doi.org/10.1136/bmjopen-2023-078843
Snowdon, D. A., King, O. A., Dennett, A., Pinson, J. A., Shannon, M. M., Collyer, T. A., Davis,
A., & Wil iams, C. M. (2022). Delegation of patient related tasks to allied health
assistants: a time motion study.
BMC health services research,
22(1), 1280.
https://doi.org/10.1186/s12913-022-08642-7
Snowdon, D. A., Vincent, P., Cal isaya, M. L., Col yer, T. A., Wang, Y. T., & Taylor, N. F.
(2021). Feasibility of allied health assistant management of people with acute hip
fracture: protocol for a feasibility randomised controlled trial.
BMJ open,
11(11),
e054298. https://doi.org/10.1136/bmjopen-2021-054298
Snowdon, D. A., Storr, B., Davis, A., Taylor, N. F., & Wil iams, C. M. (2020). The effect of
delegation of therapy to allied health assistants on patient and organisational outcomes:
a systematic review and meta-analysis.
BMC health services research,
20(1), 491.
https://doi.org/10.1186/s12913-020-05312-4
Taul-Madsen, L., Connolly, L., Dennett, R., Freeman, J., Dalgas, U., & Hvid, L. G. (2021). Is
Aerobic or Resistance Training the Most Effective Exercise Modality for Improving
Lower Extremity Physical Function and Perceived Fatigue in People With Multiple
Sclerosis? A Systematic Review and Meta-analysis.
Archives of physical medicine and
rehabilitation,
102(10), 2032–2048. https://doi.org/10.1016/j.apmr.2021.03.026
Voet, N. B., van der Kooi, E. L., van Engelen, B. G., & Geurts, A. C. (2019). Strength training
and aerobic exercise training for muscle disease.
The Cochrane database of systematic
reviews,
12(12), CD003907. https://doi.org/10.1002/14651858.CD003907.pub5
Zhou, B., Wei, J., Zhang, Y., Liu, Y., Shan, S., Ye, S., Li, B., Fan, D., & Luo, Y. (2022).
Different observation period of exercise training in amyotrophic lateral sclerosis
patients: A meta-analysis.
Frontiers in neurology, 13, 986882.
https://doi.org/10.3389/fneur.2022.986882
Physio and exercise for progressive conditions
Page 14 of 14
OFFICIAL
Page 14 of 14