FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 1
Acquired brain injury Disability
Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:09:18
Page 1 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Acquired brain injury Disability Snapshot
Table of Contents
1 Peak body consulted ........................................................................................................... 4
2 What is acquired brain injury? ........................................................................................... 5
3 Misconceptions about acquired brain injury .................................................................... 6
4 How is acquired brain injury diagnosed? .......................................................................... 7
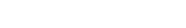
5 Language and terminology ................................................................................................. 8
6 Enabling social and economic participation ..................................................................... 9
7 How can I tailor a meeting to suit a participant with an acquired brain injury? .......... 10
8 Helpful links ........................................................................................................................ 11
Table of Contents – 2
Page 2 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Acquired brain injury Disability Snapshot
This Disability Snapshot provides general information about acquired brain injury to assist you
in communicating effectively and supporting the participant in developing their goals in a
planning meeting. Each person is an individual and wil have their own needs, preferences and
experiences that wil impact on the planning process. This information has been prepared for
NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 3 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Acquired brain injury Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with Brain Injury Australia.
Peak body consulted – 4
Page 4 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Acquired brain injury Disability Snapshot
2 What is acquired brain injury?
Acquired brain injury (ABI) is a term used to describe multiple disabilities caused by damage to
the brain after birth. An ABI can result in deterioration in a person’s cognitive, physical,
emotional or independent functioning.
An ABI can occur from:
• an accident
• stroke
• brain tumour
• head trauma
• infection (such as encephalitis or meningitis)
• poisoning (alcohol or other drug abuse)
• lack of oxygen (referred to as hypoxia or anoxia) or
• degenerative neurological diseases[1].
Some ABIs result in permanent physical disability, for example - paralysis, problems with
balance and coordination, epilepsy, vision or hearing loss. Other significant impacts can be
cognitive or behavioural, for example - chal enging behaviour, poor short-term memory, reduced
attention and concentration, difficulties with learning, planning and solving problems.
Challenging behaviours may include irritability, social (sometimes sexual) disinhibition and
verbal (sometimes physical) aggression.
What is acquired brain injury? – 5
Page 5 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Acquired brain injury Disability Snapshot
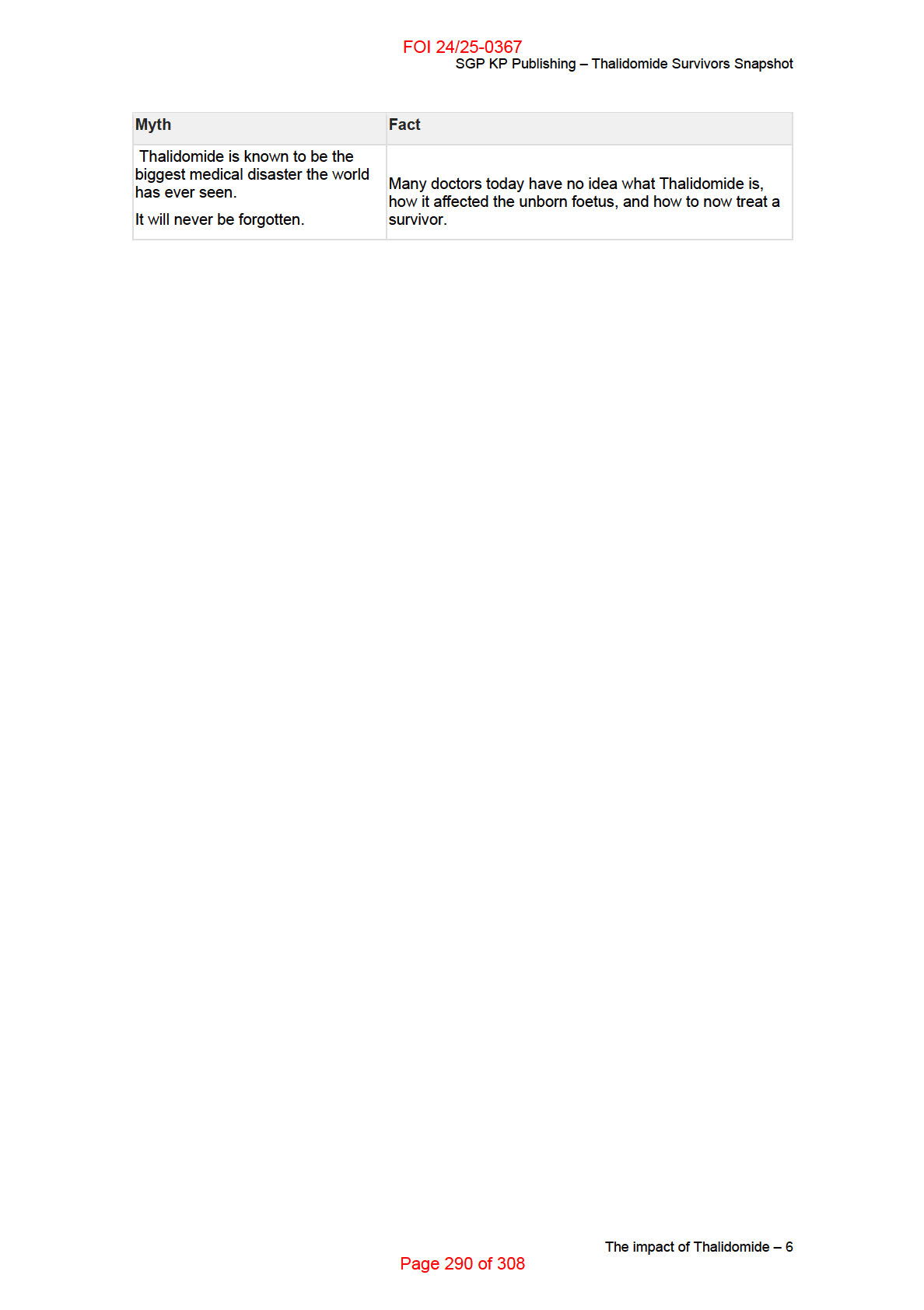
3 Misconceptions about acquired brain injury
Some misconceptions about ABI include:
• ABI is an intel ectual disability
• Recovery from an ABI doesn’t continue beyond two years.
o While the greatest improvement in function fol owing an ABI occurs in the first
two years, recovery can continue for at least five years following the injury.
• Everyone recovers from a mild traumatic brain injury.
o Approximately one in four people who have concussion/s or mild TBIs do not
make a full recovery within the expected timeframes. They can experience
ongoing physical symptoms such as headaches and dizziness, impacts on
cognition, and behaviour and/or mental il ness. For some people, the
impairment is permanent.
Misconceptions about acquired brain injury – 6
Page 6 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Acquired brain injury Disability Snapshot
4 How is acquired brain injury diagnosed?
Participants who have a severe ABI wil likely have one or more neuropsychological
assessments. Assessments include an interview and standardised tests to determine the
injury’s effects on cognition and behaviour. Recommendations are then made for therapies to
improve function.
The period of time in which the participant is unable to have continuous day-to-day memory
(duration of post-traumatic amnesia) is currently the best single predictor of severity for the
disability.
How is acquired brain injury diagnosed? – 7
Page 7 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Acquired brain injury Disability Snapshot
6 Enabling social and economic participation
The lived experience of a brain injury is usual y very different from a lifelong developmental or
intel ectual disability. People with an ABI wil likely remember what they were able to do before
their injury. Their engagement with the NDIS may be affected by grief. Some participants may
therefore have difficulty setting and achieving goals. They may also experience a breakdown in
relationships with family and friends.
The circumstances of the participant’s injury may also be associated with embarrassment or
shame, especially when the injury was, or is perceived to be, the participant’s fault. People with
an ABI have a very high lifetime risk of mental il ness, such as depression.
Help the participant adapt to their disability by reconnecting them to as much of their life before
injury as possible. For example, exploring pre-injury employment, pursuits and pastimes.
It may be appropriate to explore ways for participants to go back to their previous career or
profession with supports in place. For others, being supported through a vocational ‘discovery’
process to re-explore their strengths and interests in preparation for work could be useful.
Volunteering to build confidence and connect with the community is another way to prepare for
work.
While employers are required to make reasonable adjustments to accommodate needs in the
workplace – supports that are above and beyond this could be funded under the NDIS.
Participants may require NDIS funding for specialist disability assessment services to access
external employment retention and support initiatives, such as the Work Assist program
provided by Disability Employment Services.
Peer support from other people with ABIs can also be helpful to improve social and economic
participation.
Enabling social and economic participation – 9
Page 9 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Acquired brain injury Disability Snapshot
7 How can I tailor a meeting to suit a participant with
an acquired brain injury?
A person with ABI may recover well physically their cognitive and/or behavioural disability can
be significant. Their disability may not be obvious to someone meeting them for the first time
and that is why ABI is often referred to as an “invisible disability”.
Participants can also lack insight into their disability and be unaware of their limitations, or may
have unrealistic expectations of their recovery and/or set unrealistic goals. It is recommended,
with participant consent, to check unmet support needs with significant others, family members,
clinicians or allied health professionals.
Many people with an ABI experience tiredness and difficulties with attention and/or
concentration and reduced information-processing speed. You can tailor a meeting to suit the
participant by:
• asking their preferred meeting length and discussing any other adjustments that might
assist when scheduling a meeting
• securing a meeting location free of competing background noise or distractions
• scheduling short meetings or taking breaks during longer meetings
• checking how they are feeling during the meeting
• communicating in short, simple, sentences using plain English
• checking for understanding without questioning the participant’s intelligence, ask “did
that make sense?” rather than “do you understand what I’m saying?”.
How can I tailor a meeting to suit a participant with an acquired brain injury? – 10
Page 10 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Acquired brain injury Disability Snapshot
8 Helpful links
• Brain Injury Australia (peak body)
• Stroke Foundation (national charity)
• Synapse (service provider)
• Ontario Neurotrauma Foundation (Canadian research and prevention organisation)
[1] Australian Institute of Health and Welfare
National Community Services Data Dictionary
(2014)
Helpful links – 11
Page 11 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 2
Autism spectrum disorder Disability
Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:09:45
Page 12 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
Table of Contents
1
What is autism spectrum disorder ..................................................................................... 4
2
How is autism spectrum disorder diagnosed? ................................................................. 5
3
Language and terminology ................................................................................................. 6
4
Enabling social and economic participation ..................................................................... 7
5
Barriers to achieving economic and social participation ................................................ 8
6
How can I tailor a meeting to suit a participant with autism spectrum disorder? ...... 10
7
Peak body consulted ......................................................................................................... 12
8
Helpful links ........................................................................................................................ 13
Table of Contents – 2
Page 13 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
This Disability Snapshot provides general information about autism spectrum disorder to assist
you in communicating effectively and supporting the participant in developing their goals in a
planning meeting. Each person is an individual and will have their own needs, preferences and
experiences that will impact on the planning process. This information has been prepared for
NDIA staff and partners and is not intended for external distribution.
What is autism spectrum disorder – 3
Page 14 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
1 What is autism spectrum disorder
Autism spectrum disorder (ASD), referred to as “autism” in the remainder of this snapshot, is the
collective term for a group of neurodevelopmental conditions affecting the brain’s growth and
development. Autism can affect the way individuals interact with others and how they
experience the world around them.
Autism is a life-long condition which can impact, to varying degrees, all areas of a person’s life,
including social communication and social interaction.
The behavioural features of autism are often present before a person is three years of age but
in others they may not be recognised until their school years or later in life. The developmental
challenges, signs and/or symptoms can vary widely in nature and degree between individuals,
and in the same individual over time – that is why the term “spectrum” is used.
Autism has a strong genetic base so there may be multiple diagnoses or related conditions
within a single family and their extended family.
A person living with autism may experience:
challenges with communication and interacting with others
repetitive and different behaviours, moving their bodies in different ways
strong interest in one topic or subject
unusual reactions to what they see, hear, smell, touch or taste
preference for routines and dislike of change.
What is autism spectrum disorder – 4
Page 15 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
2 How is autism spectrum disorder diagnosed?
Autism is diagnosed on the basis of behavioural presentation and developmental history.
Careful developmental monitoring of social attention and communication behaviours in early life
can lead to early identification and referral for a diagnosis. A reliable diagnosis is possible from
as early as 18 to 24 months of age. Some people may be diagnosed in later childhood,
adolescence or adulthood. Diagnosis is ideally undertaken by a multidisciplinary team with allied
health and medical expertise. The DSM 5 is the most commonly used diagnostic criteria in
Australia.
How is autism spectrum disorder diagnosed? – 5
Page 16 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
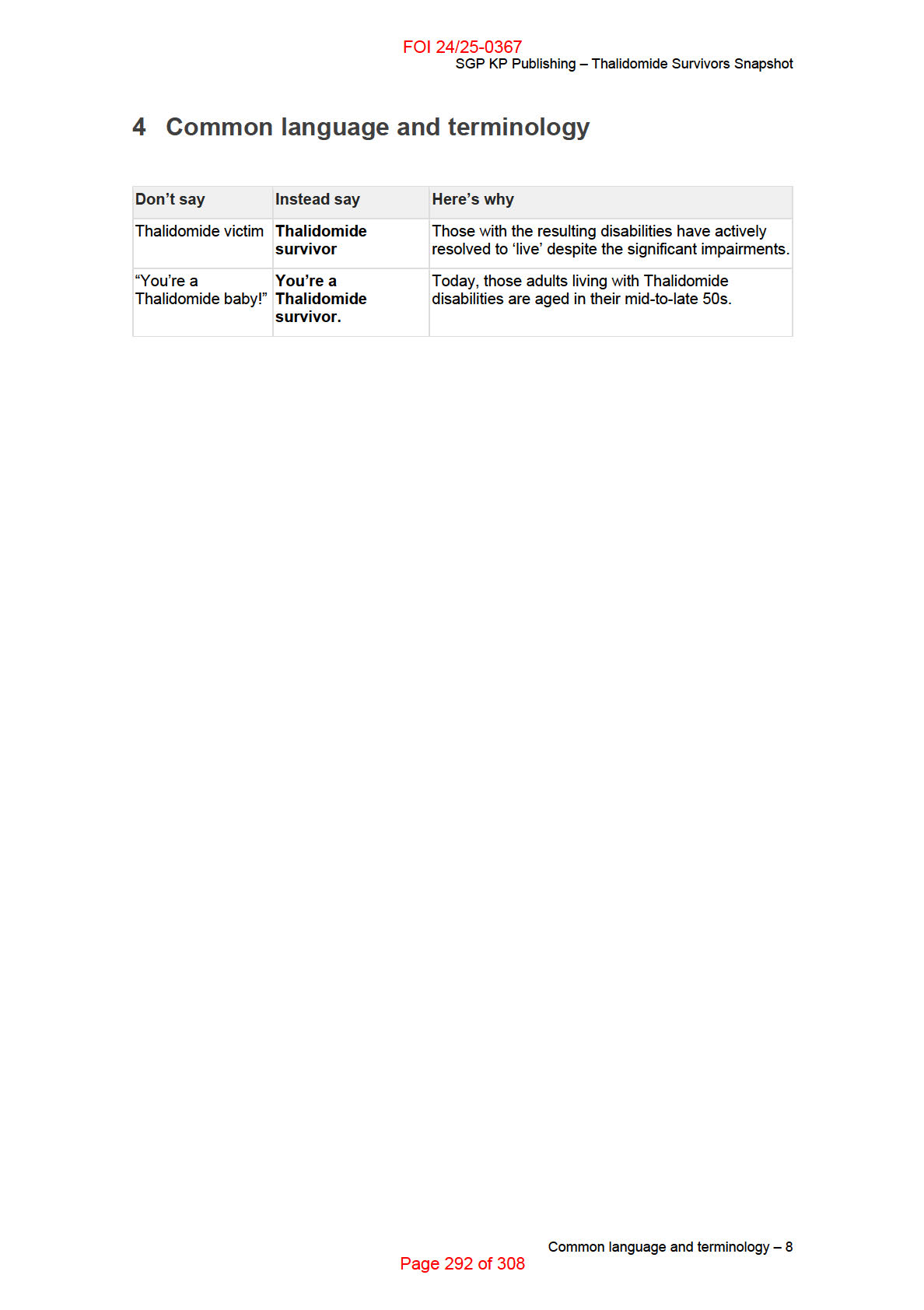
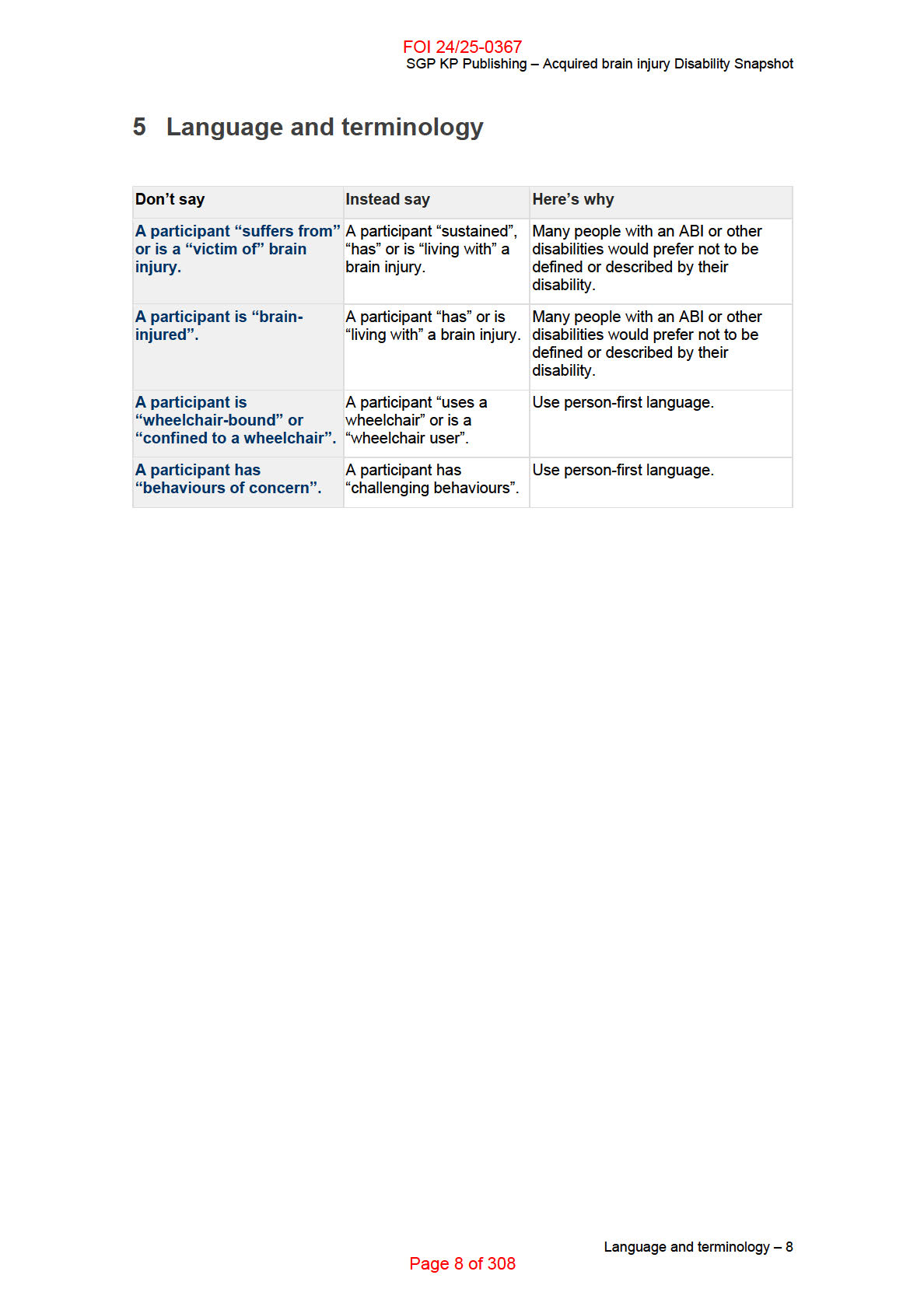
3 Language and terminology
Terminology can be a sensitive subject and reflects a range of personal perspectives.
Some families and individuals prefer “person first” language for example, “I am a person with
autism”. Others prefer “identify first” language, for example, “I am autistic”.
You should let the participant take the lead in describing themselves, their disability and their
preferred terminology. Use their preferred terminology consistently in all meetings and
correspondence.
Common terms used include:
DSM-5 - the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition. It is
published by the American Psychiatric Association and is the most commonly used tool
across the world for diagnosing psychiatric conditions and disabilities
neurodiversity - the concept that neurological differences are a natural part of human
diversity. It highlights sensitivities to words like “disorder” and “cure”
neurodivergent - is a broad term meaning atypical neurology; meaning there is a
general functional difference
neurologically typical (also referred to as NT) - a reference for people who are not on
the autism spectrum.
Language and terminology – 6
Page 17 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
4 Enabling social and economic participation
A person’s support needs for social and economic participation will vary depending on their
strengths and level of function.
Data from the Australian Bureau of Statistics Survey of Disability, Ageing and Carers (2015)
indicates people with autism experience poorer outcomes compared to other disability groups in
relation to education, economic participation, social participation and independent living.
Consider supports that reduce these barriers such as capacity building or support coordination.
Planning for transitions from school to higher education or work is also important.
NDIS funding can support people with autism to build life skills, capabilities and independence.
It can give them a greater understanding of what their interests are and what work might be
suitable. It can assist them build specific work related skills which could support them to engage
with other government services such as Disability Employment Services (DES).
Work adjustments or NDIS funding for specialist disability assessment services can help create
opportunities for jobs to be adapted to meet the capabilities and strengths of the individual and
to address access and lived challenge barriers as described below.
Enabling social and economic participation – 7
Page 18 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
5 Barriers to achieving economic and social
participation
Likely barriers to achieving similar levels of independent living, education, economic and social
participation to other disability types were identified in the ABS Survey (2015) and are listed
below.
NDIS supports can assist to address some of these barriers and improve access to social and
economic participation for people with autism. Funding for capacity building can support
participants build their planning, organisation and independent living.
Support coordination can connect participants with services and providers for assessment and
support. For example, referral to a specialist providers such as an occupational therapist can
help arrange adjustments to the physical environment for school, work or social activities.
Societal attitudes
lack of public awareness and understanding regarding autism and how it impacts on
daily living
negative media portrayal of autism
Accessibility challenges
access to timely and affordable assessments, including an understanding of the
functional impact for the individual
access to timely and appropriate supports and services following initial diagnosis and
as needs change over time
structures or physical features of the built environment, for instance lighting, noise,
smells, colours, crowding
mainstream and specialised supports and services not understanding autism or taking
individualised approaches
Lived challenges
cognitive and social differences
difficulties with planning and organisation
failure of agencies and services to work in partnership with the individual and their
friends/family to understand and address needs
experiencing bullying and harassment in schools, community settings and workplaces
failure of mainstream and disability services to provide reasonable adjustments in
education and work settings
the specific characteristics of autism (difficulties in social interactions and
communication, inflexible behaviours and routines, and executive function difficulties)
Barriers to achieving economic and social participation – 8
Page 19 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
may lead to increased difficulty in relationships, completing education, gaining and
maintaining employment, housing and health care
failure of services to recognise other health conditions (comorbidities) such as anxiety,
stress and depression.
Barriers to achieving economic and social participation – 9
Page 20 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
6 How can I tailor a meeting to suit a participant with
autism spectrum disorder?
Before a meeting
In preparation for a meeting:
provide detailed information about how and where to present for a meeting and what
the planning process will cover. Many people with autism find new events or tasks
difficult and may need
provide information at least five days before a meeting, where possible
offer a choice of meeting options such as, face to face, phone, using written and/or
verbal information
inform the individual a support person can attend
if the meeting needs to be re-scheduled or the Agency staff member attending changes,
give as much advance notice and explain the reason for the change
gather information about autism and the person you are meeting with. The participant
and their support person are best placed to inform you about their needs and
experience living with autism.
Communication during a meeting
When communicating during a meeting:
anticipate the participant may not make eye contact
consider the sensory environment, for example, sound, lights and invite the participant
to use supports to stay calm, such as, fidgets
simplify your language and use key words, natural gestures and pictures where
appropriate. Be prepared that the individual’s understanding of verbal communication
could be very literal
allow time for processing information if necessary. Pause periodically, to allow
questions and check for understanding
use positive statements as it is easier to understand positive sentences that say what to
do, rather than what not to do
sit side by side rather than face to face
acknowledge anxiety. If the individual keeps coming back to a particular issue, be
patient and allow time to answer the necessary questions to put their mind at ease
make things as predictable as possible, including running the meeting to time
allow for gender differences in the presentation of autism. Females in particular can be
adept at masking their symptoms and tend to show less severe social and
communicative symptoms. Be prepared to use gentle probing questions and draw on a
range of evidence sources to identify their support needs
How can I tailor a meeting to suit a participant with autism spectrum disorder? – 10
Page 21 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
consider many individuals view their autism as an important and valued part of their
personal identity. They don’t see their autism as a condition that needs to be “fixed or
cured
be aware that parents attending the meeting may also be highly stressed and anxious
or may also be a person with autism.
Planning considerations
Things to consider when developing or reviewing a participant’s plan:
focus on the functional impact of the diagnosis. Verifying the diagnosis or interpreting
reports made by health professionals can be frustrating for families and individuals who
have undergone an extensive (and costly) diagnostic process
include support coordination where there are complex needs or other health conditions
(comorbidities) that cross health, disability, community, housing and/or employment
sectors
consider and plan for life stage transitions, such as primary to high school or school to
work
remember people with autism have individual and unique needs which can change
throughout their life. It is best not to make assumptions based on your existing
knowledge and experience of autism.
How can I tailor a meeting to suit a participant with autism spectrum disorder? – 11
Page 22 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
7 Peak body consulted
In developing this resource we consulted with the Australian Autism Alliance, who consulted
with the following partners and supporters:
AEIOU
Foundation
Amaze
Autistic Self Advocacy Network (ASAN AUNZ)
Australasian Society for Autism Research (ASfAR)
Autism Asperger Advocacy Australia (A4)
Autism Association of Western Australia
Autism
Co-operative
Research Centre (CRC)
Autism
Queensland
Autism
SA
Autism Spectrum Australia (Aspect)
Autism
Tasmania
I CAN; and
Autism Awareness Australia.
Peak body consulted – 12
Page 23 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Autism spectrum disorder Disability Snapshot
8 Helpful links
For further information refer to:
Australian Autism Alliance
Raising Children
Autistic Self Advocacy Network
Autism Aspergers Advocacy Australia
I Can Network
See also, service providers who are partners of the Australian Autism Alliance:
Amaze
Autism Spectrum Australia
AEIOU Foundation for Children with Autism
Autism Queensland
Autism South Australia
Autism Tasmania
Autism Association of Western Australia
Other Autism Organisations
Helpful links – 13
Page 24 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 3
Blindness and vision impairment
Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:09:59
Page 25 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Blindness and vision impairment Disability Snapshot
Table of Contents
1 Peak body consulted ........................................................................................................... 4
2 What is blindness and vision impairment? ....................................................................... 5
3 How is blindness and vision impairment diagnosed? ..................................................... 6
4 Language and terminology ................................................................................................. 7
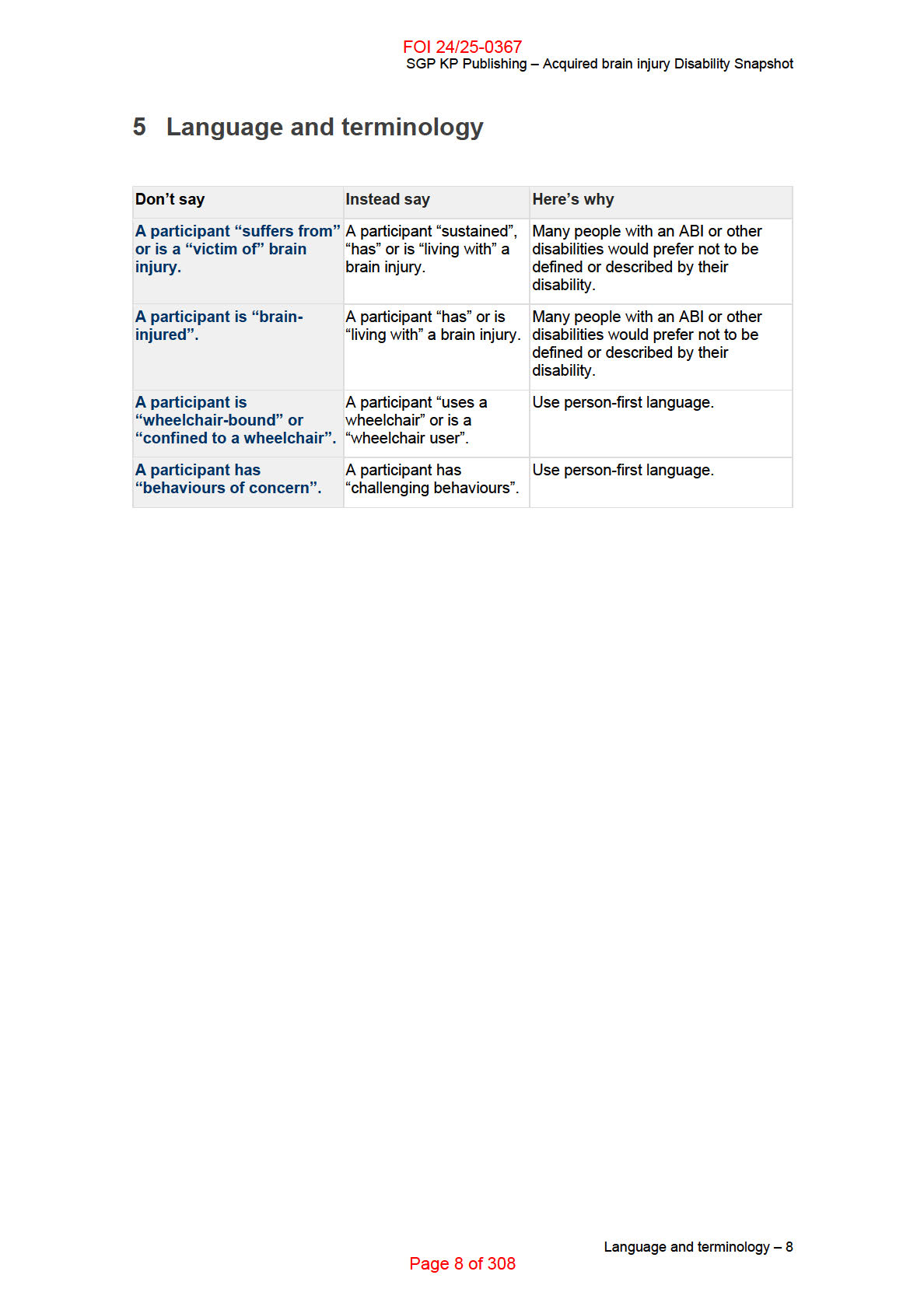
5 Communicating with people who are blind or vision impaired ....................................... 8
6 Enabling social and economic participation ..................................................................... 9
7 How can I tailor a meeting to suit a participant with blindness and vision
impairment? ............................................................................................................................... 10
8 Helpful links ........................................................................................................................ 12
Table of Contents – 2
Page 26 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Blindness and vision impairment Disability Snapshot
This Disability Snapshot provides general information about blindness and vision impairment. It
wil assist you in communicating effectively and supporting the participant in developing their
goals in a planning meeting. Each person is an individual and wil have their own needs,
preferences and experiences that wil impact on the planning process. This information has
been prepared for NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 27 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Blindness and vision impairment Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with Blind Citizens Australia.
Peak body consulted – 4
Page 28 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Blindness and vision impairment Disability Snapshot
2 What is blindness and vision impairment?
Blindness and vision impairment is a sensory disability that affects a person’s access to social,
economic and physical participation. It reduces access to information, in particular written
information. This affects the person’s ability to independently work, socialise and safely go
about their lives in the community.
While more than 453,000 Australians are blind or vision impaired, the number of people eligible
for the NDIS based on the primary disability of blindness or vision impairment is much smal er.
This is because blindness and vision impairment is primarily associated with the ageing
process.
What is blindness and vision impairment? – 5
Page 29 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Blindness and vision impairment Disability Snapshot
3 How is blindness and vision impairment diagnosed?
Some people are born blind or with a vision impairment. Others may acquire it later in life,
through a genetic eye condition or accident. Some conditions are degenerative and get worse
over time.
Eye specialists such as optometrists and ophthalmologists diagnose vision impairments.
Orientation and mobility specialists train people who are blind or vision impaired to use mobility
aids and assistive technologies. Occupational therapists provide training and advice with
independent living skil s.
How is blindness and vision impairment diagnosed? – 6
Page 30 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Blindness and vision impairment Disability Snapshot
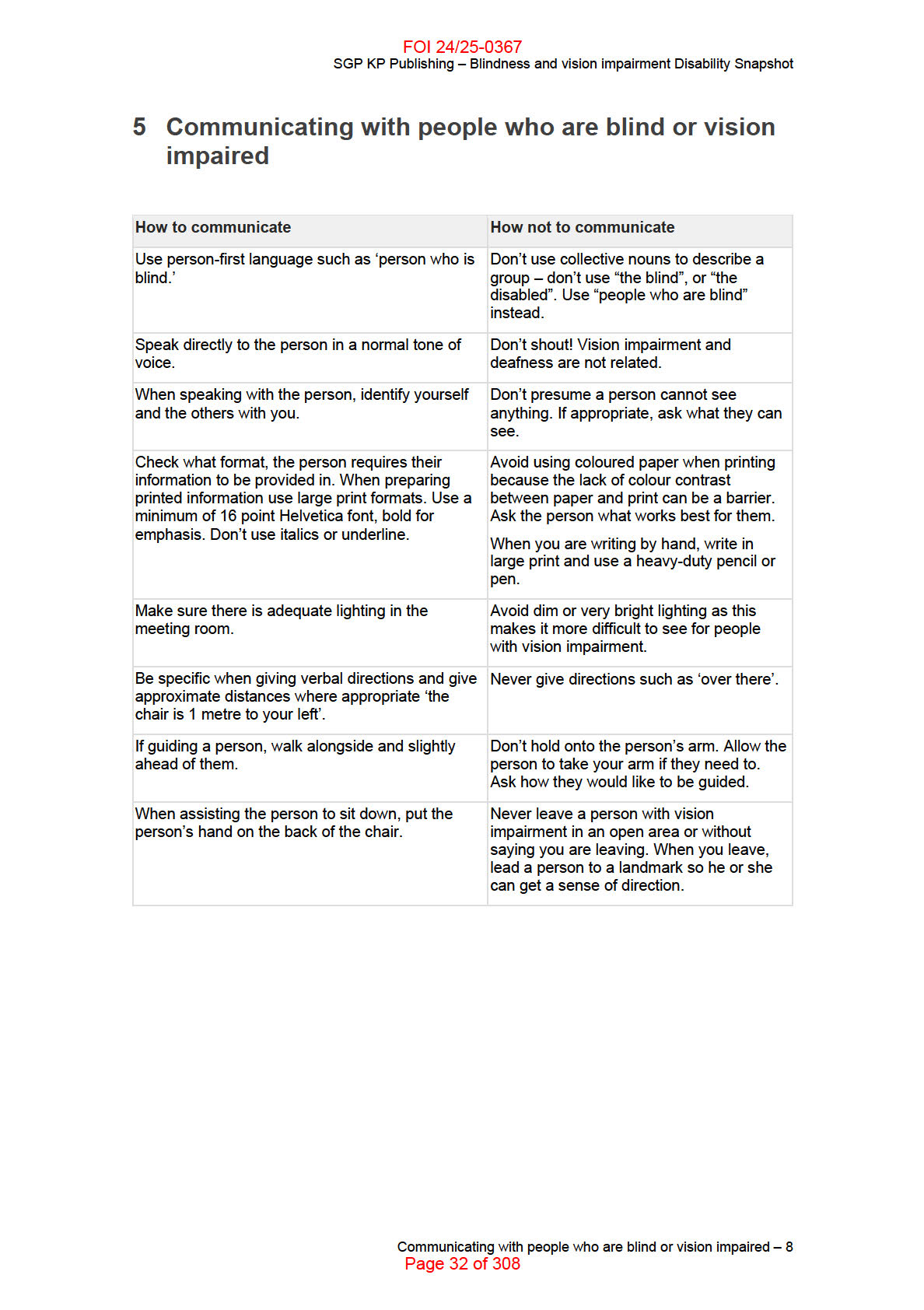
4 Language and terminology
Language shapes the way we view the world. The words we use can have a powerful effect.
How we write and refer to people with disability can affect the way they are viewed by the
community. Some words can degrade and diminish people with a disability.
Person-first language places the person first and the impairment second. Person-first language
is used to acknowledge that a disability is not as important as the person’s individuality or
humanity.
Persons with disability or people with disability are the most commonly used terms in Australia.
If you are not sure of the correct words to use, don’t be afraid to ask. Focus on the person,
rather than their disability. Offer an apology if you feel you’ve said the wrong thing and always
be wil ing to communicate.
Language and terminology – 7
Page 31 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Blindness and vision impairment Disability Snapshot
6 Enabling social and economic participation
Busy, cluttered and visual y oriented environments can be a major barrier to participation in
normal life, like; going to the shops, going for a walk in the park, going to work, looking for work
or simply socialising.
Work enables an individual to establish greater financial security, develop a sense of
productivity, purpose and make new connections with people in their community.
People who are blind or vision impaired can come up against attitudinal barriers which
compromise their dignity and independence. For example, some employers’ negative attitudes
or lack of knowledge contribute to the high rate of unemployment amongst people who are blind
or vision impaired–a rate which is four times the national average. This has a dramatic impact
on the inclusion and participation of people who are blind or vision impaired.
Assistive technology may also be required to support participation in work. To enable and
maintain work, ongoing supports or adjustments at work may be needed. This might require
NDIS funding for specialist disability or employment related assessment services. Alternatively
the person can access external employment retention and support initiatives such as Work
Assist provided by the Disability Employment Services (DES) program.
Enabling social and economic participation – 9
Page 33 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Blindness and vision impairment Disability Snapshot
7 How can I tailor a meeting to suit a participant with
blindness and vision impairment?
When meeting someone who is blind or vision impaired for the first time, they may not see your
extended hand to shake hands in greeting. Tel ing someone that you would like to shake their
hand is appropriate. Otherwise a friendly verbal greeting is okay.
Glossy brochures wil not attract or be useful to people who are blind or have minimal usable
vision. Think about other ways to share information such as information on a website (which
meets web accessibility standards, W3C), large print information with good contrast, audio
format, brail e or information over the phone.
Prior to a meeting, it is important to ask the person their preferred format for accessing
information. That way the planner can organise material in their preferred format.
During telephone conversations, especial y when organising planning meetings or other
information, encourage the person who is blind or vision impaired to make note of any times,
dates and contact information. Ask if they would like the details for the meeting and contact
information sent to them or a reminder call the day before. It is important this information is
provided in the person’s preferred communication format.
When you are planning the meeting, discuss if it wil be held at their home or another location. If
another location, ask if they wil be bringing a support person along with them. Ask what they
need from you to create an accessible environment, for example, meeting them at the entrance.
Keep in mind each person’s requirements may differ.
Verbal communication
• No matter how well you know a person who is blind or vision impaired, it is good
practice to introduce yourself when you approach the person, particularly if you are both
away from your usual environment. A simple ‘Hi Sarah, it’s John’ can help a person who
is blind or vision impaired know who has approached.
• It’s okay to use the word ‘see’ ‘see you later’ and ‘look’ ‘do you mind taking a look at
this?’ People who are blind or vision impaired use these words too.
• Talk to the person, not their guide dog.
Written communication
• Not al people who are blind read brail e. Some use brail e for reading, labelling,
identifying items or to read signs. Some don’t use brail e at all.
• How people read information can come down to personal choice, convenience and
ease. Some people with usable functional vision might use standard print or large print
(san serif font like ‘Arial’ in size 16 or greater), audio format, electronic formats (such as
word documents, html, or rtf), brail e or a number of these formats depending on the
task they are working on.
How can I tailor a meeting to suit a participant with blindness and vision impairment? – 10
Page 34 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Blindness and vision impairment Disability Snapshot
• Pictures, symbols, tables and a host of other marketing tools can be inaccessible,
depending on the technology the person is using. Therefore it’s important to check with
the person what works best.
• Word documents, html and rtf formats are a lot easier to read for people who use
screen-reading software.
• When offering information in accessible formats, offer large print, brail e, audio, or
electronic versions. Refer to Round Table Guidelines for producing information in
accessible formats.
How can I tailor a meeting to suit a participant with blindness and vision impairment? – 11
Page 35 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Blindness and vision impairment Disability Snapshot
8 Helpful links
• Blind Citizens Australia (BCA)
• Video featuring Graeme Innes AM from the NSW Government’s 2015 Don’t Dis my
Ability campaign.
• Blog post: A day in the life with Stargardts disease, Matt De Gruchy.
• Blog site, Where’s Your Dog? Article: My Roommate is Blind – Help!
• Dialogue in the Dark – an experiential awareness raising tour, led by people who are
blind or vision impaired.
Helpful links – 12
Page 36 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 4
Carers Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:10:11
Page 37 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
Table of Contents
1 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 About carers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 Carers and the NDIS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 Why respite is important . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
5 Can a plan include NDIS funding for respite? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 How can I help carers to sustain their capacity to provide informal supports? . . . . . . 9
7 Case study examples of respite supports . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
7.1 Short-term accommodation for Peter ............................................................................... 10
7.2 Short-term accommodation for Henry .............................................................................. 10
7.3 Access to the community for Jordan ................................................................................ 11
7.4 In home supports and personal care for Sami ................................................................. 11
7.5 In home supports and personal care for Eleesha ............................................................ 11
8 Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13
Table of Contents – 2
Page 38 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
This Disability Snapshot provides general information about carers to assist you in
communicating effectively and supporting the participant in developing their goals in a planning
meeting. Each person is an individual and wil have their own needs, preferences and
experiences that wil impact on the planning process. This information has been prepared for
NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 39 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with Carers Australia, the national peak body
representing Australia’s unpaid carers.
Peak body consulted – 4
Page 40 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
2 About carers
The sustainability of the National Disability Insurance Scheme (NDIS) depends on the capacity
and wil ingness of family and friend carers to provide informal supports and unpaid care.
Australian Bureau of Statistics’ data from 2015 revealed that:
• 26% of primary carers (who provide the most substantial care for someone with
disability, chronic il ness, mental health condition or is frail or aged) had been caring for
between 5 and 9 years and 28% had been caring for between 10 and 24 years
• 33% of carers were providing care for 40 hours or more per week and in many cases,
substantially more
• 50% of primary carers identified that caring had one or more negative impacts on their
physical or emotional wellbeing
• 36% indicated they were weary and lacked energy
• 12% said they frequently felt angry and resentful
• 48% reported interrupted sleep
• 12% had been diagnosed with a stress related il ness.
About carers – 5
Page 41 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
3 Carers and the NDIS
Families and carers make a valuable contribution to supporting participants. It is important to
take the time to listen to carers and support them in their role. They are often the greatest
advocates for participants.
The participant statement in a participant’s plan contains important information about the
participant’s life, their living arrangements, relationships and plan goals. As part of the
discussion to complete the participant statement, consider what may be required to strengthen
and build the capacity of those providing informal support.
The family questionnaire,
usually completed during a planning meeting
is an opportunity to
capture the experience of the family or care giver and discuss whether they have sufficient
support to provide care. A number of organisations have developed pre-planning guidance for
families and carers to assist them identify their own caring role. If they choose to, a carer can
also provide a carer statement. To access the Carers Australia Carers Checklist refer to the
Helpful links section below.
Carers and the NDIS – 6
Page 42 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
4 Why respite is important
While families and carers take pleasure and satisfaction in supporting their loved ones, they
may experience stress from caring. Carers often need support and relief. They may need to
take a break from time-to-time to sustain their own wellbeing, their relationships with others and
their capacity to continue caring.
Respite can reduce carers’ stress and give them an opportunity to recharge their batteries. It
can also assist them in continuing to provide quality care.
Respite can also assist participants. A period in short-term accommodation or participation in
community activities can provide opportunities to experience new environments, make new
social connections and in some cases, develop new skil s.
Why respite is important – 7
Page 43 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
5 Can a plan include NDIS funding for respite?
Funding for respite is available under the NDIS. Respite aims to support ongoing caring
arrangements between participants and their carers by providing carers with short term breaks
from their caring responsibilities.
Participants can purchase a number of supports through their NDIS plan for respite
arrangements including:
• short-term accommodation
• temporary periods of extra personal supports so that the participant can remain at home
when families and/or carers are not available
• support to participate in community activities, resulting in a break for carers.
The NDIS funds reasonable and necessary supports that facilitate respite and build
independence, offer time away from the home or provide supports in the home. Examples are
provided in the case studies below. These supports can reduce the demand on carers and give
them a break from caring responsibilities.
Can a plan include NDIS funding for respite? – 8
Page 44 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
6 How can I help carers to sustain their capacity to
provide informal supports?
Let carers know that, while the NDIS supports the goals and aspirations of the participant(s)
they are caring for, it recognises that supporting family and friend carers in their caring role is
also important.
Al ow carers to explain to you the type of care and amount of care they provide. Carers should
feel comfortable to be able share any concerns they have about their capacity to continue
providing their current level of care. If they are unwil ing to raise these issues in the presence of
the person they care for, a written carer statement can be provided. Refer to the Helpful links
section below for examples.
Explain to carers how the participant’s plan can be used to purchase supports like short term
accommodation which offers value for the participant and a break for carers.
How can I help carers to sustain their capacity to provide informal supports? – 9
Page 45 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
7 Case study examples of respite supports
Taking the time to listen to families and carers may identify innovative supports that facilitate
respite. Several examples are included in the case studies below to demonstrate different
arrangements.
7.1 Short-term accommodation for Peter
Carl, aged 64, and Sophie, aged 59, care for their adult son, Peter, who has cerebral palsy,
poorly controlled epilepsy, an intellectual impairment and respiratory problems. Carl and Sophie
immigrated to Australia in 1990 and would like to travel to their home country to visit their elderly
parents and catch up with other family and friends. They plan to spend three weeks overseas.
They don’t believe they can manage taking Peter with them. Carl and Sophie have no friends or
family members able to provide care in their absence so they wil need to explore alternative
accommodation options for Peter while they are overseas.
In this situation funding for short-term accommodation in Peter’s plan wil allow his parents to
take a break from their caring role. It wil also benefit Peter by having some experience with
other carers and environments. This is important preparation for when Carl and Sophie won’t be
able to care for Peter at home because his parents are getting older. Peter supports his parents’
request.
7.2 Short-term accommodation for Henry
Henry, aged 9, has severe autism and regularly has difficulty controlling his behaviour which
includes physical and emotional aggression. This behaviour often occurs for several hours at a
time and typically at night. Despite therapeutic interventions these behaviours are stil occurring
and employment of an in-home support worker is not suitable.
Henry’s parents are constantly hyper-vigilant and preoccupied with attempts to reduce
behavioural outbursts. They find it difficult to find the time and energy to give enough attention
to their other two children or to each other. The situation is taking a significant toll on Henry’s
family members and their relationships.
The family would like to include funding in Henry’s plan for regular short-term accommodation.
This wil allow his parents and siblings to strengthen their resilience and bond as a family by
spending time together. It is also intended to give Henry the opportunity to undertake new
activities and interact with other children guided by specialised professional carers.
Case study examples of respite supports – 10
Page 46 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
7.3 Access to the community for Jordan
Jordan, aged 13, lives with his parents and sister in a regional area. He has severe intellectual
and language delays and attention deficit hyperactivity disorder. He is unable to talk, has
behavioural concerns and needs constant supervision and help with daily living activities. Each
Saturday Jordan participates in a three-hour group activity that allows him to access the
community with his friends, develop social skil s and independence. The group meets in a town
that is one and a half hours’ drive from home.
Jordan’s parents have asked that the transport costs and a support worker to accompany him to
each group session be included in his plan. This wil enable them to have respite and to spend
time together and with their other child.
Without this support, one parent would need to drive Jordan to the activity and stay in the town
while he is participating. The NDIS planner could consider that the transport of this distance to a
community activity exceeds ordinary parental responsibilities, provides Jordan with an
opportunity to meet his goals and objectives while providing a break for his parents.
7.4 In home supports and personal care for Sami
Sami, aged 18, is the sole family carer for her mother, Sara, who has advanced multiple
sclerosis and suffers from severe depression. Sami manages the household duties, including
looking after her 10 year old brother, as her mother cannot. While Sara receives paid personal
care and some household assistance during the day until Sami comes home from school, she is
very often in pain and in need of assistance throughout the night. This seriously interferes with
Sami’s sleep. Sara feels very guilty about the situation and the negative affect it is having on
Sami. This compounds her depression.
As well as paid carer support between the hours of 8.30am and 3.30pm on school days, Sara
would like funding in her NDIS plan for some over-night support during the week. This wil
relieve Sami from providing overnight care, improve her general wellbeing, and her capacity to
engage in education. This would also have a positive effect for Sara and her ongoing well-
being.
7.5 In home supports and personal care for Eleesha
Katerina is the primary carer of her three year old daughter Eleesha, who has a congenital heart
disease, stroke and developmental delay. Complications from her medical conditions have
resulted in the loss of a kidney, damage to her spleen and a reduced ability to fight infections.
Because of Eleesha’s susceptibility to infections she is becoming increasingly isolated with little
interaction with anyone other than her parents. Katerina is also feeling isolated. However, while
Case study examples of respite supports – 11
Page 47 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
Eleesha would benefit from the opportunity to develop independence and social skil s ordinarily
provided by attending child care, she is unable to attend a child care centre because contact
with other children increases her risk of infection.
Katerina would like Eleesha’s NDIS plan to include funding for regular in-home support. This
would have the benefit of providing Eleesha with the opportunity to interact with people other
than her parents and develop social skil s, as well as enabling Katerina to have some time for
herself. Katerina is also considering returning to part time employment.
Case study examples of respite supports – 12
Page 48 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Carers Disability Snapshot
8 Helpful links
• While the section on the NDIS and carers on the Carers Australia website is primarily
designed to help carers understand the NDIS, it is also a useful resource for NDIA staff
and partners to understand the carer’s perspective.
• Carers Australia Carer Checklist. Carers are encouraged to fil out this checklist prior to
engaging with the planning process. It also provides planners with some useful insights
into the range and diversity of supports which carers provide and the ways in which
caring can impact on their own lives and wellbeing. It may be useful to provide the
checklist to carers and family members to help them prepare for a planning meeting.
• Carer Statement examples. These may help planners understand why in some cases it
may be important for both the participant and the NDIA for carers to have an
opportunity to tell their own story without having to do so in front of the participant.
o Carer statement
o Primary carer’s statement
• How to speak NDIA guide on the Endeavour Foundation website. This can assist in
understanding some of the communication problems which arise between NDIA
professionals, participants and their carers.
Helpful links – 13
Page 49 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 5
Cerebral palsy Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:10:27
Page 50 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
Table of Contents
1 What is cerebral palsy? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 Different types and measures for describing cerebral palsy . . . . . . . . . . . . . . . . . . . . . 5
3 Common characteristics and impacts of cerebral palsy . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 Common misconceptions about cerebral palsy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
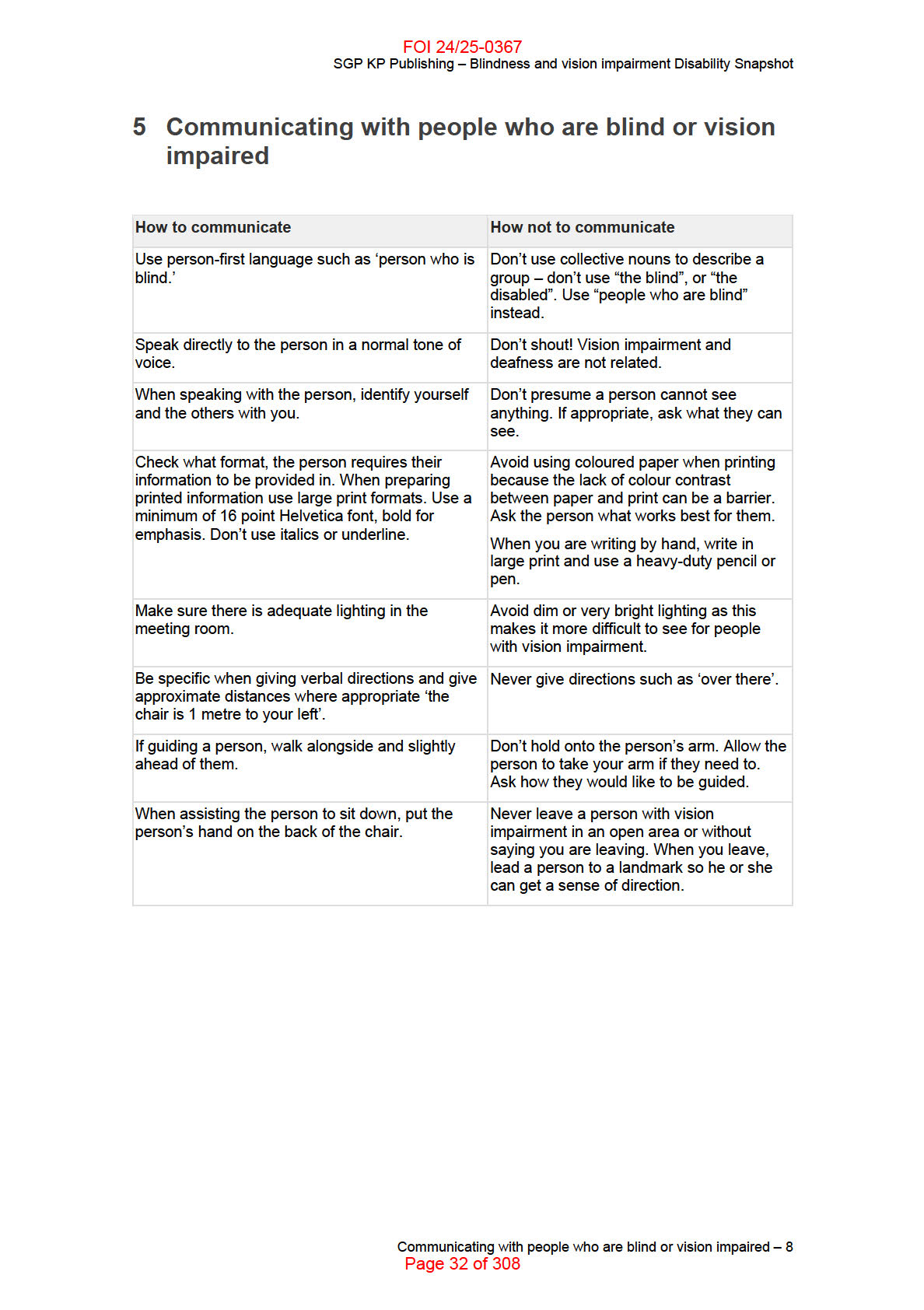
5 Language and terminology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 Enabling social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
7 Families and carers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
8 How can I tailor a meeting to suit a participant with cerebral palsy?. . . . . . . . . . . . . . 11
9 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13
10
Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14
Table of Contents – 2
Page 51 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
This Disability Snapshot provides general information about cerebral palsy to assist you in
communicating effectively and supporting the participant to develop their goals in a planning
meeting. Each person is an individual and wil have their own needs, preferences and
experiences that wil impact on the planning process. This information has been prepared for
NDIA staff and partners and is not intended for external distribution.
What is cerebral palsy? – 3
Page 52 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
1 What is cerebral palsy?
Cerebral palsy (CP) is a lifelong physical disability that begins in early childhood. It occurs in the
developing brain in pregnancy or in early childhood. It effects movement, posture, muscle
control and co-ordination of movement. Many people with CP may also have secondary
disabilities.
CP may change and its impact may become more complicated over time but it is not a
degenerative condition. CP is the most common physical disability in children. There are
currently around 34,000 people living with CP in Australia and 1 in 500 Australian babies are
diagnosed with the condition.
CP can affect gross and fine motor skil s, as well as speech. This impacts on participation in
everyday activities. Although CP is lifelong and non-progressive, factors such as puberty,
ageing and weight gain may detrimentally impact a person’s function.
Specialists such as paediatricians or neonatal specialists can diagnose CP. General
practitioners (GPs) also frequently play a critical role in maintaining the daily functioning and
wellbeing of someone with CP. The complexity of CP means interventions from a variety of
specialists and allied health professionals are usually required to support participation in
everyday activities.
What is cerebral palsy? – 4
Page 53 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
2 Different types and measures for describing cerebral
palsy
The different types of CP include spasticity, involuntary muscle movements (dyskinesis),
writhing or repetitive movements (athetosis or dystonia) and involuntary coordination of
movements (ataxia).
CP can affect people in different ways:
• quadriplegia where both upper and lower limbs are affected. Often the torso and head
are also affected
• diplegia where the lower limbs are affected. The upper limbs may be only slightly
affected
• hemiplegia where only one side of the body is affected.
The Gross Motor Function Classification System (GMFCS) is the most commonly used
measurement tool for describing the severity of CP. This system has a 1-5 rating scale, with 1
being the least severe and 5 being the most severe. The GMFCS classifies the level of a
person’s function in terms of their ability to perform gross motor actions, including sitting,
standing, walking and running.
Different types and measures for describing cerebral palsy – 5
Page 54 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
3 Common characteristics and impacts of cerebral
palsy
Although everyone with CP is different, there are some commonalities, including:
• Many people with CP have a second or third disability or associated impairments such
as intellectual disability (50%), epilepsy (25%), hearing or vision impairment (10%),
speech impairment (25%), behaviour disorder (25%), incontinence (25%), sleep
disorder (20%) and saliva control problems (20%).
• Some people with CP have a mental health condition. Anxiety and depression are
common. Reasons for this are not the underlying physical disorder but the associated
psychological and social factors that may impact the individual.
• Many people with CP experience chronic pain (75%), particularly in adulthood.
• Most people experience a significant decline in physical functioning in adulthood.
Exercise, stretching and therapy help people maintain their strength and function.
• People with CP can have muscle weakness.
These additional impairments can have a greater impact than the CP itself and wil require
higher levels of support to enable someone to engage in everyday life. For example, a person
who does not have good hand function and a speech impairment, wil likely need assistive
technology to help them to communicate effectively.
Common characteristics and impacts of cerebral palsy – 6
Page 55 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
4 Common misconceptions about cerebral palsy
• Most people with CP can walk with minimal support. In fact, some individuals mobilise
with little or no support so their disability may go unnoticed by others.
o The misconception is ‘everyone with CP uses a wheelchair or walking aid’.
• Intellectual disability only affects 50% of people with CP. Some people with mild CP
have an intellectual disability and some
o The misconception is ‘everyone with CP has an intellectual disability’.
• Approximately 10-30% of cases have a genetic component, with 1% being familial
(multiple siblings have CP).
o The misconception is ‘CP is not a genetic condition’.
• CP is not progressive or a life-limiting condition. In rare cases where a person has
profound CP, associated risk factors may reduce their life expectancy.
o The misconception is ‘everyone with CP has a limited life expectancy’.
• Most adults with CP can have regular sex. In some cases, physical limitations, societal
attitudes and other social barriers may present challenges to sexual activity.
o The misconception is ‘people with CP cannot be sexually active’.
• People with CP have the same reproductive systems as everyone else. Women with
CP can expect to have typical pregnancies.
o The misconception is ‘people with CP cannot have babies’.
• Non-verbal people with CP are most likely able to understand you. An inability to
communicate verbally does not mean the person has an intellectual disability.
o The misconception is ‘everyone who is non-verbal and has CP also has an
intellectual disability and cannot understand me’.
• Some people with CP may appear unsteady if they have uncoordinated, shaky, walking
patterns.
o The misconception is ‘a person with CP appears to be drunk’.
• Everyone has the right to full citizenship and inclusion.
o The misconception is ‘people with CP belong together and away from their
community’.
Common misconceptions about cerebral palsy – 7
Page 56 of 308
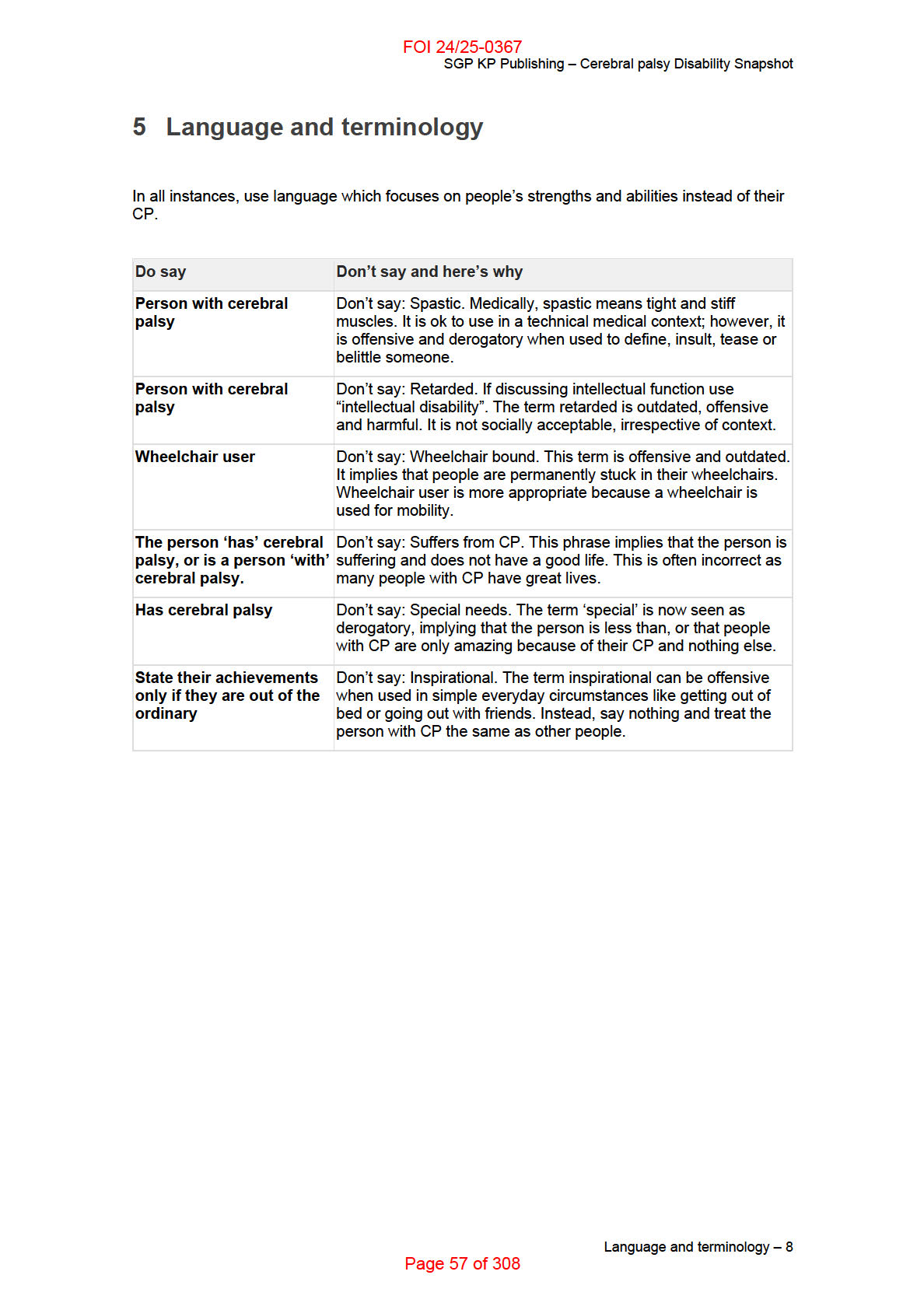
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
6 Enabling social and economic participation
It is important to explore how a person with CP can be supported to enable or maintain their
participation in mainstream activities, education and employment, taking into consideration their
interests and aspirations as an individual.
To enable and maintain work, ongoing supports or adjustments at work may be needed. This
might require NDIS funding for specialist disability or employment related assessment services.
Alternatively the person can access external employment retention and support initiatives such
as Work Assist provided by the Disability Employment Services (DES) program.
NDIS funding for personal care, assistance with travel or assistive technology may also be
required to support participation in the workforce.
If the person is preparing to enter the workforce, NDIS funded supports can assist people with
CP to build life skil s, capabilities and independence. Supports can be used to assist them
identify what their interests are and what work might be suitable. The supports can assist with
building specific work related skil s, manage barriers to work or develop a career plan.
Additionally, they can help prepare people with CP to connect with other government services
such as DES.
Enabling social and economic participation – 9
Page 58 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
7 Families and carers
Generally, the family of an individual with CP wil play a vital role in their physical, social and
emotional health for an extended period. A family’s ability to provide these supports wil vary
based on their own physical and mental health, work responsibilities, parenting capacity,
resilience and whether the parent has a disability themselves.
Family members of a person with CP are usually quite involved in providing direct support with
personal care, daily living, assistive technology, implementing therapy, teaching and supporting
communication, study and work, as well as attending medical and allied health appointments.
This is often beyond the age you would generally expect a parent or family member to provide
support.
Family members are often expected to advocate for their family member with CP, which is not
always possible. Family members may feel disempowered, exhausted and lacking in confidence
to challenge systemic barriers and mainstream services where supports are inadequate.
Supports including respite for family members can be critical to maintaining their own health and
wellbeing and allowing them to continue providing informal supports.
Supporting and considering holistic family needs, as well as other informal supports is important
when working with an individual with CP. This means the individual and those important to them
can function at their best.
Families and carers – 10
Page 59 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
8 How can I tailor a meeting to suit a participant with
cerebral palsy?
Every person with CP is unique and has different needs, wants, likes and dislikes. This means
people with CP wil have varied support requirements.
Before the meeting
• Ask if there are any accessibility requirements to consider.
• Check if the meeting place meets the participant’s needs. (For example, if the
participant is a wheelchair user the meeting place should have a ramp and/or elevator
and spacious disabled toilet with a railing).
• Consider the time of day and duration of the meeting. It can take a number of hours for
a person with CP to get up, dressed and ready to leave their home. Travel is also often
more complex.
• People with CP may require breaks during meetings. Some people become fatigued
easily and others with an intellectual disability may be overwhelmed with complex
information. Consider the length of the meeting and ask what time of day suits them
best.
• Ask the person if they require additional supports to understand information (such as
pictographs or sign language). Check if the person has a hearing or vision impairment
which may impact on how they need to receive information.
• Check to determine whether the participant wil be bringing an advocate or support
person with them.
• Provide as much information as possible about the purpose of the meeting ahead of
time, as they may need to discuss and prepare their responses with their support
person. People using a speech generating device to communicate may need to prepare
messages and store them in their device before the meeting.
• Provide any written material in plain English or Easy Read well before the meeting if
this is required.
Communication during the meeting
• It’s important to remember each person is different in their communication and the
support they might need. Approximately 25% of people with CP have challenges with
verbal communication. They may have sensory issues that affect their vision or hearing,
which may also affect their language and speech. They may have an intellectual
disability with difficulty in planning how to say complex sentences. People with CP may
have speech that is difficult to understand.
• When speaking, use appropriate volume and speed. Speak to the person directly and
observe how those known to the person communicate with them. Listen to the person
and clarify understanding.
• Check if the person has a personal communication system such as a communication
book, board, iPhone, iPad or speech generating device. If they do, ensure you give
them enough time to respond, ask questions and interact during the meeting.
• Don’t assume people who have communication difficulties have intellectual disabilities.
They may not use speech to communicate but may stil be able to understand
How can I tailor a meeting to suit a participant with cerebral palsy? – 11
Page 60 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
everything you say. When communicating with someone with CP where speech may be
affected, speak normally and use age appropriate language.
• If the person has an intellectual disability, use short sentences and provide pauses to
give the person enough time to hear and process what you are saying. Avoid using
jargon.
• If the person has speech which is difficult to understand, you may need to ask them to
repeat what they are saying. Speaking can require great effort for people with CP, so
repeat what you have understood so the person can concentrate on saying the part you
did not understand. If the person has repeated themselves several times and you are
stil unable to understand them, try alternative ways to communicate such as using a
gesture, communication board/device or pointing to an alphabet display.
• Speak as you usually would. Be aware it may take a while for someone to verbalise
what they want to say. Do not correct them or jump ahead or make assumptions about
what they are trying to say. Some people may use informal methods to communicate,
including facial expression, gestures, body language and behaviour.
• Understand some people may need more meetings to discuss everything.
How can I tailor a meeting to suit a participant with cerebral palsy? – 12
Page 61 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
9 Peak body consulted
The following organisations assisted in the development of this resource:
• Cerebral Palsy Support Network (members and staff)
• Cerebral Palsy Education Centre
• Members of the AusACPDM
• Melbourne Disability Institute
• The Royal Children's Hospital (Victoria)
• Centre of Research Excellence - CP
• Murdoch Children’s Research Institute
• Victorian Paediatric Rehabilitation Service
• CP Australia
• CP Al iance/Al iance Research Institute NSW
• CPL QLD
• Ability Centre WA
• Novita/Scosa SA
• Australian Catholic University.
Peak body consulted – 13
Page 62 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Cerebral palsy Disability Snapshot
10 Helpful links
• Cerebral Palsy Support Network
Helpful links – 14
Page 63 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 6
Deafblind Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:10:47
Page 64 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
Table of Contents
1 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 What is deafblindness? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 How many people are deafblind? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 Types of deafblindness . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
5 What are the characteristics of deafblindness? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 Psychosocial impact of deafblindness . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
7 Communication . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
8 Enabling social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
9 How can I tailor a meeting to suit a participant with deafblindness?. . . . . . . . . . . . . . 12
10
Communication access and supports . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13
11
Written communication . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14
12
Aids and equipment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15
13
Technology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16
14
Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
Table of Contents – 2
Page 65 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
This Disability Snapshot provides general information about deafblindness to assist you in
communicating effectively and supporting the participant to develop their goals in a planning
meeting. Each person is an individual and wil have their own needs, preferences and
experiences that wil impact on the planning process. This information has been prepared for
NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 66 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with the peak body representing people with this
disability, Deafblind Australia.
Peak body consulted – 4
Page 67 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
2 What is deafblindness?
Deafblind is a term used when a person has a combination of both impaired vision and hearing.
Dual sensory loss or dual sensory impairment are other terms used to describe deafblindness.
Deafblindness is described as a unique and isolating sensory disability having both hearing and
vision loss or impairment. The disability can have a significant effect on communication,
socialising, connecting with others, mobility and daily living (Deafblind Australia, 2004).
A person with deafblindness may strongly identify with the blind culture or the deaf culture (or in
some cases, neither) as well as the culture of their family. An understanding of the complexity of
each person’s culture is important to respectfully establish communication, language and
learning.
What is deafblindness? – 5
Page 68 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
3 How many people are deafblind?
• Studies have reported 0.2% to 3.3% of the population may be deafblind.
• In Australia nearly 100,000 people are reported to be deafblind and two-thirds of these
people are over the age of 65 years.
• One study reported 36% of individuals over the age of 85 years are deafblind.
How many people are deafblind? – 6
Page 69 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
4 Types of deafblindness
Congenital deafblindness is a term used when a person is born deafblind or when their
combined hearing and vision impairment exists before any form of language or communication
has developed.
Congenital deafblindness can occur due to:
• hereditary or genetic conditions
• infection contracted by the mother during pregnancy
• disease
• infection or injury that affects a child early in their development.
Acquired deafblindness is a term used when a person:
• is born deaf or hard of hearing and later in life experience a deterioration in their vision
• has deafness or hearing impairment at birth and has vision impairment later in life
• is born with a vision impairment or blindness and has hearing loss later in life
• has vision and hearing that deteriorates at a later stage in their life through accident,
injury or disease
• experiences deafblindness through the ageing process.
Types of deafblindness – 7
Page 70 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
5 What are the characteristics of deafblindness?
• A small number of people wil have no sight and no hearing.
• Other people who are deafblind wil have varying degrees of vision impairment and of
hearing impairment.
• Experiences and understanding of their world wil be different depending on whether a
person was born deafblind or if they acquired vision and hearing loss through
deterioration later in life.
• Becoming used to new environments and travelling independently and safely are
challenges.
• Communication is a key challenge for all people with deafblindness.
• Balance issues may affect some people with deafblindness, particularly those with
Usher Syndrome type 1. These balance issues can affect a person’s mobility.
What are the characteristics of deafblindness? – 8
Page 71 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
6 Psychosocial impact of deafblindness
The impact of deafblindness on a person’s life wil vary. The impact on a person who has a
severe vision and hearing impairment can be significant.
Depression, anxiety, frustration, and boredom can occur from the isolation and other challenges
experienced by people with deafblindness. A person with this diagnosis may experience low
self-esteem and lack of confidence to move about independently and carry out daily tasks.
Psychosocial impact of deafblindness – 9
Page 72 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
7 Communication
People with deafblindness are a very diverse group because of the varying degrees of their
vision and hearing impairments. Some people who are deafblind may also have other
disabilities. A wide range of communication methods might be used, including:
• speech, oral and aural communication (communication using verbal and non-verbal
signals)
• various forms of sign language including tactile and deafblind fingerspelling alternative
and augmentative communication (adding to communication often through devices like
tactile feeling boards, use of signs and gestures)
• print and brail e.
Do not assume all people who are deafblind communicate in the same way as they may use
one primary form of communication or a combination of these. Some people who are deafblind
(and people who are blind) use social haptics, a form of communication which involves touch
signals on the body.
Because of the wide range of communication methods, it can be difficult for another person to
know how to communicate with a person who is deafblind. Many organisations fail to recognise
communication needs and preferences for people who are deafblind. This is especial y the case
when arranging the most appropriate interpreter. Different types of interpreters can be needed,
for example tactile or Australian Sign Language (Auslan).
You need to be aware of, and have confidence to ask the person who is deafblind about their
communication requirements. A person who is deafblind is often familiar and comfortable in
explaining how they prefer to communicate.
Communication – 10
Page 73 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
8 Enabling social and economic participation
A person’s support needs for social and economic participation wil vary depending on their
areas of strength and level of function. It is important to explore how a person with deafblindess
can be supported to enable their participation in mainstream activities, education and
employment, taking into consideration their interests and aspirations as an individual.
This may include using supports to assist a person through a vocational ‘discovery’ process to
explore their strengths and interests in the context of work. For those who have acquired
deafblindess later in life, re-exploring their strengths and interests wil be important.
Individual supports can enable participants with deafblindness to build life skil s capabilities and
greater independence; including in the work place. Volunteering can be a first step in building
confidence and connecting to the community and the idea of employment. Peer support from
other people with deafblindness can also play a key role in improving social and economic
participation.
To maintain work, ongoing support and customisation of work tasks to match the level of
function should be considered, along with any needs related to personal care in the work place
or assistance with travel. Supports should take into account the degenerative nature of some
people’s sensory abilities and mobility. This might require NDIS funding for specialist disability
or employment related assessment services as well as access to employment retention and
support initiatives such as Work Assist provided through the Disability Employment Services
(DES) program. If regular, intensive ongoing support is required to assist a participant with
deafblindness maintain meaningful participation in the workplace, supported employment
supports could be considered.
Assistive technology or interpretation may also be required to support participation in work.
Enabling social and economic participation – 11
Page 74 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
9 How can I tailor a meeting to suit a participant with
deafblindness?
Consider the following for face to face communication:
• ask the person who is deafblind about their communication requirements and book the
most appropriate interpreter/s. For information on deafblind interpreters refer to
Communication access and supports below
• face the person and make eye contact
• identify yourself verbally and/or by signing. Say your name
• physically touch the person on the shoulder or elbow. The sense of touch is a core
communication means for people who are deafblind. However each person has their
own preference and sensitivity in terms of being touched. Ask each person their
preference.
If the person has a preference for touch as a method of communication, you may find it
beneficial to softly touch the back of your hand on the back of the person’s hand or arm to
ensure they are aware of you and are ready to communicate.
A lack of response by a person who is deafblind should not be considered as being rude, but
rather as a sign of ineffective communication. This would also be the case if a person who is
deafblind moves away from the speaker.
Observe the facial expressions of the person who is deafblind – an expression suggesting worry
can indicate confusion or unhappiness with the type and effect of the communication.
Conversely, a person who is deafblind might interpret the other person’s message and
intentions by the person’s body language. So, friendly and open body language wil aid effective
communication.
How can I tailor a meeting to suit a participant with deafblindness? – 12
Page 75 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
10 Communication access and supports
People who are deafblind can live independent lives and may travel with CommGuides.
CommGuides are specialised support workers that understand the needs of deafblindness.
They facilitate independent community participation through communication support and guiding
support.
Deafblind interpreters are important to ensure people who are deafblind receive information and
communicate effectively in more complex situations such as attending appointments and
professional services.
A CommGuide can also be used for communication support during short informal interactions
such as at the shops or at the gym. However, for any formal meetings or workshops an
interpreter should be booked. In many instances two interpreters wil be required depending on
the length of the meeting and the potential need for tactile signing.
Communication access and supports – 13
Page 76 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
11 Written communication
Some people who are deafblind have not received appropriate support to access education and
may require additional assistance with literacy and numeracy tasks. It is also important to note
that for people who are deafblind and have Auslan as their first language, English is a second
language.
Plain language should always be used. It should be simple, clear and straight to the point.
Explain the context of the communication and keep it focused and relevant. Increase
understanding by using examples. Avoid slang, acronyms and bureaucratic language.
Written communication – 14
Page 77 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
12 Aids and equipment
There are a variety of aids and equipment which many people with deafblindness require to
access communication, information and their environment. Common aids and equipment used
by people with deafblindness include:
• Hearing aids and Cochlear implants
• Wireless microphones with Blue Tooth (Roger Pens)
• White mobility canes
• Seeing eye dogs
• Home/personal alert systems
• Magnifiers, such as Zoom text
• Jaws screen reader
• Closed circuit televisions
• Smart phone with accessibility apps (sometimes paired with brail e display)
• Brail e devices and displays (Brail e watches)
• Smart watches with accessibility apps including haptics
• Vibration devices such as ‘Ditto’.
Aids and equipment – 15
Page 78 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
13 Technology
Technology is very important to people with deafblindness. Technology can assist with
communication, social and community engagement, access to information and education,
transport assistance (GPS), safety in the home and community and activities of daily living.
The following accessibility considerations may support a person to be able to access content on
websites:
• adjustable font sizes
• contrasting colours
• accessibility for screen reading software
• plain language
• image descriptions – text format screen readers do not pick up images, so picture
description is required.
Technology – 16
Page 79 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafblind Disability Snapshot
14 Helpful links
• Deafblind Australia
• Deafblind Information website
Helpful links – 17
Page 80 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 7
Deafness and Hearing Impairment
Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:11:21
Page 81 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
Table of Contents
1
Peak body consulted ........................................................................................................... 4
2
What is deafness and hearing impairment? ...................................................................... 5
3
Common characteristics ..................................................................................................... 7
4
Common misconceptions about deafness and hearing impairment ............................. 8
5
Language and terminology ................................................................................................. 9
6
Enabling social and economic participation ................................................................... 10
7
How can I tailor a meeting to suit people who experience Deafness or hearing
impairment? ............................................................................................................................... 11
8
Helpful links ........................................................................................................................ 13
Table of Contents – 2
Page 82 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
This Disability Snapshot provides general information about deafness and hearing impairment
to assist you in communicating effectively and supporting the participant in developing their
goals in a planning meeting. Each person is an individual and will have their own needs,
preferences and experiences that will impact on the planning process. This information has
been prepared for NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 83 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
1 Peak body consulted
In developing this resource we consulted with Deaf Australia, Deafness Forum of Australia and
Deafblind Australia, peak bodies for people with deafness, hearing impairment or deafblindness.
Peak body consulted – 4
Page 84 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
2 What is deafness and hearing impairment?
Deaf, deafness, hard of hearing, hearing loss, and hearing impairment are all terms used to
describe the sensory disability that affects a person’s ability to hear.
Levels of deafness vary from mild to profound and can occur at birth or at any age regardless of
a person’s gender or background. However, it can become more common as age increases.
The terms deafness and hearing impairment mean different things to different people and must
be used sensitively. Deaf is the preferred term used by people who use Australian Sign
Language (Auslan) as a primary or preferred communication method and who identify
themselves as a member of the signing Deaf community. It is used to describe their unique
cultural identity which is a result of their rich visual language and is used with pride. In this case
the D in Deaf is capitalised.
Many in the Deaf community regard the terms ‘hearing impairment’ and ‘hearing loss’ as
alienating and damaging because it implies deafness needs to be ‘fixed’.
Because of the sensitivities around the different terms, it is particularly important that
participants are encouraged to take the lead in describing themselves and their disability or
cultural identity. Care needs to be taken to ensure that the terminology preferred by the
participant is consistently used in all meetings and correspondence. See the language and
terminology section of this Disability Snapshot for further detail.
People who are deafblind have specific needs beyond deafness and blindness. Their
communication and mobility requirements will be highly specialised and often require one-on-
one supports. See the separate Deafblind Snapshot for further detail.
How are deafness and hearing impairment diagnosed?
Australia has a system of universal, hearing screening for newborns in all hospitals. When
deafness or hearing impairment is identified, a referral is made for the newborn to be assessed
by a diagnostic audiologist.
In some states, hearing testing is done in primary schools. People can also be referred to an
audiologist by their GP, health provider or family members.
Approximately 95% of children born with hearing loss are born to parents who can hear and
speak. These parents may have no prior knowledge of deafness or hearing impairment. They
may experience a range of emotions and not fully understand the implications of the diagnosis.
A number of children may have multiple disabilities, including deafness or hearing impairment.
These children will need a range of supports to address their different needs.
People may acquire hearing loss through a wide range of causes such as illness, accident,
exposure to loud damaging noise and the natural process of ageing. Often it is a family member
that notices the hearing loss and encourages the person to seek professional advice.
What is deafness and hearing impairment? – 5
Page 85 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
Australian Hearing is the only provider in Australia who receives government funding to deliver
hearing services (including the fitting of hearing devices) for children and young adults (under
26 years of age). Australian Hearing do not do diagnostic testing. Once a child has a confirmed
hearing loss they are then referred to Australian Hearing.
What is deafness and hearing impairment? – 6
Page 86 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
3 Common characteristics
Lack of access to communication and information is the primary barrier to inclusion and
wellbeing - communication and quality of life are very closely linked. Poor access to
communication and lower levels of interaction are known to negatively
impact on social,
emotional, psychological and physical wellbeing.
People who experience deafness and hearing impairment need access to a range of strategies
to access information and to communicate.
They may need to access several of the following supports and strategies:
listening and spoken language therapies in conjunction with assistive hearing
technologies
Auslan, the sign language used by the Deaf community in Australia
lip-reading (a specialised skill used by a small part of the population)
devices that amplify or replace sound (e.g. hearing aids, cochlear implants) and therapy
/ rehabilitative supports
hearing augmentation systems such as hearing loops, remote microphone systems,
soundfield systems and captioning
assistive visual devices and systems (for example flashing doorbells, telephones and
smoke alarms and live captioning).
For more information see Appendix A: technology as an enabler as the end of this document.
The most helpful approach to the provision of supports is to provide a person and their family
with as much information as possible to identify strategies that might work for them. It is not true
that people who are deaf only require Auslan interpreters, or that a single item of assistive
technology (AT) (for example a cochlear implant) is sufficient to resolve access to
communication and information.
It is important that planners, Local Area Coordinators and Early Childhood partners support
participants and their families to obtain independent recommendations for interventions and/or
AT from organisations that are independent of service provision.
Common characteristics – 7
Page 87 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
4 Common misconceptions about deafness and
hearing impairment
Hearing aids or cochlear implants can significantly reduce the disabling effects of
hearing loss although hearing loss is irreversible. The ability to hear and the ability to
understand sounds are two different things. People who wear hearing devices may still
have difficulty hearing in a noisy environment, on the phone or comprehending spoken
language and speech.
o A misconception is that hearing aids or Cochlear implants ‘fix’ or restore
hearing loss.
For many Deaf people, being deaf is an essential part of their identity which leads to
positive social, emotional and language developments. An assumption that intervention
is needed to fix the deafness needs careful consideration of each person’s choice,
communication needs and participation opportunities.
o A misconception is that deafness needs to be ‘fixed’.
Technology is usually most effective when combined with hours of learning to interpret
the device’s sounds. This may be with the support of a speech pathologist or teacher,
particularly during early childhood. Similar for all people with disability, intensive therapy
needs to be balanced with other important elements of life such as recreation time,
social interaction and general downtime.
o A misconception is that hearing devices immediately allow a person to hear.
Auslan (Australian Sign Language) is a visual and spatial language that has its own
grammar rule. It has no written form. Auslan is recognised as a language. Auslan is
different to English and does not translate directly. Sign language is not universal,
Auslan is a unique language used within Australia.
o A misconception is that Auslan is just a signed form of spoken English
language.
Lip-reading and listening skills are acquired through years of practice and training and
these skills vary widely. It is difficult and complicated because there are many different
speech sounds that look similar on the lips (for example ‘b’, ‘p’ and ‘m’). Lip-reading is a
tiring exercise - it requires high levels of concentration irrespective of the age of the
person.
o A misconception is that all deaf people can lip-read.
Common misconceptions about deafness and hearing impairment – 8
Page 88 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
5 Language and terminology
Terminology is a sensitive issue in the deafness and hearing impairment communities. NDIS
participants must be given the opportunity to describe themselves and their disability. Take care
to ensure the participant’s preferred terminology is always used in any meetings and
correspondence.
Preferred terms
Deaf, for a person whose first language is Auslan.
Person who is deaf and has other disability/s.
Description of terms
Deaf (with capital ‘D’) is the preferred term used by people who use Auslan as a
primary or preferred communication mode, and who identify themselves as a member
of the signing deaf community. This group of people may also identify themselves as
culturally Deaf. Auslan users have a unique language and experience, and like all
cultural and linguistic groups, English is their second language. Auslan users are more
likely to have been born deaf or have become deaf in early life. There are some who
discover Auslan later in life and then use it as their primary language.
deaf (with lower case ‘d’) is a general term used to describe people who have a
physical condition of hearing loss of varying degree, no matter which communication
mode they use (for example hearing devices, Auslan or lip reading).
The term ‘hearing impairment’ refers to a full or partial decrease in the ability to hear. It
is one of the commonly used terms to describe a person who has a hearing loss,
irrespective of their level of hearing. This term must not be used as a blanket term for
people who identify as ‘capital D’ Deaf. Some individuals may prefer to use hearing
impairment to describe their identity but many Deaf and hard of hearing people find this
term derogatory.
‘Hard of hearing’ is the internationally preferred term used to describe people with
acquired hearing loss in a way that does not imply impairment.
Language and terminology – 9
Page 89 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
6 Enabling social and economic participation
A person’s support needs for social and economic participation will vary depending on their
strengths and level of function. Identifying potential solutions for increasing access to
communication and information is critical. This could include arranging assistive technology or
Auslan.
To enable and maintain work, ongoing supports or adjustments at work may be needed. This
might require NDIS funding for specialist disability or employment related assessment services.
Alternatively the person may access external employment retention and support initiatives such
as Work Assist provided by the Disability Employment Services (DES) program.
Peer support from people who identify themselves as a member of the signing community or
with other people who are deaf can also assist to address challenges to social and economic
participation.
Enabling social and economic participation – 10
Page 90 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
7 How can I tailor a meeting to suit people who
experience Deafness or hearing impairment?
Offer a variety of options to contact you: email, fax, text message or letter. Some people
will nominate a TTY phone contact via the National Relay Service (NRS) as their
preference. Ensure you are familiar with the NRS before use.
o Do not use a phone call as the first point of contact. It is important to
communicate with people in the means which they find accessible and most
comfortable.
Always ask what communication access is needed for the meeting. This could be a
hearing loop, live captions, a room with Auslan interpreters or a combination of
supports.
o Do not impose unwanted supports. Interpreter and captioners preferences must
be respected. NDIS meetings often include a lot of information and may be
quite overwhelming.
Book communication support as soon as possible and confirm the details with the
participant.
o Do not ask interpreters and captioners to provide advocacy or other support.
Their role is solely to interpret/caption all communication. There is a shortage of
Auslan interpreters, captioners are in high demand, and not all meeting rooms
have hearing loops.
Make sure meetings are held in a quiet space that is well lit.
o Do not presume that a busy office or café is a welcoming environment. A quiet,
well-lit space is a place where conversations can take place free of background
noise, strong background light and distractions.
Ensure that you are clearly visible and facing the person.
o Do not wave hands or hold other objects near your face while speaking. Some
people can read lips for some words.
Use normal clear speech at normal speed.
o Do not exaggerate your speech. Try not to speak too quickly, don’t mumble and
don’t yell. It’s clarity that counts. Hearing devices (including ears) work best
when they are receiving normal speech free of background noise. Some people
can read lips for some words.
Look at and speak directly to the person.
o It is always good manners to look at the person you are speaking to.
Use plain language that is clear. Rephrase as needed.
o Do not keep saying the same thing over again or assume that a person with
communication support needs has an intellectual disability because they have a
limited vocabulary or language difficulties.
Hearing devices might not pick up every word clearly. Remember that a person whose
first language is not English (this may include users of Auslan) might not have a high
English literacy level.
Have paper and pen available.
o Don’t rely on one communication method only. All people in the meeting need
to have the same understanding about key information, support requirements,
outcomes and next steps.
How can I tailor a meeting to suit people who experience Deafness or hearing impairment? – 11
Page 91 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
Ask for clarification and things to be reworded if you do not understand. Play it back to
check that both parties have the same understanding.
o Don't assume you know what the person is trying to say.
How can I tailor a meeting to suit people who experience Deafness or hearing impairment? – 12
Page 92 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Deafness and Hearing Impairment Snapshot
8 Helpful links
Deaf Australia
Deafness Forum of Australia
Aussie Deaf Kids
Better Hearing Australia
CICADA (Cochlear implantee group)
Parents of Deaf Children
Hearing Topics A – Z
The Meaning and Practice of Audism
Helpful links – 13
Page 93 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 8
Down syndrome Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:11:35
Page 94 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
Table of Contents
1 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 What is Down syndrome? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 Common misconceptions about Down syndrome . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 How is Down syndrome diagnosed? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
5 Language and terminology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 Enabling social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
7 Families and carers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
8 How can I tailor a meeting to suit a participant with Down syndrome? . . . . . . . . . . . . 12
9 Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13
Table of Contents – 2
Page 95 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
This Disability Snapshot provides general information about Down syndrome to assist you in
communicating effectively and supporting the participant in developing their goals in a planning
meeting. Each person is an individual and wil have their own needs, preferences and
experiences that wil impact on the planning process. This information has been prepared for
NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 96 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with Down Syndrome Australia.
Peak body consulted – 4
Page 97 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
2 What is Down syndrome?
Down syndrome is a genetic condition – it is not an il ness or disease. Down syndrome is the
most common genetic cause of intellectual disability. It occurs at conception as a result of an
extra chromosome. In Australia, around one in 1,100 babies are born with Down syndrome.
People with Down syndrome have:
• Areas of strengths and other areas where they need more support, just like everyone
else in the community.
• Some level of intellectual disability. The average IQ for a person with Down syndrome is
50, whereas two-thirds of the general population scores between 85 and 115.
• Some characteristic physical features, including a recognisable facial appearance and
short stature.
• Significant delays in gross motor skil s (whole-body movements like climbing and
jumping jacks), fine motor skil s (smaller muscle actions like picking things up between
thumb and finger) and speech development. Plus ongoing difficulties and support needs
in these areas.
• Increased risk of a range of health issues (which compound developmental delay and
can impact functional ability), including congenital heart defects, respiratory, hearing
and vision problems, childhood leukaemia, thyroid conditions, gastrointestinal issues,
and earlier onset of ageing. Average life expectancy is currently around 60.
• Increased risk of younger onset dementia, with more than 50 per cent of people with
Down syndrome having a diagnosis of Alzheimer’s disease by the time they are 60.
Dementia can be difficult to diagnose and needs to be addressed by a health
professional. There are a range of strategies and supports that can be put in place if a
person has dementia and Down syndrome.
• Increased likelihood of having other disabilities as well as Down syndrome. These can
include physical disabilities, sensory disabilities, psychosocial disability or other
conditions such as autism, ADHD and cerebral palsy. It is important to ensure that other
disabilities and the need for support are not discounted due to the person having Down
syndrome as their primary diagnosis. Sometimes, these other disabilities are the ones
the person needs the most support with.
What is Down syndrome? – 5
Page 98 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
3 Common misconceptions about Down syndrome
• ‘People with Down syndrome all look the same’.
o While people with Down syndrome usually have recognisable facial features,
each person looks more like their family than like other people with Down
syndrome.
• ‘People with Down syndrome can’t read, write or learn’.
o Every person is different and wil have different capabilities when it comes to
reading, writing and other skil s.
• ‘People with Down syndrome can’t communicate’.
o Some people with Down syndrome speak well, others can be more difficult to
understand and some may use little or no speech.
o Many who have difficulty in speaking wil understand what is said to them.
o Some may need more time to communicate or use communication devices to
help them have a conversation.
• ‘People with Down syndrome are childlike’.
o Adults with Down syndrome are adults and should be respected and treated as
such.
• ‘People with Down syndrome are always happy and loving’.
o People with Down syndrome experience the same range of feelings and moods
as anyone else.
• ‘People with Down syndrome can’t live an independent life’.
o People with Down syndrome can live independently. Some own their own
homes and don’t need much support, others need more support and the kinds
of support wil differ for each person.
• ‘People with Down syndrome are better off in segregated settings’.
o In the past, many supports such as ‘special’ schools, sheltered workplaces and
group homes were provided in separate places. Evidence suggests children
with Down syndrome do better in inclusive education and adults with Down
syndrome can work in regular workplaces and live in ordinary homes in the
community. It’s just about providing the support each person needs in different
places.
Common misconceptions about Down syndrome – 6
Page 99 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
4 How is Down syndrome diagnosed?
Diagnosis is often made prenatally by sampling foetal cells to analyse the foetal chromosomes.
After birth, Down syndrome is often identified based on the baby's appearance. The diagnosis is
confirmed through a test called a chromosomal karyotype. Using a sample of blood, this test
analyses the child's chromosomes. If there is an extra chromosome 21 in all or some cells, the
diagnosis is Down syndrome.
How is Down syndrome diagnosed? – 7
Page 100 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
5 Language and terminology
‘Person first’ language should be used to describe Down syndrome. This means, for example,
saying ‘person with a disability’ or ‘man with Down syndrome’.
Language and terminology – 8
Page 101 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
6 Enabling social and economic participation
A person’s support needs for social and economic participation wil vary depending on their
areas of strength and level of function. It is important to explore how a person with Down
syndrome can be supported to enable their participation in mainstream activities, education and
employment, taking into consideration their interests and aspirations as an individual.
This might include:
• support to access mainstream sporting groups, dance groups or other activities
• supports to build capacity to participate in mainstream education settings
• social and community participation supports tailored to build ‘soft skil s’ for employment
• travel training
• supports to facilitate participation in mainstream employment and
• supports to build capacity for independent living.
Barriers to social and economic participation A Down Syndrome Australia survey found that people with Down syndrome experience
significant barriers to social and economic participation.
Barriers to inclusion and participation include:
• discriminatory attitudes
• lack of understanding about Down syndrome and how to support inclusion
• bullying in schools and workplaces
• lack of accessible information (including in government services, the community,
employment and schools)
• exclusionary educational systems, settings and practices
• difficulty accessing employment
• lack of support for transition between school and adult life
• difficulty accessing vocational education and skil s training
• lack of suitable jobs (including accessibility issues and lack of flexibility)
• lack of workplace support including recruitment and ongoing support
• housing and lack of support to live independently from family
• inadequate support services to help build skil s and capacity and make community
connections
• getting to work or community activities.
Supporting social and economic participation
Enabling social and economic participation – 9
Page 102 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
NDIS funding can support people with Down syndrome to build life skil s, capabilities and
independence. It can give them a greater understanding of what their interests are and what
work might be suitable. It can also assist them build specific work related skil s which could
support them to engage with other government services such as Disability Employment
Services (DES).
While some NDIS participants with Down syndrome may build their capacity and successfully
participate in DES, many may need more intensive, regular, ongoing support in the workplace to
help them meaningfully participate at work. This support is generally provided by Australian
Disability Enterprises (ADEs).
In some instances work adjustments or NDIS funding for specialist disability assessment
services can help create opportunities for jobs to be adapted to meet the capabilities and
strengths of the individual.
Also consider the need for personal care support or assistance with travel in the work place.
Enabling social and economic participation – 10
Page 103 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
7 Families and carers
Families provide different levels of support to a person with Down syndrome, but usually play an
active role in providing a range of supports including assisting with daily living tasks, advocating
for inclusion, and working to find employment. Families usually have a good understanding of
the support the person needs to participate in the community and improve their independence.
While families are usually happy to provide some support, it can affect their own employment,
ability to meet the needs of other family members, and their own needs and health, especially
as they age.
It is not reasonable to expect a family to be the main source of support for an adult with Down
syndrome. It is important to consider for children and adults whether the level of informal
support being provided is sustainable and what impact it has on the family.
Families and carers – 11
Page 104 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
8 How can I tailor a meeting to suit a participant with
Down syndrome?
Every person with Down syndrome is unique with individual personality, strengths and areas
where they need support. It’s important to remember that each person is different in their
communication and the support they might need. Some key suggestions to support
communication include:
• Get in touch before the meeting and ask what support they need to access and take
part in the meeting.
• Provide any written material in Plain English or Easy English if required well before the
meeting.
• Provide as much information about questions and things that wil be discussed at the
meeting ahead of time. This wil give the person with Down syndrome an opportunity to
discuss these questions with their support person and to have time to consider their
responses.
• Always communicate and engage directly with the person with Down syndrome, not the
person with them. Be patient and take their lead regarding whether the person with
them helps them communicate.
• Speak respectfully in an age appropriate way. Don’t treat an adult with Down syndrome
as if they are a child.
• It can help to use visual information to help explain some concepts and messages. This
could be pictures or objects, such as a clock or calendar. Easy English information can
be used to help with discussion.
• Al ow the person additional time to respond to questions where needed.
• Consider arranging a second planning meeting to ensure all elements are covered.
How can I tailor a meeting to suit a participant with Down syndrome? – 12
Page 105 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Down syndrome Disability Snapshot
9 Helpful links
• Down Syndrome Australia
Helpful links – 13
Page 106 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 9
Fetal Alcohol Spectrum Disorder
Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:11:52
Page 107 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fetal Alcohol Spectrum Disorder Disability Snapshot
Table of Contents
1
Peak body consulted ........................................................................................................... 4
2
What is Fetal Alcohol Spectrum Disorder? ....................................................................... 5
3
How is Fetal Alcohol Spectrum Disorder diagnosed? ..................................................... 6
4
Language and terminology ................................................................................................. 7
5
Enabling social and economic participation ..................................................................... 8
6
Families and carers .............................................................................................................. 9
7
How can I tailor a meeting to suit a participant with Fetal Alcohol Spectrum
Disorder? .................................................................................................................................... 10
8
What people with Fetal Alcohol Spectrum Disorder want you to remember ............... 11
9
Helpful links ........................................................................................................................ 12
Table of Contents – 2
Page 108 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fetal Alcohol Spectrum Disorder Disability Snapshot
This Disability Snapshot provides general information about Fetal Alcohol Spectrum Disorder
(FASD) to assist you in communicating effectively and supporting the participant in developing
their goals. Each person is an individual and will have their own needs, preferences and
experiences. This information has been prepared for NDIA staff and partners and is not
intended for external distribution.
Peak body consulted – 3
Page 109 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fetal Alcohol Spectrum Disorder Disability Snapshot
1 Peak body consulted
In developing this resource, we consulted with:
Developmental
Disability
WA
Dr Amanda Wilkins, a Developmental Paediatrician experienced in diagnosing FASD
and who was involved in establishing FASD C.A.R.E Inc
Dr Robyn Williams, a Nyoongar woman who completed her PhD on FASD in the south
west region of Western Australia
National Organisation for
Fetal Alcohol Spectrum Disorder (NOFASD) Australia.
Peak body consulted – 4
Page 110 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fetal Alcohol Spectrum Disorder Disability Snapshot
2 What is Fetal Alcohol Spectrum Disorder?
Fetal Alcohol Spectrum Disorder (FASD) is a term that describes the impacts on the brain and
body of a person exposed to alcohol during pregnancy. It is a lifelong disability and people with
FASD will experience challenges in their daily living. Each person with FASD is unique and will
experience their own strengths and challenges.
To reach their potential they may need support with:
motor
skills
physical
health
learning
memory
attention
communication
emotional
regulation
social
skills.
Some children with FASD may have shorter than average height, low body weight and a small
head size. They may also appear hyperactive and have poor coordination.
It is common for people with FASD to be able to express themselves but may have difficulty
understanding, processing and retaining information.
What is Fetal Alcohol Spectrum Disorder? – 5
Page 111 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fetal Alcohol Spectrum Disorder Disability Snapshot
3 How is Fetal Alcohol Spectrum Disorder diagnosed?
FASD is usually diagnosed by a multi-disciplinary team which may include paediatricians,
psychologists, speech/language pathologists or occupational therapists. When assessing for
FASD, a clinician will consider:
the person’s history and presenting concerns from an obstetric, developmental,
medical, mental health, behavioural, and social point of view
any diverse features such as unusually shaped or sized head or facial features and
other major/minor features present at birth
whether the child may have been exposed to alcohol during and after pregnancy
any known medical conditions including genetic syndromes and other disorders
the growth of the person.
Only 1 in 10 children with FASD will have identifiable facial features. Children with FASD will still
have significant developmental impairments even if they do not have physically identifiable
features.
An early diagnosis may lead to better outcomes for a child living with FASD. If a child receives
early intervention and support, they may be less likely to develop other behaviours and issues in
adulthood and the ongoing impact of the condition may be less severe.
How is Fetal Alcohol Spectrum Disorder diagnosed? – 6
Page 112 of 308
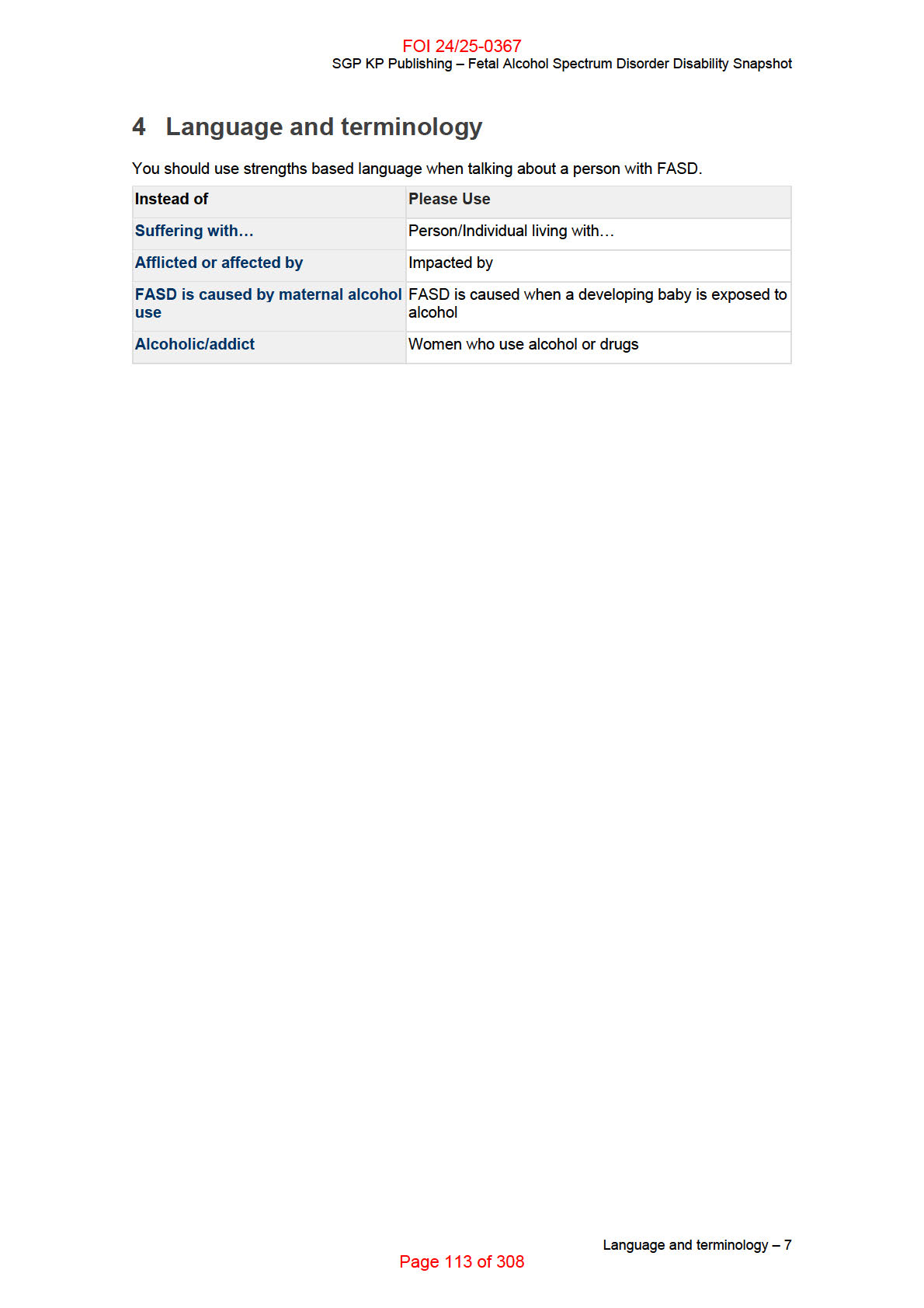
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fetal Alcohol Spectrum Disorder Disability Snapshot
5 Enabling social and economic participation
Therapy and support services can be beneficial to enable social and economic participation for
people with FASD. Supports will vary depending on the age and circumstances of the
participant. Children under 7 years with FASD will be supported by the Early Childhood Early
Intervention approach. Some young children may present with global developmental delay,
before they have a formal diagnosis of FASD.
Common therapy supports include speech therapy and occupational therapy. People with FASD
may also benefit with support from counsellors who are experienced in working with the
disorder.
They may support people with FASD with:
developing and improving communication, comprehension, and literacy skills
learning social skills to develop and maintain friendships at school and in the
community, and protect against isolation
improving their memory and ability to process information
capacity building in concepts such as planning, time, money and problem solving
participation in programs to support self-regulation, emotional regulation and calming
responses such as the “Zones of Regulation” program
sensory
processing
skills
daily living skills such as dressing, tying shoelaces, and writing
education support and instruction for maths and other subjects
developing social, educational and emotional maturity.
Enabling social and economic participation – 8
Page 114 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fetal Alcohol Spectrum Disorder Disability Snapshot
6 Families and carers
Families can provide different levels of support to a person with FASD. They assist with daily
living tasks and encourage the participant to find a job. Family members may have a good
understanding of the support the person needs to participate in the community and work
towards independence.
While families are usually happy to provide support, it can impact their own employment, the
needs of other family members, and their own needs and health – especially as they age. It is
important to consider, for children and adults, whether the level of informal support being
provided is sustainable and how it may impact the family.
Biological mothers of children with FASD may experience guilt or concern that they will be
blamed for the disorder. It is important not to make assumptions about how or why an individual
was exposed to alcohol during pregnancy. Many mothers of children with FASD do not have
problematic patterns of alcohol use, may have been unaware of the early pregnancy and are
not neglectful parents. They may feel frustration at the attitudes of health care providers toward
them. This can affect their confidence in their ability to parent a child who already faces many
challenges.
Families and carers – 9
Page 115 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fetal Alcohol Spectrum Disorder Disability Snapshot
7 How can I tailor a meeting to suit a participant with
Fetal Alcohol Spectrum Disorder?
Every person with FASD is unique and has their own individual personality, strengths and areas
where they need support. It is important to remember that each person will have different
needs.
You can tailor a meeting to suit the participant by:
giving the person time to think about their answer and respond – some people will need
more time than others
asking questions to make sure the person understands you – don’t assume the
person’s response means they have understood
communicating in short, simple sentences and using Plain English
keeping the number of people in a meeting to a minimum as the participant may be
overwhelmed with too many people
having shorter meetings, with follow ups if necessary, to get relevant information across
reducing distractions such as visual distraction, background noise and artificial lighting if
possible
giving the person information about what will be discussed at the meeting ahead of time
to give them an opportunity to consider responses and prepare with a support person
communicating and engaging directly with the person with FASD, not just their family
member, carer or another person who attends the meeting with them
speaking respectfully in an age appropriate way
visual information can be helpful to explain some concepts and messages, such as
pictures or objects like a clock or calendar
using Easy English written information to help with discussion
writing the discussion points in simple dot point format and include any decisions made,
this will be a helpful memory aid for a person with FASD.
How can I tailor a meeting to suit a participant with Fetal Alcohol Spectrum Disorder? – 10
Page 116 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fetal Alcohol Spectrum Disorder Disability Snapshot
8 What people with Fetal Alcohol Spectrum Disorder
want you to remember
Children with FASD may engage in behaviours that look like lying and can make poor
decisions. This can mean young people with FASD are more likely to be involved in the
justice system. The desire to please and difficulty remembering can have a significant
impact in these situations.
An individual with FASD may experience difficulties with impulse control, understanding
consequences of actions and risks. This results from impairments in memory and poor
connection between emotional and logical thought.
Engaging in social interactions can be difficult for people with FASD, and if people
behave differently to their expectations, they may respond by over-reacting or shutting
down.
Sometimes people with FASD may find it difficult to focus on, and give or maintain
attention to a person or task.
What people with Fetal Alcohol Spectrum Disorder want you to remember – 11
Page 117 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fetal Alcohol Spectrum Disorder Disability Snapshot
9 Helpful links
NOFASD Australia
FASD Hub Australia
DDWA - Supporting School-age Children with Fetal Alcohol Spectrum Disorder
Marulu Strategy
Practice Guide - Early Childhood Early Intervention
Guide - Conversation style guide
Helpful links – 12
Page 118 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 10
Fragile X syndrome Disability
Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:12:05
Page 119 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fragile X syndrome Disability Snapshot
Table of Contents
1 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 What is Fragile X syndrome? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 How is Fragile X syndrome diagnosed? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 Language and terminology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
5 Enabling social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 Families and carers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
7 How can I tailor a meeting to suit a participant with Fragile X syndrome? . . . . . . . . . 10
8 What people with Fragile X syndrome want you to remember . . . . . . . . . . . . . . . . . . . 11
9 Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12
Table of Contents – 2
Page 120 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fragile X syndrome Disability Snapshot
This Disability Snapshot provides general information about Fragile X syndrome to assist you in
communicating effectively and supporting the participant in developing their goals. Each person
is an individual and wil have their own needs, preferences, experiences and capacity. This
information has been prepared for NDIA staff and partners and is not intended for external
distribution.
Peak body consulted – 3
Page 121 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fragile X syndrome Disability Snapshot
1 Peak body consulted
In developing this resource, we consulted with Fragile X Association of Australia.
Peak body consulted – 4
Page 122 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fragile X syndrome Disability Snapshot
2 What is Fragile X syndrome?
Fragile X syndrome is a genetic disorder and is the leading worldwide contributor to inherited
developmental disability. It is caused by a mutation (change in DNA structure) on the X
chromosome. The FMR1 gene is responsible for producing a protein important for brain
development. When this gene lengthens through the mutation, it switches off production of the
protein involved in brain development and other functions.
Fragile X syndrome occurs in around 1:3600 males and around 1:4000-6000 females. Fragile X
syndrome is inherited from a female carrier of the FMR1 gene premutation. A premutation
carrier does not have Fragile X syndrome, but may have mild expressions of some traits such
as anxiety, social avoidance and difficulty with planning and organisation.
Men and women can be carriers of the premutation but only female carriers can pass on the
syndrome to their children. Male carriers wil pass on the premutation to their daughters who
then become carriers. One in around 250 women are Fragile X premutation carriers, often
unknowingly. As women have two X chromosomes, there is a 50% chance that women who are
either premutation carriers or have Fragile X wil pass on the syndrome to their children.
The impacts of Fragile X syndrome are lifelong. Key characteristics of Fragile X syndrome
include developmental delay and anxiety (hyperarousal). There is a genetic link between Fragile
X syndrome and autism spectrum disorder (ASD). Approximately 50% of males and 30% of
females with Fragile X syndrome also have a diagnosis of ASD, and many other males wil have
autistic-type traits.
The impacts of Fragile X syndrome include a wide range of difficulties such as:
• daily living (anxiety, motor delays, difficulty sleeping, eating issues, toileting, etc.)
• learning challenges including short term memory, difficulty with abstract concepts and
planning, expressive language deficits, inattention
• speech and language, including delayed speech or being fixated on something
(perseveration)
• behavioural and emotional impacts such as anxiety, ASD, Attention Deficit Hyperactivity
Disorder and aggression
• other social impacts
• medical impacts including low muscle tone, epilepsy and ear infections.
The effects of Fragile X syndrome wil vary for each individual, ranging from mild to severe.
While males commonly appear more severely affected by Fragile X syndrome, some females
may also be severely affected. Intellectual disability occurs in 80% of males and about 30% of
females with Fragile X Syndrome.
With appropriate care and supports, people who have Fragile X syndrome have a normal life
expectancy. Support needs may change at times of transition and throughout life.
What is Fragile X syndrome? – 5
Page 123 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fragile X syndrome Disability Snapshot
3 How is Fragile X syndrome diagnosed?
Fragile X syndrome is diagnosed by DNA testing, generally from a blood sample. A general
practitioner, paediatrician, geneticist or any medical doctor can request the test. An individual
should be tested for Fragile X if they have developmental delay, unexplained intellectual
disability, or where there is a family
history of Fragile X.
Some girls with Fragile X syndrome may be diagnosed much later than boys if there is no
history of the condition in the family. Females are less likely to display symptoms because they
can conceal the impacts of Fragile X syndrome.
How is Fragile X syndrome diagnosed? – 6
Page 124 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fragile X syndrome Disability Snapshot
4 Language and terminology
The expression ‘living with Fragile X syndrome’ is an acceptable way to describe someone who
has been diagnosed with the condition. ‘Fragile X’ or FXS are acceptable abbreviations to use
for Fragile X syndrome.
Language and terminology – 7
Page 125 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fragile X syndrome Disability Snapshot
5 Enabling social and economic participation
There is no cure for Fragile X syndrome. Early intervention with a multidisciplinary approach
and ongoing supports wil maximise a person’s capacity for daily living and social and economic
participation.
People diagnosed with Fragile X syndrome experience communication, cognitive and
behavioural impairments which present challenges in participating in school, employment and
community settings.
Supports to enable the participant’s social and economic participation may include:
• Occupational therapy such as sensory integration, developing structured routines,
encouraging independence through capacity building, providing support in a workplace.
• Psychological therapies such as support with anxiety/hyperarousal.
• Support coordination to maintain consistency of therapeutic relationships, build capacity
of the family unit and support carers.
• Support in the community including support workers to provide consistent, safe
supports, and model appropriate social skil s in a variety of situations.
• Assistive technology and appropriate equipment in the home, work or volunteer setting.
• Speech and language therapy.
• Education supports such as learning environments that are suitable for the Fragile X
learning style and support executive function. Examples include using visual input
(pictures, timetables); minimising distractions; using calming strategies; positively
reinforcing good behaviour.
Enabling social and economic participation – 8
Page 126 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fragile X syndrome Disability Snapshot
6 Families and carers
Families and carers play an important role in supporting the participant who has Fragile X
throughout their life. They are usually involved in supporting the participant to gain access to the
NDIS, planning and implementation of supports.
As Fragile X Syndrome is an inherited condition, it may impact other family members and the
participant’s home life. The family unit may need support through access to respite or support
with the participant’s daily living activities or community participation. The impact of raising a
child or children with Fragile X syndrome can also affect a family unit. You should consider how
funded supports for the participant can result in a break for families and carers.
As Fragile X syndrome is hereditary, the biological mother can experience feelings of guilt or
other feelings associated with being a carrier of the condition.
Support coordination can be an effective support for the family/carer and individual with Fragile
X syndrome.
Families and carers – 9
Page 127 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fragile X syndrome Disability Snapshot
7 How can I tailor a meeting to suit a participant with
Fragile X syndrome?
Get in touch with the participant before the meeting to find out what support they might need.
When meeting a participant with Fragile X syndrome, make sure to minimise any distractions
and reduce any sensory stimuli in the environment. For example, bright or flickering light or
background noise. Consider offering breaks during the planning discussion. Before the meeting,
consider providing written material in plain English or Easy English, with questions and points to
discuss.
During the discussion, allow time for people to reflect on questions and respond. Use open body
language and a calm tone of voice. You can check understanding with questions such as “can
you explain that back to me?”. Make sure you read back what has been written to ensure the
participant is comfortable their goals have been accurately recorded.
Participants wil often be accompanied and supported by family members for NDIS discussions,
especially to provide support with communication. Where planning discussions involve mothers
who are premutation carriers of Fragile X, be mindful of their feelings and possible level of
anxiety. Additionally, a parent or family member may also have Fragile X syndrome and need
support themselves. This might make it difficult for them to develop or implement the
participant’s plan. Consider suggesting that the participant/family/carer involve an advocate,
support coordinator, or support worker to support them in the meeting.
How can I tailor a meeting to suit a participant with Fragile X syndrome? – 10
Page 128 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fragile X syndrome Disability Snapshot
8 What people with Fragile X syndrome want you to
remember
• Understanding the impacts of Fragile X on daily living are key to developing supports
that allow an individual to live their best life.
• Fragile X syndrome is an inherited lifelong genetic condition, and families may have
more than one child with Fragile X syndrome.
• Fragile X is diagnosed by DNA test, not behavioural testing or analysis of physical facial
features.
• In around 30% of diagnoses there is no family history of Fragile X syndrome.
• Early intervention and ongoing therapies support capacity building.
• Fragile X presents differently in females and males.
• Females who have Fragile X syndrome may mask their cognitive-communicative
disability through shyness or avoidant behaviour.
• Changes in behaviours usually have an additional cause, such as an undiagnosed
medical condition, hormonal changes (for example, puberty, or ageing later in life), a
change in environment (transitions can be difficult), adverse social interactions (for
example, bullying in work or school). Further assessments by a professional wil be
required.
What people with Fragile X syndrome want you to remember – 11
Page 129 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Fragile X syndrome Disability Snapshot
9 Helpful links
• Fragile X Association of Australia
• National Fragile X Foundation (USA)
• Fragile X Al iance
Helpful links – 12
Page 130 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 11
Global Developmental Delay
Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:12:18
Page 131 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
Table of Contents
1
Peak body consulted ........................................................................................................... 4
2
What is Global Developmental Delay? ............................................................................... 5
3
How is GDD diagnosed? ..................................................................................................... 6
4
Language and terminology ................................................................................................. 7
5
Enabling social and economic participation ..................................................................... 8
6
Families and carers ............................................................................................................ 10
7
How can I tailor a meeting to suit a participant and with global developmental delay?
11
8
What families of children with GDD want you to remember .......................................... 12
9
Helpful links ........................................................................................................................ 13
Table of Contents – 2
Page 132 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
This Disability Snapshot provides general information about global developmental delay to
support you in communicating effectively and supporting the participant and their parent/carer in
developing their goals. Each person is an individual and will have their own needs, preferences
and experiences. This information has been prepared for NDIA staff and partners and is not
intended for external distribution.
Peak body consulted – 3
Page 133 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with Association for Children with Disability Tasmania.
We would also like to acknowledge resources from Cerebral Palsy Alliance.
Peak body consulted – 4
Page 134 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
2 What is Global Developmental Delay?
Global developmental delay (GDD) describes a child who is taking longer to reach
developmental milestones in two or more areas of functioning. GDD is diagnosed when a child
experiences these delays in two or more areas of functioning which have continued for at least
6 months.
The developmental delays may impact the following areas:
speech or language development
gross motor skill development (or big movements), such as walking or sitting
fine motor skill development (or little movements), such as drawing or holding a toy
mobility and motor planning
thinking, understanding and learning
relating to other people, making friends and regulating their own emotions
daily living tasks and activities, such as dressing and going to the toilet.
Early intervention programs can give many children with GDD a head start and a better chance
to reach their full potential. Supports may improve functional outcomes relating to the child’s
daily activities, routines and social participation.
Children with GDD may go on to be diagnosed with another disability and need ongoing
support.
What is Global Developmental Delay? – 5
Page 135 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
3 How is GDD diagnosed?
GDD is diagnosed in children under five years of age and in many cases there are no known
causes. GDD is diagnosed by a specialist – usually a paediatrician – after a developmental
screening assessment by a general practitioner or maternal and child health nurse. A
paediatrician will often complete a range of tests to assess for possible causes of the child’s
developmental delays. A child will be diagnosed with GDD when they are not able to undertake
a formal assessment for intellectual disability.
A diagnosis of GDD highlights the need for regular assessments in order to determine the
cause and extent of developmental delays. A child’s diagnosis will usually change to intellectual
disability, autism, or another condition as they get older. A person will not be diagnosed with
GDD for the first time after age 5, – reports could say “initially diagnosed with GDD” as part of
the person’s history.
An assessment – either an adaptive functioning or an adaptive behaviour assessment – of the
child’s daily routines and participation in the community may also help to determine what types
of support will benefit the child. This includes looking at how the child interacts with others at
home, kindergarten, or in a community setting. It is important to assess how the child responds
to intervention – whether the child is responding to the current supports, or if another
intervention is more suitable.
How is GDD diagnosed? – 6
Page 136 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
4 Language and terminology
When talking about a child with GDD you should focus on the person, not the impairment. You
should generally use inclusive person-first language. Use the phrases such as ‘a child living
with GDD’.
As participants with GDD are children, most communication will be with parents or family
members. Make sure to focus on the child’s strengths and abilities rather than what they can’t
do. Understand that this is a difficult time for parents and make sure that your language reflects
this.
Language and terminology – 7
Page 137 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
5 Enabling social and economic participation
A child with GDD may benefit from early childhood intervention supports from the NDIS as well
as mainstream health and early childhood education support. A multidisciplinary team –
including physiotherapists, OTs, speech therapists, therapy assistants and medical personnel –
is crucial for the assessment of and intervention with the whole child.
Mainstream supports may include:
a general practitioner
medical specialists such paediatricians or maternal and child health nurses
early childhood educators and teachers who can help deliver an early learning program
and support the child in pre-school and school.
You may consider recommending NDIS supports in the Core, Capacity Building, and Capital
categories. These supports may vary depending on the child’s age and circumstances. For
example, support for daily living is largely funded through Capacity Building supports however if
there is an evidenced need beyond what would be considered typical parental responsibility,
Core supports for children may be considered.
Core supports:
Core supports may be considered in exceptional circumstances for respite or to support
informal care from parents or carers. For example, where a child requires a level of support with
daily activities significantly beyond the level usually required for children of the same age.
Capacity Building supports:
Capacity Building supports provide the participant with funding to access early childhood
intervention (therapeutic supports). These supports will come from a multi-disciplinary team and
aim to:
develop
self-care skills with tasks like picking things up, dressing or eating
independently
engage in suitable play activities
support physical development, for example, walking and overcoming poor balance,
muscle weakness, and motor planning
develop speech and language skills
auditory processing assessment and other sensory processing assessments
monitor overall development, and assess and manage behavioural or emotional issues
assess the child’s vision and vision monitoring every 6 months to a year is important as
the child develops.
Capital supports:
Enabling social and economic participation – 8
Page 138 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
Capital supports include Assistive Technology to support the child with GDD with self-care and
communication if necessary.
Enabling social and economic participation – 9
Page 139 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
6 Families and carers
A diagnosis of GDD can be unsettling for family members and carers. They may still be coming
to terms with the diagnosis and what changes need to be made as a result. They may be
confused and anxious as GDD requires further assessment which may lead to a new diagnosis.
Families and carers may experience different emotions at different times as the child’s
development progresses.
Families and carers play an important role in supporting a child living with GDD. They are
usually involved in supporting the child to gain access to the NDIS, planning and
implementation of supports for the individual.
Raising a child with GDD can have a significant impact on a family unit, particularly with other
children. The family may need support to access respite, family counselling, and information
and training on GDD. This can help parents and carers to understand the different therapies
that may be included in their child’s plan.
Families and carers – 10
Page 140 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
7 How can I tailor a meeting to suit a participant and
with global developmental delay?
Family members will be the main contact and support for children with GDD and will accompany
them at NDIS meetings.
Allow enough notice for the family member to prepare for meetings (ideally four weeks)
and be clear about what ‘prepared’ means.
Listen non-judgmentally and collaborate with the family member to clarify the child’s
needs, as well as their needs to support the child. Ask the person what they find
important and don’t make assumptions. Use paraphrasing and clarifying questions to
understand their wants and needs.
Be honest and clear about what you can and cannot do.
Discuss that information and recommendations from assessments will inform how the
next NDIS plan is created to support the child.
Provide information about your recommendations and why they are relevant, even if it
seems obvious.
Parents and family members may not know what support is available. Talk to them about the
types of supports that can be included in their plan and how they will be individualised for their
child. Highlight what necessary supports and services family members have access to in order
to support the child and the family unit as a whole.
How can I tailor a meeting to suit a participant and with global developmental delay? – 11
Page 141 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
8 What families of children with GDD want you to
remember
Family members/carers may be stressed or experiencing grief, especially if the
diagnosis is recent. Be sure to acknowledge their experience and be sensitive to how
they might be feeling.
Families may be concerned that they might not get the right supports for their child,
especially long term.
Families may not know what supports are available, or which professionals they should
access. They may be confused about which services will be provided through the NDIS
or other mainstream services such as health or education.
Families may be new to the system and not fully understand how the NDIS works. They
may be trying to navigate this while learning to be new parents, or caring for other
children in the family unit.
What families of children with GDD want you to remember – 12
Page 142 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Global Developmental Delay Disability Snapshot
9 Helpful links
Cerebral Palsy Australia - Global Developmental Delay
Raising Children - Developmental Delay
Mencap UK - Global Developmental Delay
Early Childhood Early Intervention intranet page
Helpful links – 13
Page 143 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 12
Huntington’s Disease Disability
Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:12:32
Page 144 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Huntington’s Disease Disability Snapshot
Table of Contents
1 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 What is Huntington’s Disease? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 How is Huntington’s disease (HD) diagnosed? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 Communicating and supporting people with HD . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
5 Language and terminology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 Enabling social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
7 How can I tailor a meeting to suit a participant with Huntington’s disease? . . . . . . . 10
8 What people with Huntington’s disease want you to keep in mind . . . . . . . . . . . . . . . 11
9 Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12
Table of Contents – 2
Page 145 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Huntington’s Disease Disability Snapshot
This Disability Snapshot provides general information about Huntington’s disease to help you to
communicate effectively and support the participant in a planning meeting. Each person living
with Huntington’s disease is an individual with their own needs, preferences and experiences.
This information has been prepared for NDIA staff and partners and is not intended for external
distribution.
Peak body consulted – 3
Page 146 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Huntington’s Disease Disability Snapshot
1 Peak body consulted
In developing this resource, we consulted the Consortium of Australian Huntington’s
Associations.
Peak body consulted – 4
Page 147 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Huntington’s Disease Disability Snapshot
2 What is Huntington’s Disease?
Huntington’s disease (HD) is a rare, hereditary, chronic, neuro-degenerative neuromuscular
disease with no cure. However, there are treatments and strategies to minimise the impact of
the disease. Signs and symptoms often begin to appear when people are in their 30s and 40s.
• SIGNS are changes as noted by others.
• SYMPTOMS are changes noticed by the HD affected person.
Common early signs and symptoms include:
• loss of fine motor coordination
• muscle stiffness
• involuntary body movements (often pronounced) known as chorea
• cognitive or behavioural changes (for example, memory loss, mood swings, trouble with
concentration, difficulty in making decisions, and behaving impulsively).
Not all people with HD wil have the same changes, even those from the same family.
Huntington’s disease wil progressively affect how the person functions each day, and wil
change their everyday needs. Eventually, HD will significantly impact a person’s ability to make
rational decisions, walk safely, speak clearly and swallow normal food safely.
Most people with HD have a life expectancy of 10 – 20 years after measurable changes begin,
but they have usually had signs and symptoms for much longer.
What is Huntington’s Disease? – 5
Page 148 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Huntington’s Disease Disability Snapshot
3 How is Huntington’s disease (HD) diagnosed?
Huntington’s disease is often diagnosed when a person with a family history experiences mild
changes in their functioning. Their GP wil usually organise a general physical and neurological
exam, and should refer them to a Huntington’s disease specialist clinic if one is accessible.
They wil likely recommend an MRI scan of the brain.
A genetic test wil confirm the diagnosis, usually following genetic counselling for the family in a
genetics clinic.
It is important to understand that while most people with HD are aware of a family history of the
disease, this is not true for everyone. The family history issue needs a sensitive, tactful
approach.
How is Huntington’s disease (HD) diagnosed? – 6
Page 149 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Huntington’s Disease Disability Snapshot
4 Communicating and supporting people with HD
People with HD may struggle with communication because they become less aware of other
people. They may also experience psychological symptoms such as anxiety, depression and
personality changes.
To successfully communicate with people with HD, it’s crucial to understand that they may not
be aware of their own physical and cognitive changes.
The progress of the disease varies between individuals with HD, and over time for the same
person, so a flexible, individualised care plan wil work best. The changes tend to be gradual.
However, if a sudden change in ability is noticed, professional help may be needed to treat any
reversible conditions such as infection, or to understand and manage what may be triggering
behavioural responses.
The participant’s plan may need to be reassessed often, and there may be frequent changes in
how they manage to do things.
Communicating and supporting people with HD – 7
Page 150 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Huntington’s Disease Disability Snapshot
5 Language and terminology
You should use language which reflects the person first, for example “person living with
Huntington’s disease”. Some of the language used when talking about Huntington’s disease is
explained below.
•
Chorea: involuntary, dance-like movements – the person may be unaware they have
chorea even when it’s obvious to others
•
Hereditary: passed on from one family generation to the next
•
Dominant: one mutated copy of a gene is enough to cause disease
•
Neurodegenerative: a condition of the nervous system that wil continue to get worse
over time.
Language and terminology – 8
Page 151 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Huntington’s Disease Disability Snapshot
6 Enabling social and economic participation
You’re best able to support a participant with HD when you know what challenges and barriers
to social and economic participation they’re likely to face.
For example, a participant with HD could experience challenges in their personal relationships
because of the impacts of the disease. They wil gradually lose their physical independence and
often experience psychological and/or behavioural symptoms which can place a strain on their
relationships.
Counselling or other types of psychological support may help them and their carers better cope
with their changing life circumstances. Arranging appropriate social activities, especially outings,
can make a big difference to their quality of life.
Although the cognitive impacts of HD may be subtle, they can affect the participant’s ability to
communicate their needs clearly during a planning meeting. Keep this in mind when talking to
the participant and/or their carer.
It’s important to include support coordination for the participant to implement their plan. For
example, because of the impact of HD the participant may find it difficult to communicate with
their service providers. Having a support coordinator to help them wil make sure they keep
getting the supports they need. If the participant experiences a behavioural crisis , the support
co-ordinator may be able to adjust the supports the participants needs instead of needing a
change to the participants plan.
Enabling social and economic participation – 9
Page 152 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Huntington’s Disease Disability Snapshot
7 How can I tailor a meeting to suit a participant with
Huntington’s disease?
It’s important to remember that Huntington’s disease is a degenerative disease and the
participant’s needs are likely to change over time. Make sure to check with the participant and
their carer for any adjustments they might need for the meeting beforehand. It’s important to
check with both a family member or carer as well as the participant to gain a full understanding
of their symptoms, diagnosis or problems.
While sensitivity is needed when discussing future support needs, it’s important to be realistic
about the participant’s growing and potentially unpredictable need for support as their
Huntington’s disease progresses.
You should consider supports that wil :
• enable the participant to make the most of their independence, and keep them safe for
as long as possible
• help maintain the participant’s social and economic participation
• help maintain their relationships.
You should also ensure;
• there is funding in the plan for specialist training in providing support to participants with
HD as many service providers often have no background or experience with HD.
Funding in the plan may include things like assistive technology or psychological support. It’s
important to listen to the participant as well as their carers to make sure you get all the
information you need to make your decisions.
How can I tailor a meeting to suit a participant with Huntington’s disease? – 10
Page 153 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Huntington’s Disease Disability Snapshot
8 What people with Huntington’s disease want you to
keep in mind
In building a successful relationship with a person with HD, it’s very important to convey a
strong sense of respect, and be direct and simple in your choice of words. Always request
feedback to check they have got the message you wish to convey, without hurrying the person
as they may take much longer than expected to formulate their response.
Huntington’s disease affects everyone differently, even within the same family. Keep this in
mind when supporting multiple participants from the same family.
What people with Huntington’s disease want you to keep in mind – 11
Page 154 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Huntington’s Disease Disability Snapshot
9 Helpful links
• Huntington’s Australia
• NSW Huntington Outreach Service
Helpful links – 12
Page 155 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 13
Intellectual Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:12:44
Page 156 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
Table of Contents
1
Peak body consulted ........................................................................................................... 4
2
What is intellectual disability? ............................................................................................ 5
3
How is intellectual disability diagnosed? .......................................................................... 6
4
How many people have intellectual disability?................................................................. 7
5
What causes intellectual disability? .................................................................................. 8
6
Common characteristics and impacts of intellectual disability ...................................... 9
7
Enabling social and economic participation ................................................................... 11
8
How can I tailor a meeting to suit a participant with intellectual disability? ............... 13
9
Helpful links ........................................................................................................................ 14
Table of Contents – 2
Page 157 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
This Disability Snapshot provides general information about intellectual disability to assist you in
communicating effectively and supporting the participant to develop their goals in a planning
meeting. Each person is an individual and will have their own needs, preferences and
experiences that will impact on the planning process. This information has been prepared for
NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 158 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with Inclusion Australia.
Peak body consulted – 4
Page 159 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
2 What is intellectual disability?
Intellectual disability usually begins before the age of 18 and affects people their whole life.
Intellectual disability does not define who a person is, and each individual person has their own
personality, interests, skills and needs[i].
A person with intellectual disability experiences significant limitations[ii] in
their intellectual
functioning. This includes:
reasoning
planning
problem
solving
understanding complex ideas.
Intellectual disability also affects adaptive behaviours such as:
academic skills - for example, language, reading, writing and arithmetic
social skills - for example, interpersonal skills, communication, self-esteem, gullibility,
and social problem solving
practical
skills
- for example, personal care, use of money, safety, health care, domestic
tasks, and travel.
What is intellectual disability? – 5
Page 160 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
3 How is intellectual disability diagnosed?
Intellectual disability is diagnosed by a psychologist accredited in conducting standardised
assessments of intelligence and adaptive behaviour.
How is intellectual disability diagnosed? – 6
Page 161 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
4 How many people have intellectual disability?
People with intellectual disability are one of the largest primary disability groups in the NDIS.
11% of NDIS participants at 30 December 2019 had an intellectual disability[iii].
Approximately 45% of people with intellectual disability will have another significant
disability, for example, autism, physical, psychosocial or sensory disability[iv].
How many people have intellectual disability? – 7
Page 162 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
5 What causes intellectual disability?
Intellectual disability can occur before, at, or after birth. There are a range of causes of
intellectual disability, including:
Prenatal – for example, chromosomal disorders, gene disorders, syndromes, metabolic
conditions, brain malformation or injury, parental substance abuse, maternal
malnutrition, or violence
Perinatal – for example, labour or birth injury
Postnatal
– for example, malnutrition, child abuse and neglect, chronic illness, and
degenerative disorders[v].
What causes intellectual disability? – 8
Page 163 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
6 Common characteristics and impacts of intellectual
disability
Communication
Challenges with communication are common for many people with intellectual disability. This
can make it difficult for a person to navigate service systems.
Some people with intellectual disability have good conversation skills whereas others have
limited or non-verbal communication skills.
People with intellectual disability have the right to be supported to make or contribute to making
their own decisions (supported decision making). Even when an individual has a legal guardian
or appointed nominee (substitute decision making), it is the responsibility of the guardian or
nominee to support them increase their capacity to make decisions.
For both supporting and appointed decision makers, the rights, dignity, interests, choices and
wellbeing of the person with intellectual disability are paramount.
People with intellectual disability can be vulnerable to suggestion and may agree to what is
asked or said because they think it is expected of them. They may agree with authority figures
because they want to please people.
It is essential to check with the participant during meetings to ensure they understand the
discussion and are able to communicate their wishes, opinions or decisions. A simple check of
understanding can be made by asking an individual; “can you explain that back to me in your
own words?”
Behaviour
Some people with intellectual disability may have “behaviours of concern” or “challenging
behaviour” which may include self-harming behaviour, verbal or physical aggression, or
property damage. This behaviour is often a form of communication due to an inability to convey
messages through typical forms of communication.
People with intellectual disability who experience difficulty with their behaviour need strategies
and support to develop appropriate behaviours. This then allows them to feel comfortable and
included in typical community activities.
Physical health and mental health
The physical health and mental health of people with intellectual disability can impact on their
functional capacity.
Common characteristics and impacts of intellectual disability – 9
Page 164 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
Some individuals with intellectual disability enjoy good health and mental health which allows
them to participate fully in work and community activities. Other individuals with intellectual
disability have significant health limitations that can restrict personal, social and economic
activities, and may require special medical attention.
Complex support needs
Some people with intellectual disability also have complex support needs. This may mean they
require supports for daily activities from a range of mainstream and community service systems
including:
health and mental health
criminal
justice
alcohol
and
drug
housing
education and employment.
Common characteristics and impacts of intellectual disability – 10
Page 165 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
7 Enabling social and economic participation
Full inclusion
Historically people with intellectual disability have been grouped together in separate settings
for living, education, work, and day activities. People with intellectual disability do not need to be
grouped together to meet their individual needs for education, work, living or community
participation.
For people with intellectual disability, full inclusion means being involved and accepted as equal
participating members in the Australian community.
The NDIS provides people with intellectual disability with the reasonable and necessary
supports to pursue their areas of interest and fully participate in roles and activities in the
community.
Some people with intellectual disability require frequent or intensive support to promote
development, maximise independence and well-being.
Expectations
People with intellectual disability are frequently and unfairly at risk of low expectations about
their capacity to learn and do tasks.
For example, if we think a person cannot learn to use public transport, we may choose not to
teach a person how to use public transport. Without travel training, a person will not get the
opportunity to learn how to travel.
This low expectation can be a self-fulfilling prophecy. It can lead to an individual becoming
dependent on others to do daily tasks despite having the capacity to learn and take on these
tasks independently.
Research and lived experience indicates we can assume people with intellectual disability can
learn, work and participate in community activities.
Skill development and support
Research and lived experience have shown people with intellectual disability may find it difficult
to generalise or transfer skills from one setting to another. This makes it essential for skill
development to happen in the place a person with intellectual disability is to perform that skill.
For example, the most effective open employment strategy is to train a person with intellectual
disability in a regular workplace in the open workforce[vi].
Enabling social and economic participation – 11
Page 166 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
A person with intellectual disability may benefit from NDIS supports like taking part in a
vocational ‘discovery’ process. This allows the person to explore their strengths and interests in
the context of work. Volunteering can also be a first step in building confidence and connecting
to the community and the idea of employment.
Once in work, many NDIS participants with intellectual disability may need regular, ongoing
support in the workplace to help them undertake daily work tasks, as well as develop and
maintain skills in the workplace. This level of support to work has traditionally been provided in
an Australian Disability Enterprise (ADE).
Assistive technology may also be required to support participation in work.
Enabling social and economic participation – 12
Page 167 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
8 How can I tailor a meeting to suit a participant with
intellectual disability?
Every effort must be made to enable people with intellectual disability to lead discussions and
actively participate in meetings.
Consider what will support a successful planning meeting. Do not assume what a person may
need.
It may be helpful to:
provide written information in easy to read English before the meeting
provide the questions and points to discuss before the meeting
if the person has a communication aid, ensure it is available for the meeting
ask the participant what support they may need to participate in the meeting
use pictures or objects, such as a clock or calendar when explaining abstract concepts
such as time
always talk directly to the person wherever possible, not to a support person
speak respectfully in an age-appropriate way. Allow the person whatever time they
need to respond
hold meetings in a quiet setting free of distractions and take breaks if required to
maximise attention
consider having a second meeting to ensure everything is discussed
consider having a family member to participate in the meeting as families often play an
active role in the lives of people with intellectual disability. This will require consent from
the person, unless a family member is a legal guardian, appointed nominee or child
representative
consider having an advocate who is not a family member to participate in the meeting.
How can I tailor a meeting to suit a participant with intellectual disability? – 13
Page 168 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Intellectual Disability Snapshot
9 Helpful links
Inclusion Australia
[i] American Association on Intellectual and Development Disability (2010). Intellectual
Disability: Definition, Classification, and Systems of Supports. AAIDD: Washington. American
Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Arlington, VA: American Psychiatric Publishing
[ii] Significant limitations are defined as approximately two standard deviations below the mean
for a standardised assessment of intellectual functioning and adaptive behaviour
[iii] NDIS COAG Disability Reform Council Quarterly Report, 31 December 2019, page 103.
[iv] Australian Institute of Health and Welfare 2018. Disability support services: Services
provided under the National Disability Agreement 2016–17. Canberra: AIHW
[v] American Association on Intellectual and Development Disability (2010). Intellectual
Disability: Definition, Classification, and Systems of Supports. AAIDD: Washington.
[vi] (a) Department of Social Services. National Disability Employment Framework – Issues
Paper 2014. Migliore, 2010. (b) International Encyclopedia of Rehabilitation. Centre for
International Rehabilitation Research Information and Exchange (CIRRIE).
Helpful links – 14
Page 169 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 14
Motor neurone disease Disability
Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:12:55
Page 170 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Motor neurone disease Disability Snapshot
Table of Contents
1 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 What is motor neurone disease? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 Common characteristics and impacts of motor neurone disease . . . . . . . . . . . . . . . . . 6
4 What are the different types of motor neurone disease? . . . . . . . . . . . . . . . . . . . . . . . . 7
5 How is motor neurone disease diagnosed? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 Enabling social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
7 How can I tailor a meeting to suit a participant with motor neurone disease? . . . . . . 10
8 Accessibility or support . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
9 Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12
Table of Contents – 2
Page 171 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Motor neurone disease Disability Snapshot
This Disability Snapshot provides general information about motor neurone disease to assist
you in communicating effectively and supporting the participant in developing their goals in a
planning meeting. Each person is an individual and wil have their own needs, preferences and
experiences that wil impact on the planning process. This information has been prepared for
NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 172 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Motor neurone disease Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with the peak body, Motor Neurone Disease Australia.
Peak body consulted – 4
Page 173 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Motor neurone disease Disability Snapshot
2 What is motor neurone disease?
Motor neurone disease (MND) is the name given to a group of diseases in which the muscles
that enable us to move, speak, breathe and swallow fail to work normally. These muscles and
the nerves that supply them are known, collectively, as the motor system - the system that is
concerned with action and movement (as opposed to sensation).
The system fails because the nerve cells that control movement (the motor neurones)
degenerate and die. This loss of motor neurones causes an increasing loss of function over
time. The patterns of weakness in MND vary from person to person and currently there is no
effective treatment or cure.
There are two different types of motor neurones, and both may be affected:
• Upper motor neurones in the brain - damage to these neurones causes spastic or stiff
paralysis of the muscles that they serve.
• Lower motor neurones in the spinal cord - damage to them causes flaccid or floppy
paralysis.
Without nerve impulses (messages from the brain and spinal cord) the muscles have nothing to
activate them and they gradually waste away.
The average life expectancy for a person with MND is two to three years from diagnosis or three
to five years from the onset of early symptoms. However, about five to ten per cent of people
with MND wil have a slowly progressive form of the disease and may live with the disease for
up to ten years or more.
What is motor neurone disease? – 5
Page 174 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Motor neurone disease Disability Snapshot
3 Common characteristics and impacts of motor
neurone disease
The pattern of symptoms of MND varies from person to person. Usually the condition begins by
affecting only one part of the body then gradually spreads. In some people the symptoms are
widespread from the start. Often only upper or lower motor neurones are affected in the early
stages, but both are usually involved as the condition progresses.
Early symptoms are usually mild. They may include problems with walking or holding objects in
the hand, slurred speech or difficulty swal owing. Some people find that emotional responses
such as laughing or crying are more easily triggered.
Cramps are common as is muscle twitching (fasciculation), which is a sign of damage to lower
motor neurones (those in the spinal cord). Damage to upper motor neurones (those in the brain)
results in stiffness of the muscles (spasticity) and slowed movements. Sometimes the muscles
wil spasm or jerk spontaneously.
Overtime, the loss of mobility and independence means that many people with MND wil need
help with personal care, including washing, dressing and going to the toilet. While most people
maintain their ability to control their bowel and bladder, their reduced capacity to move about
can mean it is harder to get to the toilet. This can be very distressing. Constipation can also
occur because they are moving less and have made diet changes to adapt to their swallowing
difficulties.
In the past, it was thought that MND only affected the neurones controlling the muscles that
enable us to move, speak, breathe and swallow. It is now known that up to 50 percent of people
with MND can experience changes in cognition, language, behaviour and personality. Most
people experience relatively mild changes. However, a small proportion (5 -15 percent) wil
show more significant changes and wil receive a diagnosis of motor neurone disease with
frontotemporal dementia (MND/FTD). Often the symptoms of dementia come before the motor
symptoms, sometimes by a number of years.
MND does not affect memory or the senses (sight, hearing, taste, smell and touch).
Common characteristics and impacts of motor neurone disease – 6
Page 175 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Motor neurone disease Disability Snapshot
4 What are the different types of motor neurone
disease?
There are four main forms of MND:
• Amyotrophic lateral sclerosis (ALS) is the most common form, characterised by muscle
weakness and stiffness, over-active reflexes and rapidly changing emotions. Upper and
lower motor neurones are both affected and the limbs cease to work properly.
• Progressive muscular atrophy (PMA) is characterised by muscle wasting and
weakness, loss of weight and muscle twitching. Only the lower motor neurones are
affected.
• Progressive bulbar palsy (PBP) mixed bulbar palsy and pseudo-bulbar palsy all involve
the muscles of speech and swallowing. The nerves that control these muscles are in
the lower part of the brain (the bulb), hence the term bulbar palsy (palsy means
paralysis).
• Primary lateral sclerosis (PLS) is very rare with upper motor neurone damage causing
stiffness and paralysis of the limbs. PLS may begin in the arms (flail arm type) or the
legs (flail leg type).
What are the different types of motor neurone disease? – 7
Page 176 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Motor neurone disease Disability Snapshot
5 How is motor neurone disease diagnosed?
It can be difficult to diagnose MND as there are several other conditions resembling it. Doctors
may need to keep the person under review for weeks, months or years to formally diagnose.
The person wil probably be referred to a neurologist - a doctor who specialises in conditions
affecting the brain and nervous system.
The doctor may order various tests, including some to eliminate other conditions. These include
nerve conduction studies (NCS) and electromyography (EMG) which look at how nerves are
functioning by stimulating a nerve electrically and recording the muscle activity that results. The
EMG wil involve putting a fine needle into muscles which can be uncomfortable.
Currently there is no cure for MND, although worldwide research is showing encouraging
progress.
How is motor neurone disease diagnosed? – 8
Page 177 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Motor neurone disease Disability Snapshot
6 Enabling social and economic participation
A person’s support needs for social and economic participation wil change as the disease
progresses. Maintaining maximum independence in work, personal relationships and in the
community wil be an important focus.
• To maintain work, ongoing customisation of work tasks to match the level of function
wil be important, along with consideration of personal care in the work place or
assistance with travel. This might require NDIS funding for specialist disability
assessment services as wel as access to external employment retention and support
initiatives such as the Work Assist program provided by Disability Employment
Services.
Common barriers to social and economic participation include:
•
Lived chal enges: mobility, communication, decision making, social connection,
respiration, emotional lability, swallowing and secretion control, workplace and housing
modifications, transport, obtaining appropriate assistive technology (AT).
•
Concerns and sensitivities: the future, maintaining relationships, living arrangements
such as being able to remain in their own home, embarrassment, activities of daily
living, personal care, family and carers, finances, death.
Enabling social and economic participation – 9
Page 178 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Motor neurone disease Disability Snapshot
7 How can I tailor a meeting to suit a participant with
motor neurone disease?
It is common for people in the early stages of MND to present with reasonable functional
capacity and a person therefore may decline formal personal supports. While a person may be
currently able to continue with their current duties at work, it wil be important to discuss and
plan for functional changes. Participants and employers should be encouraged to work together
as early as possible to discuss customisation of work tasks. This conversation would include
planning for the supports that may be introduced to maximise their independence and longevity
at work.
It is important to be aware that support needs wil change over time and sometimes rapidly.
Sensitivity is needed when discussing the wishes of the person with MND and their family.
Planning for formal support needs may have to be encouraged initial y to enable a smoother
transition when there is a need for more intensive supports.
As MND causes progressive deterioration and loss of function it is more appropriate to ask the
person about their priorities and what actions to take to address these in their plan. This is
preferable to using the term, goal setting.
Planning meetings should provide the person with MND and their family with the opportunity to
think about, discuss and set some immediate and longer term priorities.
These may include:
• maintaining employment and independence in the community
• deciding how they would like to be supported
• health and lifestyle decisions
• maintaining relationships
• carer needs
• equipment and assistive technology including rental or purchase, maintenance and
replacement (to maintain independence, social inclusion, safety and communication)
• assistance with planning and managing changing supports.
Supports for a person with MND are often complex and cross many sectors including health,
disability, community and housing. Individuals often have an ongoing need for assistance with
planning and using their informal, mainstream and funded supports. Given the rapidly
degenerative nature of MND and complexity of supports required, it is highly recommended that
support coordination is included in the plan.
How can I tailor a meeting to suit a participant with motor neurone disease? – 10
Page 179 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Motor neurone disease Disability Snapshot
8 Accessibility or support
The participant may prefer the planning meeting takes place in their home due to mobility
issues, assistive technology in use, toileting concerns, transport issues and fatigue. Accessibility
or support requirements for the meeting should be discussed with the participant prior to the
meeting taking place.
Ensure the participant is aware they can have one or more support people present at the
meeting. Ask about communication and AT needs when making arrangements for the meeting.
Remember the needs of people living with MND can be complex and wil vary from person to
person.
Accessibility or support – 11
Page 180 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Motor neurone disease Disability Snapshot
9 Helpful links
• MND Australia
• MNDcare
Helpful links – 12
Page 181 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 15
Multiple sclerosis Disability
Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:13:06
Page 182 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
Table of Contents
1 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 What is multiple sclerosis? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 Important things to note . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 Common symptoms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
5 How is multiple sclerosis diagnosed? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 Types of multiple sclerosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
7 Common experiences and impacts of multiple sclerosis . . . . . . . . . . . . . . . . . . . . . . . 10
8 Enabling social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
9 How can I tailor a meeting to suit a participant with multiple sclerosis? . . . . . . . . . . 12
10
What people with multiple sclerosis want you to remember . . . . . . . . . . . . . . . . . . . 13
11
Answers to common questions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14
12
Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15
Table of Contents – 2
Page 183 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
This Disability Snapshot provides general information about multiple sclerosis to assist you in
communicating effectively and supporting the participant to develop their goals in a planning
meeting. Each person is an individual and wil have their own needs, preferences and
experiences that wil impact on the planning process. This information has been prepared for
NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 184 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with Multiple Sclerosis Australia.
Peak body consulted – 4
Page 185 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
2 What is multiple sclerosis?
Multiple sclerosis (MS) is the most common degenerative neurological condition diagnosed in
young adults. It is an incurable and chronic, long-term condition. MS affects the central nervous
system. It affects the brain, spinal cord and/or optic nerve and interferes with the normal
conduction of nerve impulses around the body. It is characterised by scarring of the fatty
insulating myelin sheath which protects the nerve fibres. This happens when the body’s own
immune system attacks the myelin sheath, causing inflammation.
These attacks happen early in the disease process and cause a gradual loss of function due to
nerve damage. The attacks result in brain atrophy, creating both cognitive issues and functional
impairments.
Depending on where in the body these attacks and the resulting damage occur, a diverse range
of symptoms, both sensory (sensation) and/or motor (movement) may develop.
What is multiple sclerosis? – 5
Page 186 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
3 Important things to note
• The condition course is unpredictable and differs from person to person.
• For some people, it is a disease that fluctuates in severity with periods of unpredictable
relapse and remission. For others, it is a progressive decline over time. For all, it is life
changing.
• Symptoms interact and cannot be assessed in isolation.
• Symptoms interact with other co-occurring conditions causing a compounding effect.
• Symptoms can be unpredictable and may vary on any given day.
• Invisible symptoms can be debilitating and result in a range of functional impairments.
Important things to note – 6
Page 187 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
4 Common symptoms
MS symptoms can be any combination of the five major functional impairments, including:
•
motor control – lack of muscle control or coordination of movements (ataxia),
muscular spasms and tremors, muscle weakness, impaired style or manner of walking
(gait), coordination problems, speech and communication difficulties (such as dysarthria
and dysphonia), abnormal tone, hyper-tonicity, swallowing difficulties (dysphagia),
breathing difficulties, heart problems, imbalance and impaired upper and lower limb
function
•
fatigue – debilitating fatigue often in combination with heat sensitivity. Fatigue may
impact other active symptoms, for example, the ability to walk distances, concentrate or
complete daily tasks and work
•
other neurological symptoms – including dizziness (vertigo), pins and needles, nerve
pain (neuralgia), ongoing pain, discomfort, and visual disturbances including impaired
vision (diplopia) and depth perception, involuntary eye movement (nystagmus) or partial
or complete sight loss
•
bladder and bowel dysfunction – including incontinence, failure to store or empty,
urgency, waking up more than usual to urinate at night (nocturia), faecal impaction and
constipation, diarrhoea and sexual problems
•
neuropsychological symptoms – including ‘brain fog’, impaired memory and
concentration, changes in processing speed and ability, impaired executive function (for
example reasoning and problem solving), personality changes, emotional changes,
anxiety, depression, suicidal thoughts, cognitive impairment, and dif iculties sleeping.
Common symptoms – 7
Page 188 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
5 How is multiple sclerosis diagnosed?
To help identify MS symptoms earlier, more awareness of MS is needed. Some people may
delay seeking treatment for their symptoms and some GPs and health professionals can miss
early symptoms.
Patients usual y experience a first neurological episode caused by inflammation of the nerve
tissue. This can be significant, especially if it is inflammation of the optic nerve in the eye (optic
neuritis) and there is impaired vision.
Generally, a patient might present to a GP, hospital or specialist with unexplained symptoms.
For example, visual disturbances or loss of physical function in their hands, arms or legs.
MS is usually diagnosed by a specialist MS neurologist following at least one episode of
neurological symptoms and MRI scan results showing new and old lesions in the brain and
spinal cord.
For an accurate diagnosis and effective management, best practice suggests a diagnosis and
ongoing support should be provided by a team of health professionals specialising in MS.
How is multiple sclerosis diagnosed? – 8
Page 189 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
6 Types of multiple sclerosis
•
Relapsing-Remitting MS (RRMS): characterised by unpredictable attacks followed by
partial or total recovery (also called exacerbations, relapses, or flares). This is the most
common form of MS. 70 to 75% of people with MS begin with a relapsing-remitting
course. Treatments aim to reduce attacks to improve long-term outcomes.
•
Secondary-Progressive MS (SPMS): a relapsing-remitting course which later
becomes steadily progressive. Some attacks and partial recoveries may continue to
occur. Of the 70-75% who start with relapsing-remitting disease, more than 50% wil
develop SPMS within 10 years; 90% within 25 years.
•
Primary-Progressive MS (PPMS): a progressive course from onset. Symptoms
generally do not remit. 15% of people with MS are diagnosed with PPMS, although the
diagnosis usually needs to be made later on, when the person has been living for a
period of time with progressive disability and no acute attacks.
Types of multiple sclerosis – 9
Page 190 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
7 Common experiences and impacts of multiple
sclerosis
People living with MS are more likely to be under-employed or unemployed and experience
financial hardship as a result. Some patients might try to hide their symptoms, have persistent
denial of diagnosis or don’t disclose their diagnosis, perhaps for fear of losing their job.
There are also a number of indirect and direct costs (out of pocket expenses) associated with
MS.
Due to the condition’s complexity, people living with MS may struggle to navigate the health and
disability sectors.
Some invisible symptoms such as cognitive and visual disturbances, muscle weakness, spasms
or decreased motor control can impact day to day activities and the ability to:
• engage in long conversations or follow long sentences
• concentrate for lengthy periods
• understand abstract concepts
• complete forms
• use a computer.
Slurred, slow or impaired speech can be misinterpreted as the person being intoxicated or of
lower intelligence. Psychosocial impacts may include reduced self-esteem, social isolation
and/or interpersonal and relationship dif iculties.
Furthermore, carers of people with MS can experience significant carer burden and this has the
potential to lead to relationship difficulties and breakdown.
Common experiences and impacts of multiple sclerosis – 10
Page 191 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
8 Enabling social and economic participation
It is important to explore how a person with MS can be supported to continue their participation
in current activities, education and employment, taking into consideration their interests, level of
function and fatigue.
It may be appropriate for some participants with MS to explore ways to maintain their current
career/profession with supports in place. Peer support from other people with MS can also help
support social and economic participation.
Employment supports that might be considered through the NDIS include, personal care in the
workplace, assistance with travel, assistive technology and funding for specialist disability or
employment related assessment services. Employment retention and support initiatives can be
accessed through Work Assist, the Disability Employment Services (DES) program.
Enabling social and economic participation – 11
Page 192 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
9 How can I tailor a meeting to suit a participant with
multiple sclerosis?
These are some accessibility or support requirements to consider:
• face to face meetings are recommended. Phone conversations are often hard to
manage
• check individual preference for best time of day due to possible brain fog or fatigue.
• check
accessibility requirements. Advise participant of location and availability of
accessible parking
• check if there is a need to break up a face-to-face meeting into two parts or provide a
break
• schedule a reminder for appointments
• encourage a person with MS to bring a support person along to provide reminders,
assist with reading and provide general support
• check comfort levels and ensure adjustable air conditioning is available during a
meeting
• ensure the person knows the location of the nearest restrooms/toilets. Al ow for breaks
• consider that coordination of supports is often required. MS Australia members have
found that plans are often not activated or progressed and can become too complex to
manage when coordination of supports is not included in a person’s plan
• treat someone with the progressive form of MS with urgency, as achieving optimal
functioning in the progressive stage is important to maintain quality of life
• ensure the person knows to notify the NDIA of any changes in circumstances and how
to do so. Consider building flexibility into their plan.
How can I tailor a meeting to suit a participant with multiple sclerosis? – 12
Page 193 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
10 What people with multiple sclerosis want you to
remember
• MS can be challenging, complex and frustrating. Listen with sensitivity.
• Be flexible and prepared to ‘think outside the box’.
• Quite often a person living with MS ‘presents well’ and it is only after more in-depth
questioning that their needs become apparent.
• While some symptoms are relatively easy to discuss, others can cause discomfort or
embarrassment. For example, cognitive symptoms, bladder and bowel dysfunction,
sexual dysfunction and even depression.
• People living with MS may have symptoms that fluctuate greatly from one day to
another. It’s important to ask about hidden (invisible) symptoms and how the person
functions on a ‘bad’ day.
• Good questions to ask are “what makes your symptoms worse?” and “what makes
them better?”
• Ask about other co-occurring conditions/disabilities and how these and various
medications compound the person’s ability to perform daily tasks.
• Fluctuations in mood and mental health are common and greatly impact on functioning
and quality of life. Someone living with mood changes and mental il ness may find goal
setting and evaluation difficult.
• For many people living with MS, impaired cognition can be a major issue and they may
not be fully aware of the full effects of their condition. A person with MS may have
prepared a checklist ahead of the planning meeting to help prompt their memory. It is
important that you adhere to any agreed follow up, for example, by phone or email.
Lack of timely communication is very stressful for people with MS and their carers.
• Consider each person’s support and social network, stability, vocational and family
history, and circumstances. Be mindful of carer burden, relationship breakdown, social
isolation, children with special needs, child protection and family violence issues.
What people with multiple sclerosis want you to remember – 13
Page 194 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
11 Answers to common questions
• Does everyone’s MS follow the same path?
No. Because of the epidemiology of MS, each person’s disease course and the resulting
functional impairments are unique to them.
• Is there a particular age group susceptible to MS?
No, MS can be diagnosed at any age – even in children. The majority of people diagnosed
are in their early 30’s.
• Is there a cure for MS?
No, there is no cure for MS. There are treatments, but only for relapsing-remitting MS.
Treatments aim to reduce inflammation and relapses in order to slow disease progression
and resulting disability. Each person responds differently to treatment.
Answers to common questions – 14
Page 195 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Multiple sclerosis Disability Snapshot
12 Helpful links
• Multiple Sclerosis Australia
Helpful links – 15
Page 196 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 16
Snapshot for Muscular Dystrophy
SGP KP Publishing
Exported on 2024-10-18 03:14:28
Page 197 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Snapshot for Muscular Dystrophy
Table of Contents
1 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 What is muscular dystrophy? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 Common characteristics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 How is muscular dystrophy diagnosed? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
5 Language and terminology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 Enabling social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
7 Families and carers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
8 How can I tailor a meeting to suit a participant with muscular dystrophy? . . . . . . . . 11
9 What people with muscular dystrophy want you to remember . . . . . . . . . . . . . . . . . . 12
10
Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13
Table of Contents – 2
Page 198 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Snapshot for Muscular Dystrophy
This Disability Snapshot provides general information about muscular dystrophy and
neuromuscular disorders to assist you in communicating effectively and supporting the
participant. Each person living with muscular dystrophy is an individual and wil have their own
needs, preferences and experiences. This information has been prepared for NDIA staff and
partners and is not intended for external distribution.
Peak body consulted – 3
Page 199 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Snapshot for Muscular Dystrophy
1 Peak body consulted
In developing this resource, we consulted with Muscular Dystrophy Australia.
Peak body consulted – 4
Page 200 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Snapshot for Muscular Dystrophy
2 What is muscular dystrophy?
Muscular dystrophy is a type of neuromuscular disorder classified by the breakdown of muscle
fibres leading to progressive and irreversible degeneration of muscles. Symptoms of types of
the disorder appear at birth or in young babies, but in other cases the symptoms may only start
to show in childhood or even in adulthood. Some types of muscular dystrophy can lead to
significant impairment and impact on life expectancy, while other types can be much milder.
Around one in every 625 individuals wil be affected with a muscular dystrophy during their
lifetime. There are over 60 separate and distinct types of neuromuscular disorders, each with
their own unique symptoms, treatments and prognosis. There is no cure for any type of
muscular dystrophy.
Neuromuscular disorders are classified into four groups:
• muscular dystrophies
• spinal muscular atrophies
• motor neurone disease
• peripheral (affecting feet and hands) neuropathies.
This snapshot focuses mainly on muscular dystrophy.
What is muscular dystrophy? – 5
Page 201 of 308
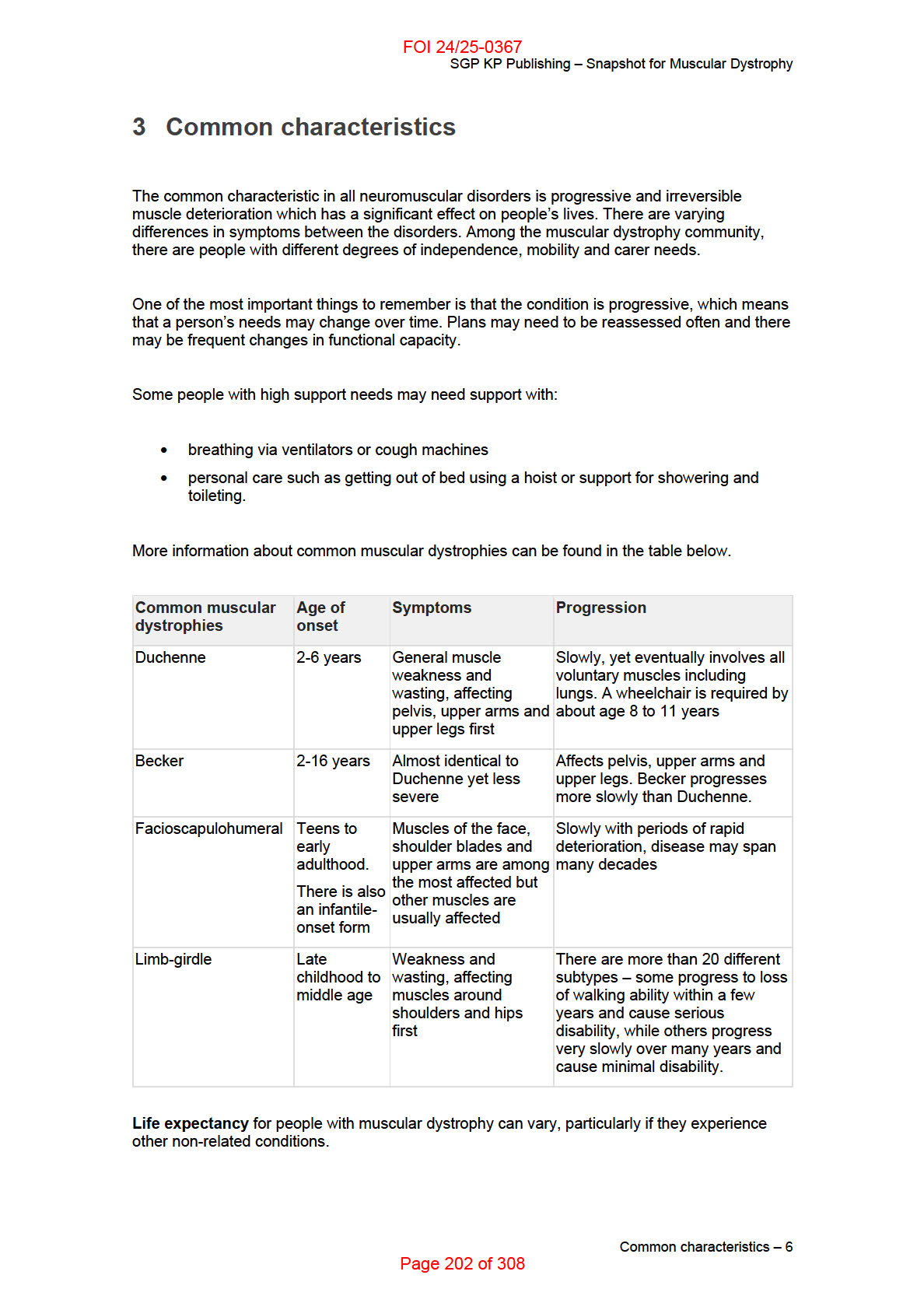
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Snapshot for Muscular Dystrophy
4 How is muscular dystrophy diagnosed?
Diagnosis usually starts with a visit to a general practitioner (GP). A parent might notice their
child falling over more than his or her friends, or an adult finds they can no longer walk very far
without tiring. The GP may carry out initial tests but these conditions are often difficult to
diagnose and the individual wil usually be referred to a specialist – typically a neurologist. The
specialist wil use different tools and tests to reach a clinical diagnosis that best explains the
symptoms and test results.
Tests may include:
• muscle biopsy
• genetic testing
• electromyography
• blood tests.
How is muscular dystrophy diagnosed? – 7
Page 203 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Snapshot for Muscular Dystrophy
5 Language and terminology
You should use language which reflects the person first such as ‘person with a neuromuscular
disorder’, or ‘person living with muscular dystrophy’.
Some of the language used to talk about the common characteristics of neuromuscular
disorders is further explained below:
•
Neuropathies: damage, disease, or dysfunction of one or more nerves especially of
the peripheral nervous system. This is typically marked by burning or shooting pain,
numbness, tingling, or muscle weakness or atrophy (often degenerative).
•
Muscle wasting: weakening, shrinking, and loss of muscle.
•
Myotonic disorders or ‘Myotonia’: the inability to relax muscles fol owing contraction.
Myotonic dystrophy can also affect many other tissues and organs in the body.
Language and terminology – 8
Page 204 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Snapshot for Muscular Dystrophy
6 Enabling social and economic participation
When assessing Assistive Technology (AT) or Capacity Building (CB) support needs, the same
priority needs to be given to work and outside work activities. Not everyone living with muscular
dystrophy is able to work, and everyone has a right to the best quality of life. When you are
considering AT needs for work purposes, you should always explore mainstream services such
as the Employee Assistance Fund (EAF).
Depending on the type of muscular dystrophy and its stage, patients might benefit from different
types of AT, including:
• adapted devices for using a computer, phone, or appliances, including head pointers, a
switch adapted mouse, sip-and-puff switches, and mouth sticks.
• software for alternate access such as voice recognition and auto-type software
• eye gaze systems such as an eye-tracking device of specialised computer input device
• environmental control software such as smart switches and bulbs, and automated
thermostats.
CB supports for people living with muscular dystrophies, depending on the type and stage,
could include:
• disability related respiratory supports
• speech therapy
• occupational therapy
• support coordination.
Enabling social and economic participation – 9
Page 205 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Snapshot for Muscular Dystrophy
7 Families and carers
Families provide different levels of support to a person with muscular dystrophy, and usually
play an active role in a range of supports including:
• assisting with daily living tasks
• advocating for inclusion
• supporting the participant to find employment.
Families usually have a good understanding of the support the person needs to participate in
the community and work towards independence. Some family members may find it confronting
to consider the impact of further deterioration of their loved one’s condition over time and may
need support to think about future support needs.
While families are usually happy to provide support, it can affect their own employment, ability
to meet the needs of other family members, and their own needs and health. This wil increase
especially as they age. It is unreasonable to expect a family to be the main source of support for
an adult living with muscular dystrophy. It is important to consider, for children and adults,
whether the level of informal support being provided is sustainable and what supports might be
included in the plan that result in a break for carers.
Funded support including respite, support to access the community and personal care in the
home can offer relief from family and carer stress.
Families and carers – 10
Page 206 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Snapshot for Muscular Dystrophy
8 How can I tailor a meeting to suit a participant with
muscular dystrophy?
It’s important to think about how people living with muscular dystrophy can be supported to be
included in education, employment, and community and mainstream activities alongside their
peers.
Some people, particularly those with later onset conditions, may have been living with
symptoms for years while struggling to receive a diagnosis. The relative rarity of some forms of
muscular dystrophy means it can be hard to find a specialist who can confidently diagnose the
condition and predict its likely progression. For these individuals, thinking about what supports
they might require in the future may be more difficult.
Specific issues to be considered:
• helping the individual consider not just their current capacity in the ‘here and now’, but
also likely progression of their condition over the length of the plan
• consideration of transport modifications and technology to maintain schooling,
employment, interests, and activities of everyday life
• whether physiotherapy is appropriate, either at home under the guidance of a physio or
at an external venue
• adaptions needed to the home environment to access wheelchairs, hoists, or walking
supports
• consideration of suitability of formal and informal carer supports
• consideration that the person’s condition wil change over time, meaning that plans may
need to be reassessed regularly and the participant may need an unscheduled review.
How can I tailor a meeting to suit a participant with muscular dystrophy? – 11
Page 207 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Snapshot for Muscular Dystrophy
9 What people with muscular dystrophy want you to
remember
• Each case is different and wil have different requirements.
• Make yourself familiar with each condition by referring to this snapshot and other
resources, but also consider each individual’s needs.
• Muscular dystrophies are
progressive disorders, which means the participant’s
functional impairment wil require regular reassessment.
What people with muscular dystrophy want you to remember – 12
Page 208 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Snapshot for Muscular Dystrophy
10 Helpful links
• Muscular Dystrophy Australia (MDA)
• MDA Peripheral Disorders
• MDA Spinal Muscular Atrophy
• MDA Duchenne Muscular Dystrophy
• MDA Becker Muscular Dystrophy
Helpful links – 13
Page 209 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 17
Physical Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:13:20
Page 210 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Physical Disability Snapshot
Table of Contents
1 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 What is Physical Disability?. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 How is Physical Disability diagnosed? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 Language and terminology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
5 Enabling social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 Families and carers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
7 How can I tailor a meeting to suit a participant with Physical Disability? . . . . . . . . . . 10
8 What people with Physical Disability want you to remember . . . . . . . . . . . . . . . . . . . . 11
9 Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12
Table of Contents – 2
Page 211 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Physical Disability Snapshot
This Disability Snapshot provides general information about physical disability to assist you in
communicating effectively and supporting the participant in developing their goals. Each person
is an individual and wil have their own needs, preferences and experiences. This information
has been prepared for NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 212 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Physical Disability Snapshot
1 Peak body consulted
In developing this resource, we consulted with Physical Disability Australia.
Peak body consulted – 4
Page 213 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Physical Disability Snapshot
2 What is Physical Disability?
A physical disability refers to an impairment that affects a person’s range of body movements
when compared to someone without physical disability. It is important to note many different
diagnoses fall under this broad category, and there may be other conditions that can limit a
person’s physical capacity.
Generally, physical disability does not affect a person’s mind or ability to sense their
environment. It is important to not make assumptions about a person’s cognitive capacity or
how their condition may progress as they get older.
This broad category includes the following disabilities in the NDIS Business System:
• cerebral palsy
• spinal cord injury
• multiple sclerosis
• stroke
• other neurological
• other physical.
People with physical disability experience fewer opportunities for social, economic and cultural
participation. They experience more difficulty moving around and interacting with their physical
environment compared to people without physical disability. Many people with physical disability
use mobility aids (such as wheelchairs, scooters, walking frames, etc.), prosthetic limbs, home
and vehicle modifications, and other assistive technology devices.
This information provides a general overview and you should always talk to the participant
about their individual experience. Refer to Helpful links for further information on some of the
specific physical disabilities identified above.
What is Physical Disability? – 5
Page 214 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Physical Disability Snapshot
3 How is Physical Disability diagnosed?
Physical disability can be diagnosed in many different ways depending on the individual and
their circumstances. This may be through physical assessment or further testing. Some physical
disabilities are congenital, meaning a person is born with the disability. A congenital physical
disability may be obvious when a child is born, or it may develop as the person grows older and
be diagnosed later in life.
Other physical disabilities can be caused by injuries or diseases that lead to a significant
physical impairment. This results in either a loss of function to part of the body, or a change in
the person’s capacity to use their body.
How is Physical Disability diagnosed? – 6
Page 215 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Physical Disability Snapshot
4 Language and terminology
Person-first language should be used. You should take care not to identify a person with
physical disability by their impairment. The person with disability has the right to determine what
terminology they prefer and how they identify.
Regardless of their speech or verbal capacity, it is important to approach any discussion with a
person with physical disability as you would with a person without a physical impairment.
Language and terminology – 7
Page 216 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Physical Disability Snapshot
5 Enabling social and economic participation
Some people with a physical disability wil use mobility aids to enable access to community
participation, study, employment and volunteering opportunities. People with different
impairments may also benefit from a wide range of assistive technology that supports access
the community and to assist daily living activities. These may include communication aides,
portable ramps, and devices to assist with turning taps and holding utensils.
Learning from the participant’s lived experience is the best way to understand the type and level
of supports a person with physical disability needs. Each individual wil have preferred
strategies to overcome the barriers that limit their social and economic participation.
Capacity building supports may assist a person with physical disability to participate in social
and economic life in their community. For example, physical and occupational therapies can
support people with physical disability to maintain or improve mobility, making it easier to
engage in an ordinary life.
While capacity building supports are an important part of supporting people with employment
goals, the NDIS is also responsible for funding frequent and ongoing supports that assist a
person with disability to take part in work. This support includes day-to-day, on the job
assistance designed to assist the participant to meaningfully participate in work. Economic
participation has a number of benefits for participants including income, confidence, social
interaction and networks, and a sense of independence.
Enabling social and economic participation – 8
Page 217 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Physical Disability Snapshot
6 Families and carers
People with physical disability live in many different settings and can be receiving support from
family members, as well as other informal and formal supports. Sometimes a participant may
have limited living options, may not have chosen their current living situation and they may not
be happy with these arrangements. It is important not to make assumptions about the informal
support they may (or may not) be receiving.
For example, some people with physical disability may have ‘living independently’ as one of
their goals. They may want to live outside of the family home and gain more self-independence..
Alternatively, they may want to move out of accommodation run by a service provider and have
more choice and control over who they live with, the supports they receive and where they
receive them.
Think about whether additional support in the home, support to access the community or short
term accommodation, including respite, could offer the participant some independence from
family members.
Families and carers – 9
Page 218 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Physical Disability Snapshot
7 How can I tailor a meeting to suit a participant with
Physical Disability?
When organising a meeting with a participant, ask them directly, using their preferred
communication method, what they need in terms of access and support to attend meetings. It
may be useful to ask open ended questions to understand the participant’s needs, such as:
• ‘How would you like to meet with us?’
Travel can be difficult for some people with physical disability so telephone or video-
conference calls may be their preferred option.
• ‘Do you have any physical access requirements for our meeting?’
Some people with physical disability have specific access requirements such as mobility aids
and you wil need to make sure your location is accessible, spacious, level and free of trip
hazards.
• ‘Wil you be bringing anyone with you?’
This may include family members, support workers, communication facilitators and/or
advocates.
• ‘How do you want to receive information from us?’
Paper can be hard for some people with physical disability to manage so it’s a good idea to
discuss alternative formats that are available.
How can I tailor a meeting to suit a participant with Physical Disability? – 10
Page 219 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Physical Disability Snapshot
8 What people with Physical Disability want you to
remember
People with physical disability need you to understand they:
• do not (generally) have a cognitive impairment and they can understand the discussion
• can express their goals and identify barriers to achieving them
• have a good understanding of their disability and level of functional impairment, and
what it means in terms of their capacity to lead an ordinary life
• can express what supports they need and why they consider them reasonable and
necessary.
What people with Physical Disability want you to remember – 11
Page 220 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Physical Disability Snapshot
9 Helpful links
• Physical Disability Australia
• Western Sydney University - Key facts on physical disability
• BetterHealth - Physical disabilities
• Disability Snapshot – Cerebral Palsy
• Disability Snapshot – Multiple Sclerosis
Helpful links – 12
Page 221 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 18
Polio-Related Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:13:32
Page 222 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Polio-Related Disability Snapshot
Table of Contents
1
Peak body consulted ........................................................................................................... 4
2
What is polio-related disability? ......................................................................................... 5
3
How are Polio, LEoP and PPS diagnosed? ....................................................................... 6
4
Language and terminology ................................................................................................. 7
5
Enabling social and economic participation ..................................................................... 8
6
Families and carers .............................................................................................................. 9
7
How can I tailor a meeting to suit a participant with PPS and LEoP? .......................... 10
8
What people with polio-related disability want you to remember ................................. 11
9
Helpful links ........................................................................................................................ 12
Table of Contents – 2
Page 223 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Polio-Related Disability Snapshot
This Disability Snapshot is about polio-related disability and will assist you in supporting the
participant and communicating effectively. This information is a general guide only – each
person is an individual and will have their own needs, preferences and experiences. This
information has been prepared for NDIA staff and partners and is not intended for external
distribution.
Peak body consulted – 3
Page 224 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Polio-Related Disability Snapshot
1 Peak body consulted
In developing this resource, we consulted with Polio Australia.
Peak body consulted – 4
Page 225 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Polio-Related Disability Snapshot
2 What is polio-related disability?
Poliomyelitis (polio) is a highly infectious disease caused by a virus. It affects the nervous
system and can cause complete paralysis. Polio-related disability affects those who have
survived polio, knowingly or unknowingly. Many polio survivors have lived with neuromuscular
disability since their polio infection, which usually occurs in early childhood. Other polio
survivors develop disability later in life, which is known as Late Effects of Polio (LEoP). Some
polio survivors will go on to have a specific diagnosis of Post-Polio Syndrome (PPS) from a
specialist doctor.
LEoP is the general term describing the varied and progressive condition experienced by those
with a history of polio. The symptoms of the condition develop between one to five decades
after infection, and usually include:
new or increasing muscle weakness affecting quality of life or safety
fatigue of muscles of the limbs or trunk, and/or central (exhaustive) fatigue
pain in muscles and/or joints of the limbs or trunk
difficulty
sleeping
other symptoms, including breathing problems, speech and swallowing issues, and
poor thermoregulation.
The majority of polio survivors that access the NDIS are likely to come from migrant or refugee
populations where polio is not eradicated in their home country. Many polio survivors in
Australia are already over the age of 65 and may not be eligible for the NDIS.
Polio survivors mostly display physical disabilities which vary widely from person to person.
Many polio survivors need long-term limb bracing and use assistive technology to increase their
function.
What is polio-related disability? – 5
Page 226 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Polio-Related Disability Snapshot
3 How are Polio, LEoP and PPS diagnosed?
Polio is a virus that can only be diagnosed at the time of infection. Some people don’t know they
have had polio, and it can be diagnosed later in life based on the person’s history and the
likelihood of a previous infection.
LEoP is an informal diagnosis that accounts for a person’s current symptoms and abilities in
context of their polio history. Examples include:
back pain from scoliosis or limping
difficulty maintaining a strong voice during conversations
being exhausted from performing household tasks like doing laundry.
A General Practitioner can diagnose these symptoms and develop a plan to support the polio
survivor. Often, LEoP is only recognised after many other possible illnesses and conditions
have been ruled out. Getting a diagnosis can be an exhausting and traumatic process.
PPS is a specific diagnosis based on five criteria, made by a specialist doctor:
1. prior paralytic poliomyelitis with evidence of motor neuron loss
2. a period of partial or complete functional recovery after acute paralytic poliomyelitis
3. slowly progressive and persistent new muscle weakness or decreased endurance, with
or without generalised fatigue, muscle atrophy, or muscle and joint pain
4. symptoms that persist for at least a year, and
5. exclusion of other neuromuscular, medical, and skeletal abnormalities as causes of
symptoms.
Not all polio survivors who develop LEoP go on to be diagnosed with PPS, but those who are
diagnosed with PPS have most certainly been experiencing LEoP.
How are Polio, LEoP and PPS diagnosed? – 6
Page 227 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Polio-Related Disability Snapshot
4 Language and terminology
People who survived polio are commonly called polio survivors or survivors. Some survivors
refer to themselves as “polios”, however this term is used by the polio community and its use by
others is not encouraged.
When talking about function and activity, you should prioritise managing LEoP, rather than
attempting to find solutions. Ask questions like “how could you make things easier to manage?”
or “if you changed a few things, do you think you might be able to …?”.
Using this type of language, the polio survivor can focus on what they can achieve and avoid
unrealistic goals that may not be achieved with their condition.
Language and terminology – 7
Page 228 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Polio-Related Disability Snapshot
5 Enabling social and economic participation
Support to enable social and economic participation for polio survivors varies. This can depend
on the person’s degree of physical difficulty and any compounding cultural or language barriers.
Required supports may include:
access to culturally-relevant services and supports
collaboration with local cultural services regarding accessibility issues
referral to allied health professionals (especially those trained in post-polio
management)
assistance and/or capacity building in using public transport, or transport funding in
certain situations where public transport is not suitable because of fatigue or low
mobility
vehicle modifications to increase access, both as a driver and a passenger
workplace assessment and appropriate modifications.
Being able to participate in social and community engagement are also important for polio
survivors to increase daily functioning and to promote good mental health.
You should respect the polio survivor’s own ideas about how to achieve their goals, but keep in
mind that many polio survivors might not know how the best way to work within their level of
function and limit fatigue and muscle weakness. Many polio survivors may be overdoing activity,
leading to a further loss in function over time.
For polio survivors from a migrant background, it can be difficult to access employment because
of marginalisation due to physical disability, language barriers, and cultural differences. They
may try to hide their disability out of fear of jeopardising their residency in Australia. They may
also work in manual labour jobs, which are more likely to make their LEoP conditions worse.
Enabling social and economic participation – 8
Page 229 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Polio-Related Disability Snapshot
6 Families and carers
Informal support from family members can range from full time carers to assistance with specific
tasks. With the polio survivor’s permission, it may be appropriate to give the carer or family
member information about the Late Effects of Polio, support services available and direct
contacts who are able to offer guidance. This may be useful to understand the reasons for the
polio survivor’s functional limitations.
Links to resources, contacts and further information can be found in the Helpful Links section.
Families and carers – 9
Page 230 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Polio-Related Disability Snapshot
7 How can I tailor a meeting to suit a participant with
PPS and LEoP?
When organising a meeting you should consider fatigue and mobility issues. You should contact
the participant when booking the meeting to make sure the time suits their routine and any
fatigue they make experience at different times of the day. Some polio survivors may appreciate
the option of a phone or online meeting.
For face-to-face meetings, make sure:
the meeting room is close to the building’s entrance
accessible parking is available, and
the room is at a moderate temperature as polio survivors can experience cold
intolerance.
Before the meeting, take some time to develop an understanding about LEoP and PPS. Don’t
make assumptions, take time and actively listen to understand the history of the person – both
physical and psychological.
It is common for polio survivors to give an impression of more independence than they actually
experience. Use open-ended questions to encourage more detailed answers. For example, ask:
“How do you manage your shopping?”, rather than “Are you able to shop without help?”.
How can I tailor a meeting to suit a participant with PPS and LEoP? – 10
Page 231 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Polio-Related Disability Snapshot
8 What people with polio-related disability want you to
remember
A polio survivor’s disability is physical – there is usually no intellectual or cognitive
component (except where fatigue impacts on memory and concentration).
Their condition often progresses due to neurological breakdown.
Health professionals can often give generic advice on exercise and activity, and
recommendations must be customised to the individual.
Survivors have often overcome stigma and trauma, and may conceal their disability.
Polio survivors are resilient and determined due to overcoming stigma and limitations.
Keeping their independence is often an important goal.
Their mental health can deteriorate if LEoP/PPS symptoms return, unpleasant
childhood memories from infection surface, their independence reduces, or they feel
socially isolated.
Polio and LEoP/PPS affects each person differently – talk to the person directly about
their own experience, functional capacity and goals.
What people with polio-related disability want you to remember – 11
Page 232 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Polio-Related Disability Snapshot
9 Helpful links
Polio Australia
Fact sheets and guides for polio survivors
Fact sheets and guides for professionals
Find a local professional who is familiar with LEoP/PPS
State and territory based Polio organisations
Helpful links – 12
Page 233 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 19
Prader-Willi syndrome Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:13:47
Page 234 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Prader-Wil i syndrome Snapshot
Table of Contents
1 What is Prader-Wil i syndrome? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 Common characteristics and impacts of Prader-Wil i syndrome . . . . . . . . . . . . . . . . . . 5
3 Myths and misunderstandings . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
4 Common barriers to social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . 10
5 What is the role of the family in providing support? . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
6 How can I tailor a meeting to suit a person with PWS? . . . . . . . . . . . . . . . . . . . . . . . . . 12
7 Helpful links for further information . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14
8 Representative bodies consulted when developing this Snapshot . . . . . . . . . . . . . . . 15
Table of Contents – 2
Page 235 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Prader-Wil i syndrome Snapshot
This is a snapshot and is not designed to be a comprehensive guide. It provides general
information about Prader-Wil i syndrome (PWS) for NDIA staff and Partners. It is not to be
distributed externally.
Each person with PWS is an individual but there is a commonality of impairment. Beyond that,
each has their own additional needs, preferences and experiences that wil impact on the
planning process.
In developing this resource, we consulted with Prader-Willi Syndrome Australia.
What is Prader-Wil i syndrome? – 3
Page 236 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Prader-Wil i syndrome Snapshot
1 What is Prader-Willi syndrome?
Prader-Wil i syndrome (PWS) is a rare neuro-behavioural genetic disorder. It is a very complex,
multistage disorder that permanently affects multiple systems in the body. PWS presents at
birth and continues, with significant intensity, throughout life. It occurs equally in males and
females.
People with PWS have a flaw in the part of the brain called the hypothalamus. This part of the
brain is an important supervisory centre and hormone regulator. The hypothalamus when fully
functioning, registers feelings of hunger and satiety (fullness). For individuals with PWS this
does not occur and individuals with PWS never feel full. There is a constant pre-occupation with
food accompanied by an overwhelming physiological drive to eat.
Currently there is no cure for PWS, although advances are being made through treatment with
Growth Hormone. Most people with PWS require specialist support and a supervised diet for
life. Generally, PWS is not inherited (except in 5% of cases) and can occur in any family. A
suspected diagnosis of PWS is usually made by a physician based on clinical symptoms and a
genetic test confirms a diagnosis of PWS. It is estimated that the incidence of PWS varies from
1:15,000 to 1:25,000 births.
What is Prader-Wil i syndrome? – 4
Page 237 of 308
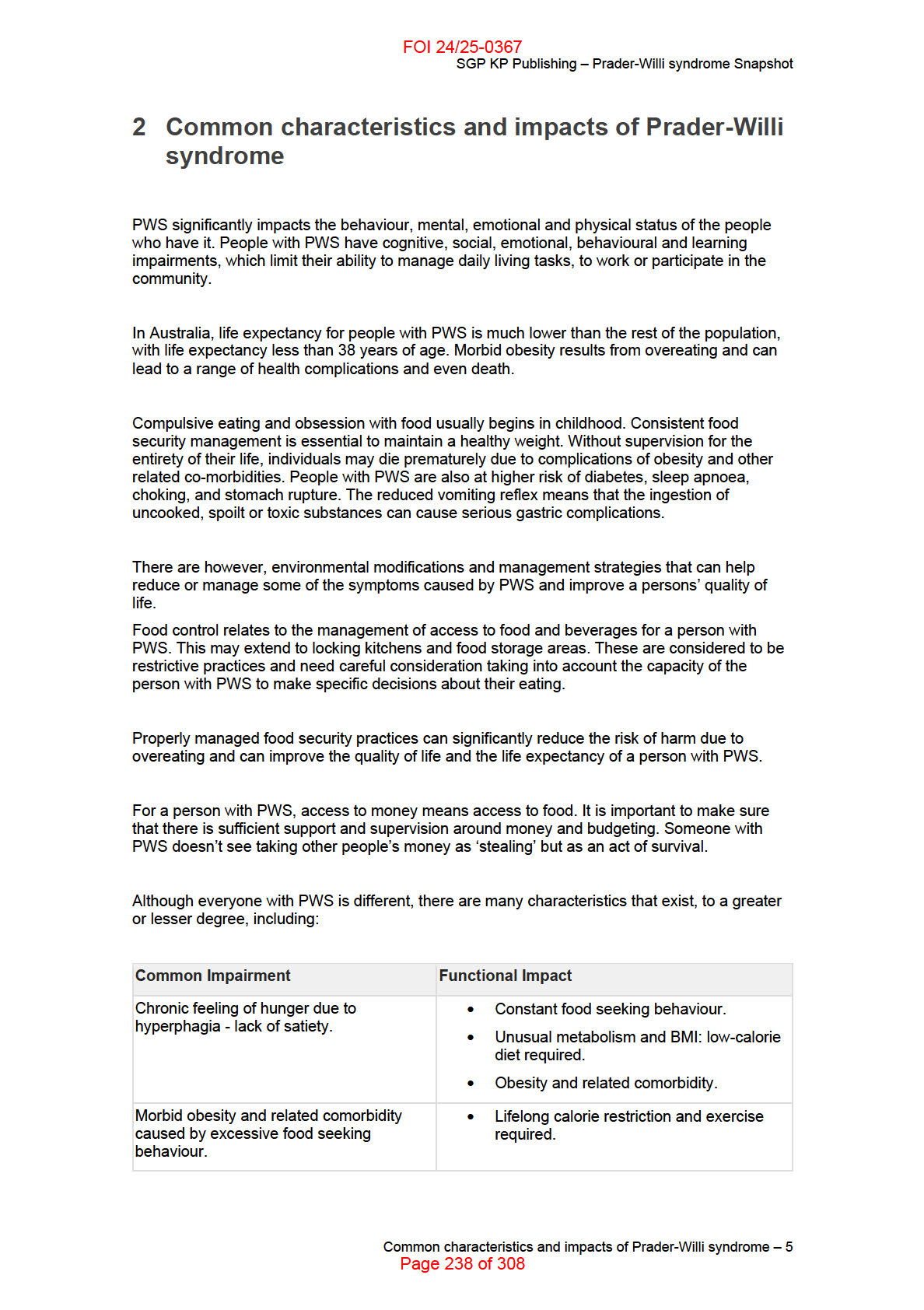
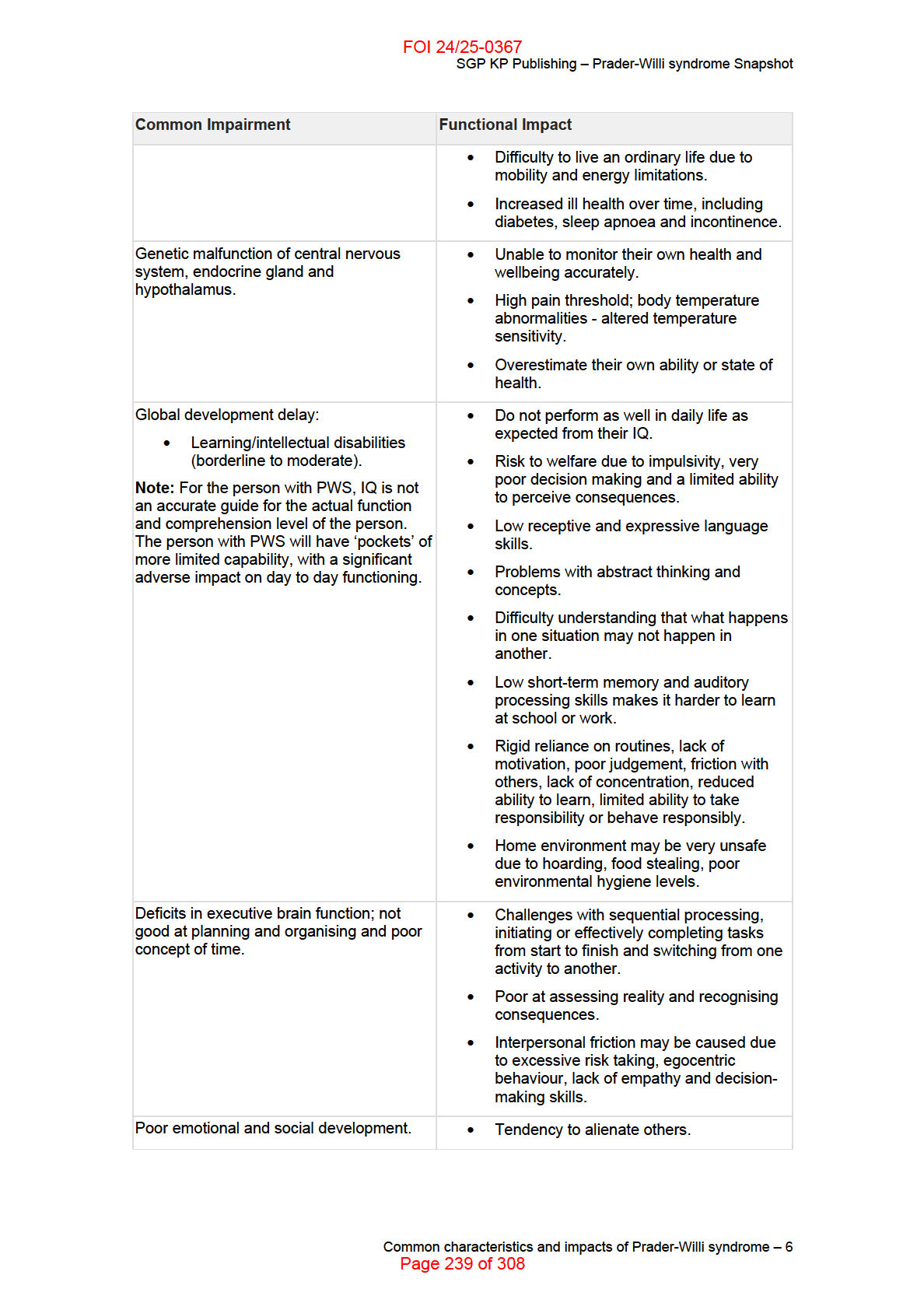
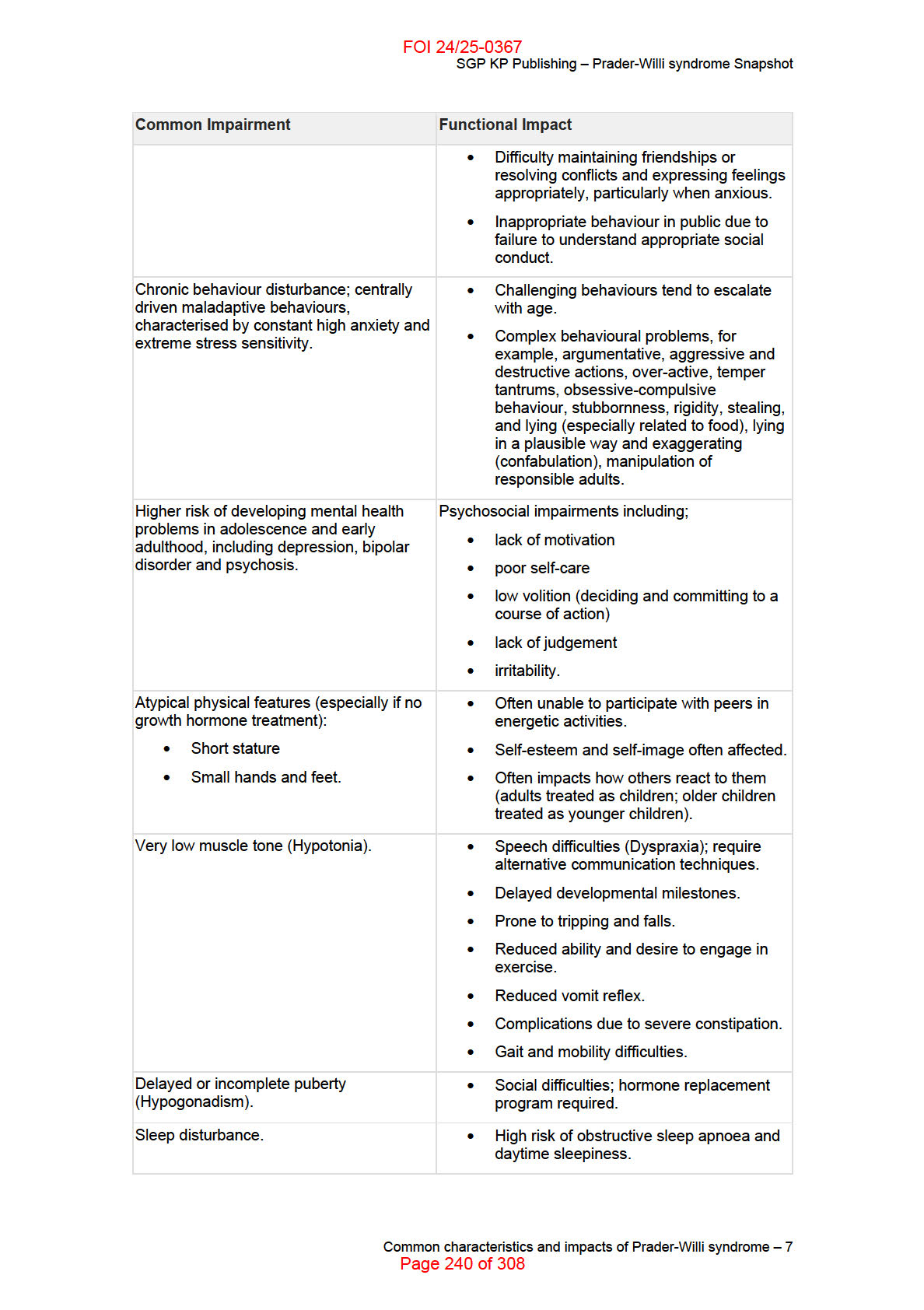
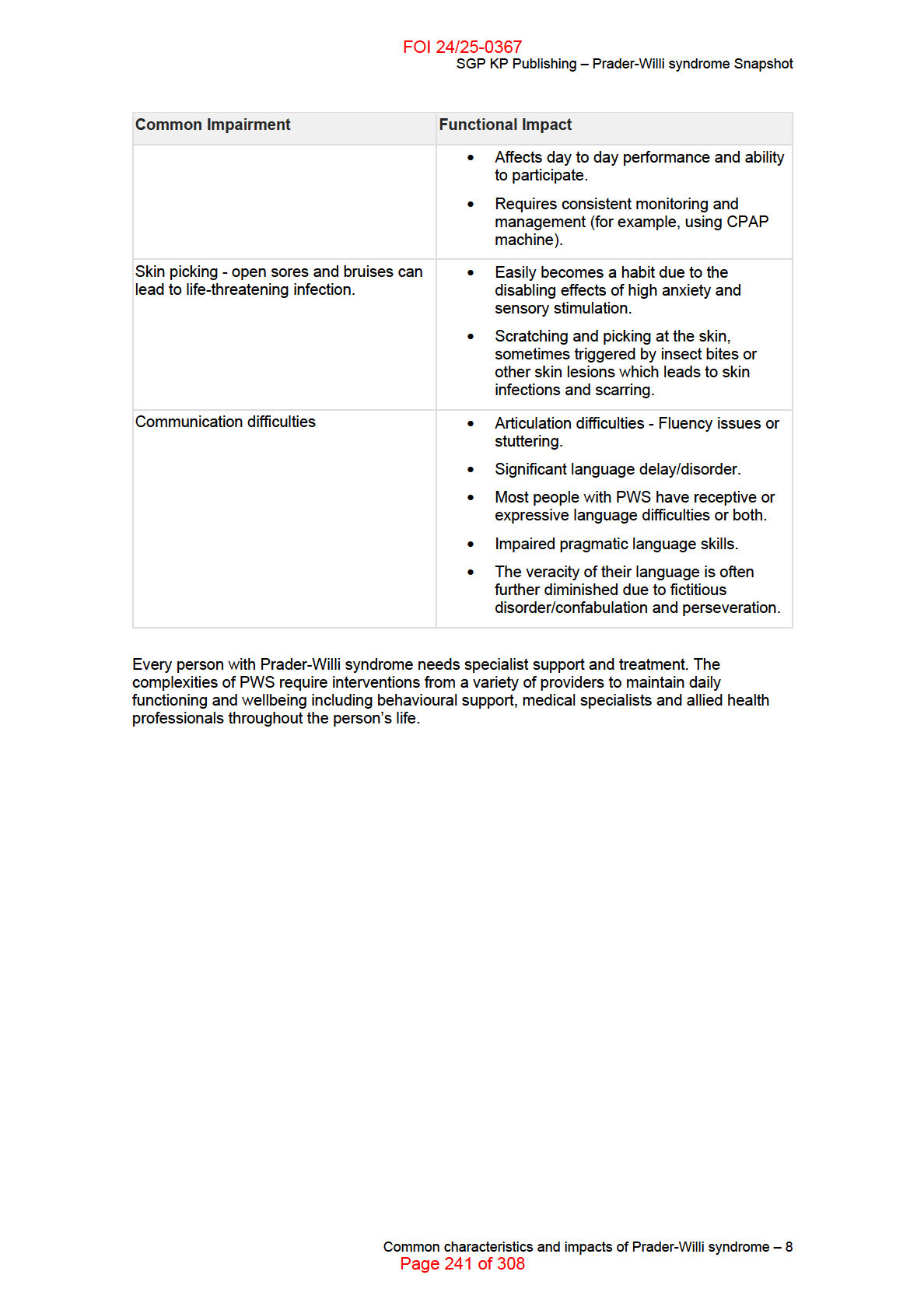
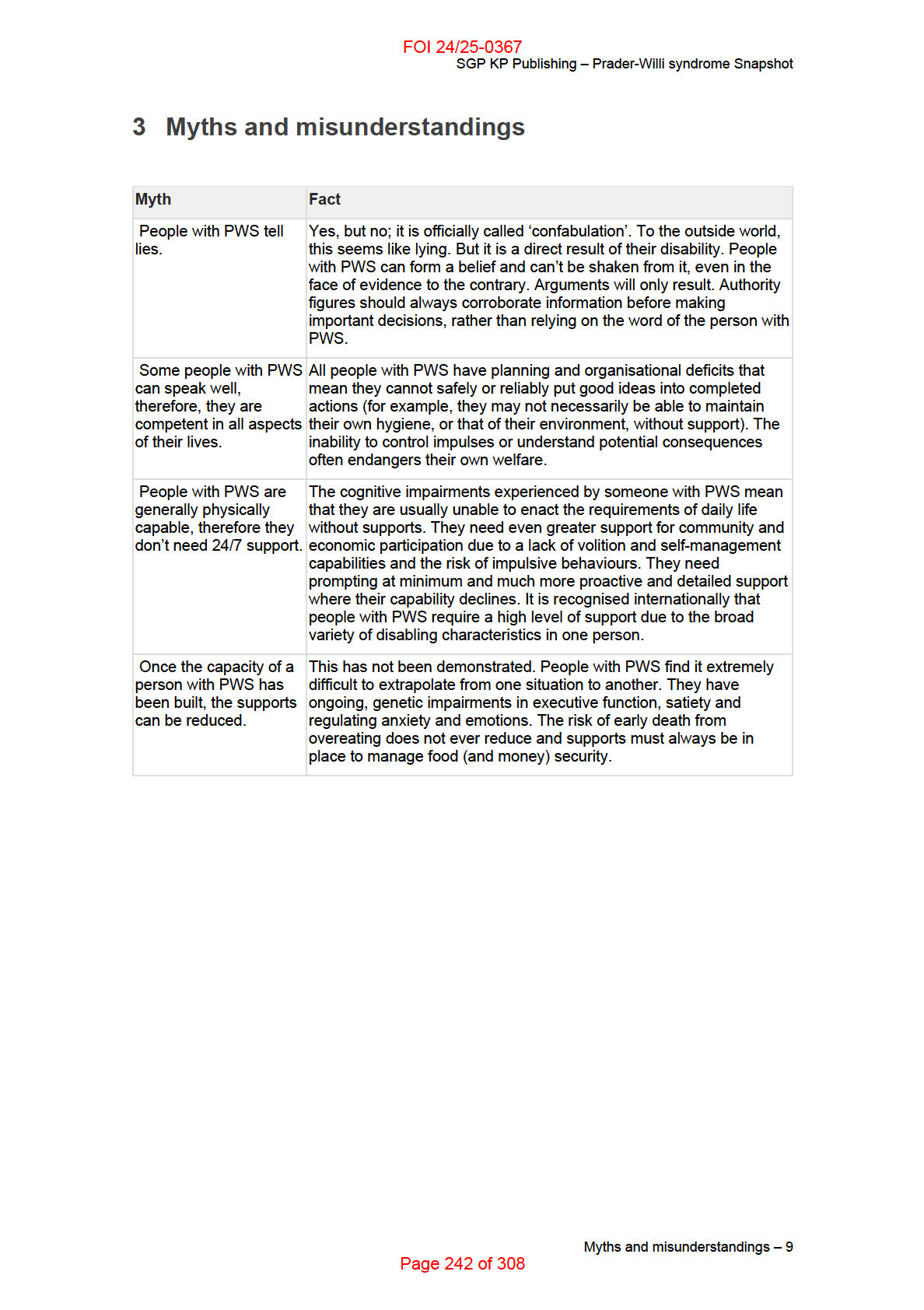
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Prader-Wil i syndrome Snapshot
4 Common barriers to social and economic
participation
People with PWS have the same aspirations as everyone else; to be in a loving relationship, to
have friends, to participate in community life and work and to feel included as full citizens.
However, like many people with disability, people with PWS encounter multiple barriers to
social, economic and civic participation. These barriers include discriminatory attitudes,
perceptions and misconceptions as well as environmental and social barriers.
• Community attitudes
o Lack of community awareness and understanding about the complexities of
PWS resulting in stigma and exclusion.
• Difficulty accessing services in the mainstream community
o Limited community resources and venues to support people with PWS to be
included in the community such as sporting clubs and public spaces.
o Reluctance on the part of organisations and facility staff to seek training and
explore ways to support people with PWS who want to access mainstream
activities and facilities.
o Inadequate access to mental health services where there has been a tendency
to attribute difficult behaviour to the intellectual disability, rather than an
emerging mental il ness.
• Education
o Reluctance on the part of schools to fund professional development, PWS
training and explore ways to support people with PWS so they can access and
participate in the full school curriculum.
• Difficulty accessing and maintaining employment.
• Housing
o Lack of housing options that provide safe and supported accommodation that
meets the specific needs of the person with PWS including substantive support,
food security and adequate staffing capabilities.
• Transport
o Lack of flexible transport arrangements and supports to allow management of
unsupervised access to food and challenging behaviours.
o While people with PWS are able to physically use public transport, it may not
be an option all the time, for reasons of safety for the person with PWS and
those around them.
Common barriers to social and economic participation – 10
Page 243 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Prader-Wil i syndrome Snapshot
5 What is the role of the family in providing support?
Families provide different levels of support to the person with PWS depending on the individual
family circumstances. Usually they play an active role in the areas of management of food
security, dietary and exercise management, supporting daily living tasks, medical care, money
management and advocating on their behalf. This is often beyond the age that you would
generally expect a parent or family member to provide support.
Parents of children with PWS consistently report higher levels of stress than families of other
complex disabilities and have higher incidence of family relationship problems. This is often due
to the 24/7 vigilance required to manage the hyperphagia and other behavioural problems such
as aggression.
Even if the person with PWS transitions to supported accommodation the family often chooses
to remain involved to advocate for their family member. Where possible, families may choose to
also have a role in attending medical and allied health appointments. But due to the extensive
list of medical and allied health appointments, parents and family members may find this difficult
to manage.
Consideration should be given to a holistic approach when reviewing informal supports to
maintain sustainability and to safeguard against disintegration of the family unit.
What is the role of the family in providing support? – 11
Page 244 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Prader-Wil i syndrome Snapshot
6 How can I tailor a meeting to suit a person with
PWS?
It is important to be aware of the characteristics of PWS before you meet someone with PWS.
There is a high risk of underestimating the difficulties experienced by someone with PWS and
this can lead to inadequate support and a decline in the participant’s health, safety and
wellbeing.
People with disability are presumed to have capacity to make decisions that affect their lives.
Every effort must be made to enable the leadership and participation of the person with PWS in
meetings. It is a good idea to make sure that an appropriate support person is included in the
meeting to confirm facts and provide additional information. People with PWS are prone to
confabulation and you should attempt to corroborate information with family/carers. It is also
important to give family/carers an opportunity to talk about their role in providing informal
supports and whether the NDIS can help them to take a break.
Consider what wil support a successful planning meeting. Prior to any meetings it may be
helpful to consider the following:
Before the meeting:
• Provide any written material in Easy English or other languages on request prior to the
meeting.
• Provide as much information about the purpose of the meeting in advance so the
person with PWS and their support person can prepare their answers thus reducing the
stress level at the actual meeting.
• Al ow more time for the meeting, as the person may want to revisit some of the
discussion to understand and assimilate the information and alleviate their anxiety.
• People with PWS frequently have a minimal sense of time. So, realistic planning for a
day, week, month, year or the future wil be difficult for them to conceive of or act upon,
despite the words they say to you.
• If a change of accommodation is planned, see the Prader-Willi Syndrome Australia
Residential guide.
• The person may have some mobility difficulties (for example, low muscle tone or
obesity), tire easily and need ready access to a toilet.
Communication during the meeting:
• Be aware that the person with PWS may be able to speak to you clearly, with good
expressive language. However, they have a relatively poor level of comprehension and
typical y:
• May lie and exaggerate about themselves and their circumstances (confabulation),
putting themselves at risk
• Wil unreliably report on their state of health
• Have poor short-term memory and auditory processing difficulties and find it hard to
take in lots of information, especially in conversation
How can I tailor a meeting to suit a person with PWS? – 12
Page 245 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Prader-Wil i syndrome Snapshot
• Can think through things slowly, ask questions and understand small amounts of
information at a time.
• Speak in short sentences; allow enough time for the person to think and respond. Avoid
jargon, slang or acronyms.
• Look for body cues that the participant is not telling the truth such as avoiding eye
contact more than previously.
• Address the questions to the person with PWS rather than the support person. The
person with PWS may elect to request assistance from their support person.
• Speak respectfully to the person with PWS in an age appropriate fashion.
• Rephrase or repeat the question if you or the support person suspect they haven’t
understood the question.
• Be patient, as the person with PWS wil need time to process the response.
• People with PWS tend to be literal thinkers. Do not make any comments that may be
interpreted literally, or promises that you cannot keep.
• People with PWS often give answers that attempt to please others. Use a variety of
questioning techniques to try to get the participant’s own views.
• Information supplied by the person with PWS which wil be used to make decisions may
need to be corroborated by another party. Ensure you apply reasonable and necessary
decision making to determine any appropriate funded supports to be included in the
participants plan.
How can I tailor a meeting to suit a person with PWS? – 13
Page 246 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Prader-Wil i syndrome Snapshot
7 Helpful links for further information
Prader-Wil i Syndrome Association of Australia
Guide for NDIA Technical Advisory Branch (for staff members who are providing advice during
planning or reviewing a plan for a person with PWS)
Clinicians and Al ied Health Professionals advice
Best Practice Guidelines for Residential Care
Prader-Wil i Syndrome: A Primer for Psychiatrists
Prader-Willi Syndrome Association UK
Prader-Willi Syndrome Association (USA)
International Prader-Wil i Syndrome Organisation
Helpful links for further information – 14
Page 247 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Prader-Wil i syndrome Snapshot
8 Representative bodies consulted when developing
this Snapshot
In developing this resource, the NDIA consulted with the Disability Advocacy Network Australia
who worked with Prader-Wil i Syndrome Australia to develop this snapshot.
Representative bodies consulted when developing this Snapshot – 15
Page 248 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 20
Psychosocial Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:14:01
Page 249 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
Table of Contents
1
Peak body consulted ........................................................................................................... 4
2
What is psychosocial disability? ........................................................................................ 5
3
How is psychosocial disability identified? ........................................................................ 6
4
Language and terminology ................................................................................................. 7
5
Enabling social and economic participation ..................................................................... 8
6
Families and carers ............................................................................................................ 10
7
How can I tailor a meeting to suit a participant with psychosocial disability? ........... 11
8
What people with psychosocial disability want you to remember ............................... 12
9
Helpful links ........................................................................................................................ 13
Table of Contents – 2
Page 250 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
This Disability Snapshot provides general information about psychosocial disability to assist you
in communicating effectively and supporting participants to develop their goals. Each person is
an individual with their own needs, preferences and experiences. This information has been
prepared for NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 251 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with Community Mental Health Australia (CMHA) and
Mental Health Coordinating Council of NSW (MHCC).
Peak body consulted – 4
Page 252 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
2 What is psychosocial disability?
Psychosocial disability refers to the social and economic consequences related to mental health
conditions. It is used to describe the challenges, or limitations, a person experiences in life that
are related to mental health conditions. This may include challenges or limitations in their
capacity to:
have a good social network including friends and a family of their own
participate fully in life
experience full physical health
manage the practical, social and emotional aspects of their lives
engage in education, training, cultural activities and economic participation
achieve their goals and aspirations.
The impact of psychosocial disability can vary over time because of the difficulties people
experience with mental health conditions and many other factors in the individual’s life. Not
everyone living with mental health conditions will experience a significant psychosocial disability
and individuals will experience psychosocial disability differently.
In Australia, people with a psychosocial disability make up a significant proportion of Australia’s
most disadvantaged population. People with a mental illness (21.7%) are the second largest
group receiving the Disability Support Pension.
People with psychosocial disability may also have lived and living experience related to trauma,
suicidal ideation, and substance use. The complexity of this means you should adopt a whole of
person approach.
What is psychosocial disability? – 5
Page 253 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
3 How is psychosocial disability identified?
A person may be diagnosed with a mental health condition, but psychosocial disability is not a
diagnosis. Psychosocial disability is
identified by the impacts of, or impairment resulting from,
the person’s mental health conditions.
A health professional such as a GP, psychiatrist or allied health professional may identify
psychosocial disability through assessment or testing.
Impairment resulting from psychosocial disability can be episodic or fluctuating. To understand
the functional impact and psychosocial disability for an individual, it can be helpful for an allied
health professional (for example occupational therapist, psychologist, speech therapist, social
worker) to provide an overall assessment of the person’s functioning.
It is important that the assessment considers the impacts in relation to:
mobility
communication
social
interaction
learning
self-care
decision-making.
Psychosocial disabilities often include cognitive difficulties which may affect function in the
areas of:
memory
communication
organising and planning skills
social
interactions
visual
interpretation.
The symptoms of a mental health condition may be of an episodic nature and vary in intensity
and need for support. How this impacts on psychosocial disability may mean that there will be
times when a person may experience significant limitations; while at other times they may be
able to go about their daily life without experiencing the same challenges.
How is psychosocial disability identified? – 6
Page 254 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
4 Language and terminology
When talking with or about a person with a psychosocial disability, use ‘person first’ language.
For example, saying ‘person living with a psychosocial disability’ rather than ‘disabled person’.
People with mental health conditions usually prefer not to be defined by them. Using strength-
based language, rather than focusing on a person’s limitations, maximises a person’s sense of
self, and independence.
The term ‘recovery’ is used widely throughout the mental health service system and can have
different meanings for different professionals/disciplines and people accessing the services. The
NDIA defines recovery as achieving an optimal state of personal, social and emotional
wellbeing, as defined by each individual, whilst living with or recovering from a mental health
condition.
Recovery is an individual and unique process. It is defined by the person and driven by their
needs and preferences.
Recovery involves:
having
hope
being
motivated
feeling optimistic about the future
having the skills and strategies to manage the challenges the participant may
experience
ensuring that services are delivered using a trauma-informed recovery-oriented practice
approach.
It is important to use language that reflects the recovery-based approach. You can find more
information on recovery-orientated language in the Helpful Links section and in the Practice
Guide – Psychosocial Disability.
Language and terminology – 7
Page 255 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
5 Enabling social and economic participation
Some of the consequences of psychosocial disability may include:
poverty
discrimination
unemployment
poor educational outcomes
poor
housing.
The relationship between these consequences and the underlying mental health condition can
be interconnected and two-way. For example, loss of connection with family, friends and
community can worsen a participant’s mental health. It is important to focus on building and
maintaining social connection and relationships.
The earlier a person connects with services and supports, the better. The episodic nature of a
mental health condition may vary on a day-to-day basis or over the person’s life span, and their
plan needs to be flexible enough to respond effectively.
A self-directed, strengths-based, trauma-informed, recovery-oriented approach to a person’s
mental health and well-being is highly effective. This may mean working with the person to help
them identify some safe activities to start such as building their social networks or getting back
into work. Capacity building supports are important to this approach as well as core and
assistive technology supports. Adopting a
strengths-based approach in supporting the
participant to identify their goals, objectives and aspirations is vital to build rapport and develop
independence. In using a strengths-based recovery approach, you will focus on the participant’s
talents, positive attributes and potential and identify how that will help them to achieve their
goals.
Capacity building supports:
A
Recovery Coach support can provide assistance in building capacity and resilience
in people with psychosocial disability and support them to live a more fulfilling life.
Recovery coaches work with participants, families, carers, and other services to get the
best outcomes from NDIS supports.
A
support coordinator can be effective in maintaining continuity of supports and
allows for supports to be increased quickly and/or accessed at short notice as needed.
Support coordinators can also ensure appropriate support is available around
transitions from hospital to community, and that an ongoing relationship is there to
facilitate engagement in social, economic and community life.
An
occupational therapist with specialist knowledge in mental health can assess
functional capacity and provide support in maintaining a job, volunteer role, study,
and/or social networks.
An
exercise physiologist can provide an accessible and achievable exercise program
to support a person’s mental health and build community networks.
Core supports:
A functional home environment can improve mental health.
Support workers can
assist with daily living activities in the home like meal preparation and cleaning.
Support workers can also assist with and encourage participation in an exercise plan
given by an exercise physiologist and promote self-care with regards to personal care
and physical health.
Access
to
community groups can help facilitate social inclusion and build
relationships.
Enabling social and economic participation – 8
Page 256 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
Assistive Technology (AT):
AT can provide both functional and emotional support for example by assisting
individuals to learn new information and build organisation, concentration and planning
skills.
Enabling social and economic participation – 9
Page 257 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
6 Families and carers
Family, friends, carers and kinship groups play an important role in a person’s recovery. Mental
health carers can include a parent caring for a child, an adult caring for a partner, friend, parent,
or sibling, or a child caring for a parent. Due to the episodic nature of mental health conditions,
people living with psychosocial disability may require regular on-call care. Family members
often provide care for many years, often either in their own home or the home of the person
living with psychosocial disability.
Other informal supporters are often unexpectedly called upon to play a role in mental health
care. They may have found themselves in this carer role because they see it as part of their
relationship with the person with psychosocial disability. Nevertheless, they may not think of
themselves as a ‘carer’.
It is important to consider whether the level of care provided by family members, carers or
informal supports is sustainable. It may be reasonable and necessary to include core supports
and respite to prevent carer burnout. To support carers and family members in this role, provide
them with relevant resources and information.
Refer to the
Helpful Links section for more information.
Families and carers – 10
Page 258 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
7 How can I tailor a meeting to suit a participant with
psychosocial disability?
Many people who live with psychosocial disability may have experienced trauma in their life and
can become distressed if they do not feel safe. To facilitate a sense of safety make sure you:
Allow enough notice for the person to prepare for meetings (ideally four weeks) and be
clear about what ‘prepared’ means.
Consider the environment and ask the person what helps them feel safe in a room. Let
them know the choices they have, such as having the meeting in a familiar place,
having a support person with them, and whether the gender of the support person and
the NDIA representative is important. A support person may need to be invited to attend
as they can be particularly important to help convey a person’s needs.
Provide easy access to exits and offer breaks or follow-up meetings.
Be honest and clear about what you can and can’t do. Set boundaries and expectations
early and allow the person to set their own boundaries if possible.
Maintain confidentiality and be clear about what information will be kept and what it will
be used for.
Provide information about your recommendations and why they are relevant, even if it
seems obvious.
Ensure the participant understands what choice and control means in the conversation.
People may feel very disempowered by those they see as ‘authority figures’ and may
feel intimidated. Encourage the person to take part in the process, allow them space
and time to speak up. An example question could be: “Is this the ideal outcome today
from your point of view? How do you think we could achieve this?”
Listen non-judgmentally and collaborate with the person to clarify their need. Ask the
person what they find important and don’t make assumptions. Use paraphrasing and
clarifying questions to understand their wants and needs.
Use the Reimagine Workbook (see the Helpful Links section) which has a tool to use in
collaboration with the participant.
How can I tailor a meeting to suit a participant with psychosocial disability? – 11
Page 259 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
8 What people with psychosocial disability want you
to remember
People living with psychosocial disability have first-hand knowledge of what they
experience.
Involving a support person in a planning meeting can help the participant feel safer and
more confident to ask for what they need and don’t want.
The road to recovery varies from person to person.
People with psychosocial disability often experience stigma and discrimination which
can be highly distressing.
Psychosocial disability is not a visible disability, but the impact on a person’s life is very
real.
Take the concerns of the person living with psychosocial disability seriously.
Social inclusion and community connection are significant to recovery.
What people with psychosocial disability want you to remember – 12
Page 260 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Psychosocial Disability Snapshot
9 Helpful links
Reimagine
Reimagine my life Workbook
Mental Health Carers Australia
Recovery Oriented Language Guide
Unravelling Psychosocial Disability Booklet
Practice Guide – Psychosocial Disability
Guide - Conversation style guide
Helpful links – 13
Page 261 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 21
Schizophrenia Disability Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:14:12
Page 262 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Schizophrenia Disability Snapshot
Table of Contents
1 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 What is schizophrenia? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 Schizophrenia is characterised by symptoms that are grouped as positive, negative
and cognitive: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 How is schizophrenia diagnosed? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
5 Language and terminology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 Enabling social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
7 How can I tailor a meeting to suit a participant with schizophrenia?. . . . . . . . . . . . . . 10
8 Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
Table of Contents – 2
Page 263 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Schizophrenia Disability Snapshot
This Disability Snapshot provides general information about schizophrenia. It wil assist you in
communicating effectively and supporting the participant in developing their goals in a planning
meeting. Each person is an individual and wil have their own needs, preferences and
experiences that wil impact on the planning process. This information has been prepared for
NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 264 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Schizophrenia Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with Mental Health Australia.
Peak body consulted – 4
Page 265 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Schizophrenia Disability Snapshot
2 What is schizophrenia?
Schizophrenia is an established medical disorder that is common worldwide. Up to 1 in 100
people wil experience schizophrenia.
What is schizophrenia? – 5
Page 266 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Schizophrenia Disability Snapshot
3 Schizophrenia is characterised by symptoms that
are grouped as positive, negative and cognitive:
•
positive symptoms are intense episodes of psychosis, in which a person may
experience auditory and/or sensory hallucinations and delusional beliefs, including
paranoia. Psychosis can make it difficult for a person to distinguish between what is real
and what isn’t real
•
negative symptoms are often characterised by reduced expression and/or reduced
motivation and/or a reduced capacity to function in everyday life
•
cognitive symptoms generally relate to attention, memory, verbal skil s and may
include longer periods of slowed or confused thinking.
Antipsychotic medicines are the main form of treatment for schizophrenia.
It is important to note that people experiencing schizophrenia do not have a split or multiple
personalities and they are not inherently more prone to violence. In fact they are more likely to
become a victim of violence.
Schizophrenia is characterised by symptoms that are grouped as positive, negative and cognitive: – 6
Page 267 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Schizophrenia Disability Snapshot
4 How is schizophrenia diagnosed?
Schizophrenia may take time to diagnose. A person wil only receive a confirmed diagnosis of
schizophrenia after experiencing one month of psychotic symptoms and six months of reduced
functioning.
A GP or other medical professional might make the initial assessment, and would then refer the
person to a specialist, usually a psychiatrist for diagnosis. The specialist might then make a
working diagnosis of schizophrenia, so that treatment can begin without delay.
There is no known biological marker for schizophrenia. Schizophrenia is primarily a clinical
diagnosis, it is diagnosed by identifying signs and symptoms and monitoring how the symptoms
develop over time.
How is schizophrenia diagnosed? – 7
Page 268 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Schizophrenia Disability Snapshot
5 Language and terminology
People living with mental il ness don’t like to be defined by their diagnosis, to be stigmatised or
have assumptions made about them. Therefore phrases such as ‘schizophrenia sufferer’ or
‘he’s a psychotic’ are inappropriate.
Instead say:
• she lives with schizophrenia
• she has had an experience of schizophrenia
• he has had an experience of psychosis
• person living with schizophrenia
• the person has schizophrenia.
Language and terminology – 8
Page 269 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Schizophrenia Disability Snapshot
6 Enabling social and economic participation
Support to participate in the community and in work can help prevent social isolation and
promote recovery and wellness for people living with schizophrenia. It is important to explore
how a person with schizophrenia can be supported to participate in activities, education and
employment, taking into consideration their interests and aspirations as an individual.
NDIS supports can assist participants build life skil s, capabilities and greater independence.
This may include being supported through a vocational ‘discovery’ process to explore their
strengths and interests in the context of work, particularly for young people transitioning from
school into employment.
Early access to pre-vocational training and employment opportunities can improve long-term
outcomes in both employment and education. Peer support from other people living with
schizophrenia can also play a key role in improving participation in work and the community.
Volunteering can also be a first step in building confidence and exploring the person’s interests
and strengths.
Enabling social and economic participation – 9
Page 270 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Schizophrenia Disability Snapshot
7 How can I tailor a meeting to suit a participant with
schizophrenia?
People experiencing schizophrenia are above all, individuals the same as you and me. No two
people with schizophrenia are alike, they wil experience schizophrenia in different ways and
their needs wil vary as much as anyone else. They enjoy family, friends, have a sense of
humour, sporting interests and like to participate in all aspects of the community.
Many people living with schizophrenia are indistinguishable from people without the condition
and they may not require any special considerations or treatment.
However, a person experiencing schizophrenia may be affected by slowed or confused thinking,
or reduced expression, motivation and functioning. They may also experience distressing side-
effects of their medication. This may mean the person might require more time than usual to
understand what is being said and to compose or express their thoughts.
When meeting with a person with schizophrenia, provide a quiet, respectful and calm
environment. Al ow the person the time they need. Avoid the temptation to finish their sentences
or rush them. Do not assume you know what they need or want.
A person experiencing active psychotic symptoms, delusional beliefs and/or sensory
hallucinations may find it very difficult to concentrate and to trust the situation they are in. They
may feel irritated, agitated or frightened. Remain calm, show respect and compassion and focus
on how they feel, rather than the details of their delusions or hallucinations.
How can I tailor a meeting to suit a participant with schizophrenia? – 10
Page 271 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Schizophrenia Disability Snapshot
8 Helpful links
• Spotlight on Schizophrenia — SANE Australia website.
Helpful links – 11
Page 272 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 22
Spinal Cord Injury Disability
Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:14:43
Page 273 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Spinal Cord Injury Disability Snapshot
Table of Contents
1 Peak body consulted . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 What is Spinal Cord Injury? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 How is Spinal Cord Injury diagnosed? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
4 Language and terminology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
5 Enabling social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
6 Families and carers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
7 How can I tailor a meeting to suit a participant with Spinal Cord Injury? . . . . . . . . . . 10
8 What people with Spinal Cord Injury want you to remember . . . . . . . . . . . . . . . . . . . . 11
9 Helpful links . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12
Table of Contents – 2
Page 274 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Spinal Cord Injury Disability Snapshot
This Disability Snapshot provides general information about Spinal Cord Injury to assist you in
communicating effectively and supporting the participant in developing their goals. Each person
is an individual and wil have their own needs, preferences and experiences. This information
has been prepared for NDIA staff and partners and is not intended for external distribution.
Peak body consulted – 3
Page 275 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Spinal Cord Injury Disability Snapshot
1 Peak body consulted
In developing this resource we consulted with Spinal Cord Injuries Australia.
Peak body consulted – 4
Page 276 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Spinal Cord Injury Disability Snapshot
2 What is Spinal Cord Injury?
Spinal Cord Injury (SCI) occurs as a result of trauma or catastrophic injury such as a fall or car
accident, or from a medical condition such as a stroke or other spine conditions. The impacts of
an injury wil depend on where it occurs on the spine. Generally, the higher the injury level on
the spine, the greater the functional impairment.
The types of SCI are:
•
Quadriplegia or Tetraplegia which is motor or sensory impairment of all four limbs
caused by SCI above the first thoracic vertebrae in the cervical spine.
•
Paraplegia which is impairment in motor or sensory function of lower extremities
caused by SCI below the seventh cervical vertebrae in the thoracic, lumbar or sacral
spine.
Each injury is either
complete, with no movement or sensation below the level of injury, or
incomplete which means there is some sensation and/or movement below the injury level.
As a result of SCI, an individual may experience the fol owing:
• bowel or bladder dysfunction
• skin issues such as pressure areas or skin breakdown because of mobility
• difficulty regulating body temperature and increased likelihood of hypothermia
(dangerously low)
• sexual dysfunction
• autonomic dysreflexia (overactivity of the autonomic nervous system), commonly
caused by bladder, bowel or skin irritation, which can lead to seizures, stroke or death if
not managed immediately and correctly.
What is Spinal Cord Injury? – 5
Page 277 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Spinal Cord Injury Disability Snapshot
3 How is Spinal Cord Injury diagnosed?
SCI is an acquired disability diagnosed by a neurosurgeon or spinal physician using the
American Spinal Injury Association classification for motor and sensory impairment level. Spinal
cord injuries lead to paralysis, which means that people wil often spend many months in
hospital in a specialist spinal injury unit for intervention and rehabilitation. Physiotherapists and
occupational therapists may provide treatment and rehabilitation.
How is Spinal Cord Injury diagnosed? – 6
Page 278 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Spinal Cord Injury Disability Snapshot
4 Language and terminology
When talking with a person with a spinal cord injury, you should focus on the person, not the
impairment. Inclusive person first language should generally be used, but some people have
their own preferences. Avoid negative language such as ‘wheelchair-bound’. A wheelchair is a
mobility aid supporting independence; ‘wheelchair user’ is an appropriate term.
Language and terminology – 7
Page 279 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Spinal Cord Injury Disability Snapshot
5 Enabling social and economic participation
As SCI is an acquired disability, it is likely a person’s routine and activities before their injury will
have been severely disrupted. They may need time to come to terms with their disability and
support to re-engage in social and economic participation. Some people with SCI may be able
to continue with their role with some workplace adjustments. However if they cannot continue
working in their pre-injury role, many others may need to develop or relearn skil s, look for a
different career or participate in vocational training to re-enter the workforce. You should
consider these factors when discussing employment goals, and include employment related
supports in the participant’s plan.
Social and community participation is important to build confidence and connect with people as
the person with SCI adjusts to their new reality of impairment. The impact of the injury wil vary
for each person, so supports wil need to be highly individualised.
Supports to enable the participant’s social and economic participation may include assistive
technology (AT) such as:
• manual and power wheelchairs and other mobility aids to help get around
• equipment to maintain good health and facilitate independence, such as electric beds,
pressure relieving mattresses and wheelchair cushions, and shower commode chairs
• environmental control units that allow for controlling the home, including lights, doors
and electrical appliances
• speech recognition software for home, education and vocational needs.
People with SCI may use consumables associated with incontinence. These items, and the
daily regimes to manage bowel and bladder function, are important for ongoing social and
economic participation.
Enabling social and economic participation – 8
Page 280 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Spinal Cord Injury Disability Snapshot
6 Families and carers
SCI is a significant injury and it has a long-term impact on the individual and their family
members. SCI wil cause many individuals and their families to experience sudden and
significant changes following the injury. It is important for the individual and their family to take
some time to learn about the injury and adjust to the disability and changes in the individual’s
life.
The role that family plays after an injury is different for everyone. This wil depend on their age
and how they balance formal and informal supports for assistance with daily living, personal
care, and social and economic participation. It may take some time for the individual and their
family members or carers to find supports and strategies to manage SCI.
Family members and carers may feel overwhelmed as they support the person with SCI, as well
as balance other commitments such as work and the needs of other family members. It is
important to offer support to the family during this time and offer strategies to balance informal
and formal supports and give carers a break. This can be through funded supports to offer the
participant independence from their family and provide respite to family members.
Families and carers – 9
Page 281 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Spinal Cord Injury Disability Snapshot
7 How can I tailor a meeting to suit a participant with
Spinal Cord Injury?
When meeting with a person with SCI, always communicate directly with the individual, even if
family members join them. Make sure the meeting is held in a place with accessible facilities
and that you give the person plenty of time to make themselves comfortable.
A person with SCI is likely to engage with the NDIS soon after their injury. They may stil be
undergoing rehabilitation and adapting to life with their disability. They may not know what
supports they need and how their condition wil progress over time. You should be mindful of
this when meeting them for the first time and deciding what supports to include in their first plan.
Consider following up with them before finalising their plan to see how they are adjusting and if
anything has changed, and whether any additional supports might be needed.
How can I tailor a meeting to suit a participant with Spinal Cord Injury? – 10
Page 282 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Spinal Cord Injury Disability Snapshot
8 What people with Spinal Cord Injury want you to
remember
• SCI is an acquired disability which wil require time to adjust to
• supports in a plan should empower the individual and focus on finding different ways to
engage in social and economic participation
• no two injuries are the same and each person should receive individualised support
• each person’s individuality and right of choice should be respected.
What people with Spinal Cord Injury want you to remember – 11
Page 283 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Spinal Cord Injury Disability Snapshot
9 Helpful links
• Spinal Cord Injuries Australia
• ParaQuad
• NSW Agency for Clinical Innovation - Spinal Cord Injury Resources
• Spinal Cord Injury Levels and Classification
Helpful links – 12
Page 284 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 23
Thalidomide Survivors Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:14:52
Page 285 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Thalidomide Survivors Snapshot
Table of Contents
1 About Thalidomide . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
2 The impact of Thalidomide . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
3 Common barriers to social and economic participation . . . . . . . . . . . . . . . . . . . . . . . . . 7
4 Common language and terminology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
5 Engaging with families and carers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
6 What specific supports might a Thalidomide Survivor need? . . . . . . . . . . . . . . . . . . . 10
7 How can I tailor a meeting with a Thalidomide survivor? . . . . . . . . . . . . . . . . . . . . . . . 11
8 Helpful links for further information . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12
Table of Contents – 2
Page 286 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Thalidomide Survivors Snapshot
This is a snapshot and is not designed to be a comprehensive guide. It provides general
information about Thalidomide Survivors for NDIA staff and partners and is not intended for
external distribution. Each Thalidomide Survivor has been impacted individually and wil have
their own needs, preferences and experiences that wil need to be taken into consideration
across the planning process.
In developing this resource, we consulted with Thalidomide Group Australia.
About Thalidomide – 3
Page 287 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Thalidomide Survivors Snapshot
1 About Thalidomide
Thalidomide was the active ingredient most commonly associated with the medication ‘Distaval’
and was marketed to pregnant women in the late 1950s and early 1960s, to ease symptoms of
morning sickness.
Though pregnant mothers had no way of knowing the effects of Thalidomide, taking just one
tablet during the first trimester could cause malformation of limbs, facial features and, significant
internal injuries to babies. Today, those adults living with Thalidomide disabilities are aged in
their mid to-late 50s. They identify as Thalidomide Survivors.
About Thalidomide – 4
Page 288 of 308
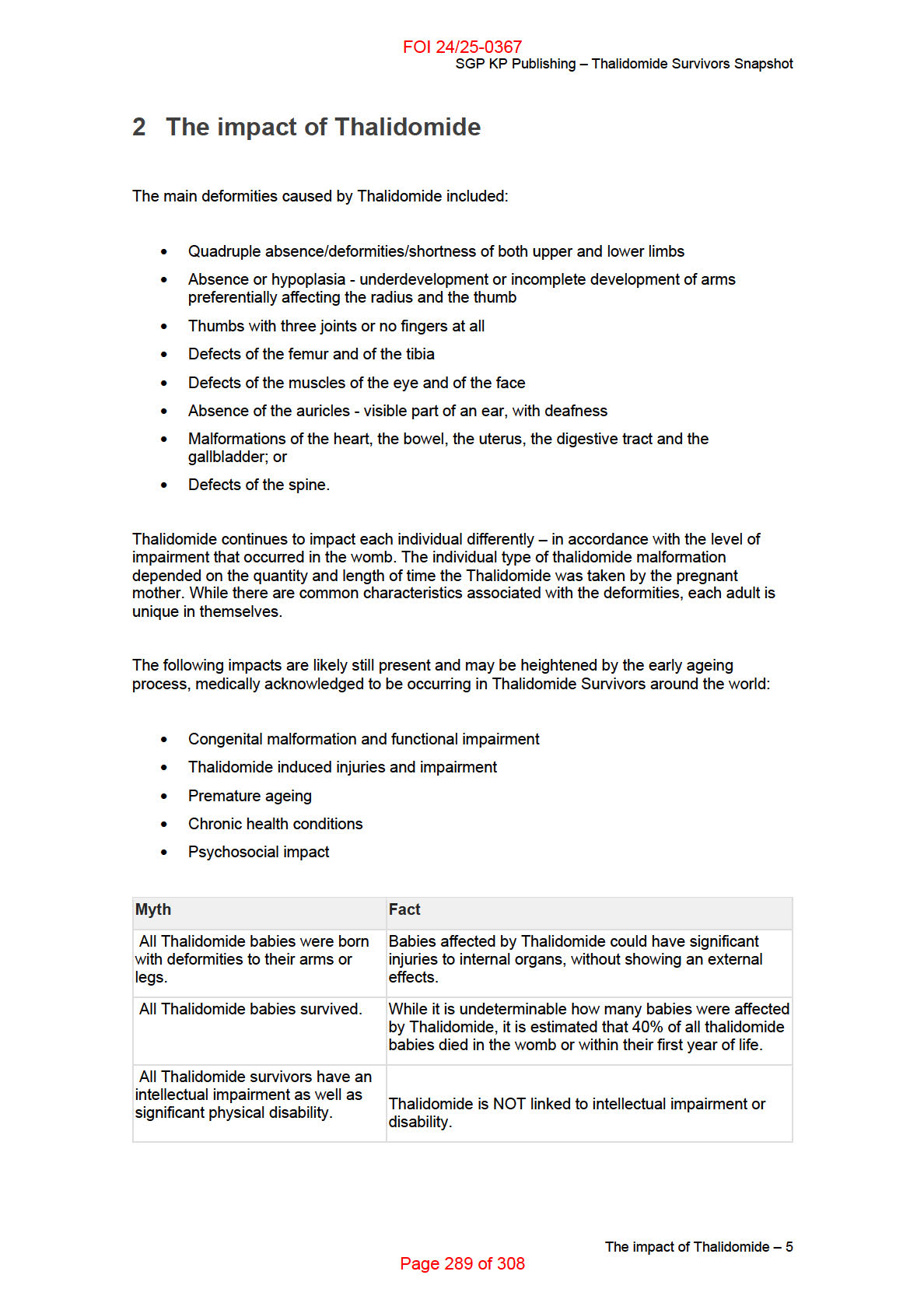
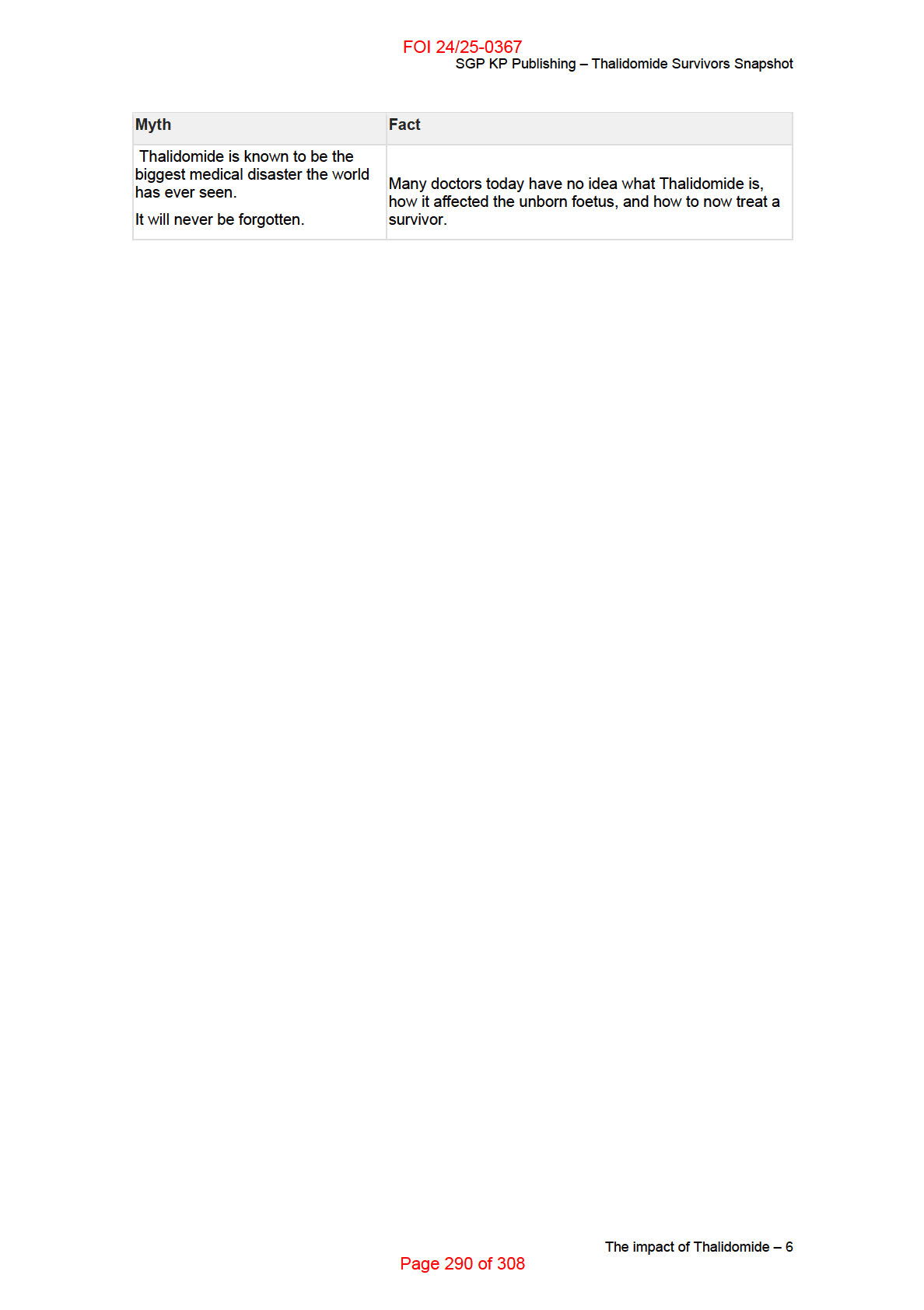
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Thalidomide Survivors Snapshot
3 Common barriers to social and economic
participation
Australia currently has around 150
recognised Thalidomide survivors. It is likely those numbers
may increase, should further investigations occur. The relative few numbers have not warranted
(until now) specialist Australian medical research – so there has been reliance on international
studies.
Research from the UK indicates that most people born affected by Thalidomide have gone on to
have happy lives with families and/or a career. However, the wear and tear on their bodies as
they get older has become increasingly noticeable. The Thalidomide Trust (UK) has recently
researched issues of health and wellbeing with all of their members and, the results show that
two-thirds rate their physical health as the same or worse than the lowest 2% of the general
population.
The key health problems noted are:
• pain that can be severe and / or continuous (90% of beneficiaries noted this)
• reduced flexibility and mobility that make it difficult to undertake everyday tasks;
• significant neurological impairment and pain;
• tingling and numbness and,
• poor reduced emotional resilience which in some people may lead to anxiety,
depression and suicide ideology.
The cost of specially tailored clothes, prosthetic limbs, wheelchairs and hearing aids/implants
has been noted as difficult to cover financially - particularly as many people find they are no
longer able to work due to their disability.
Common barriers to social and economic participation – 7
Page 291 of 308
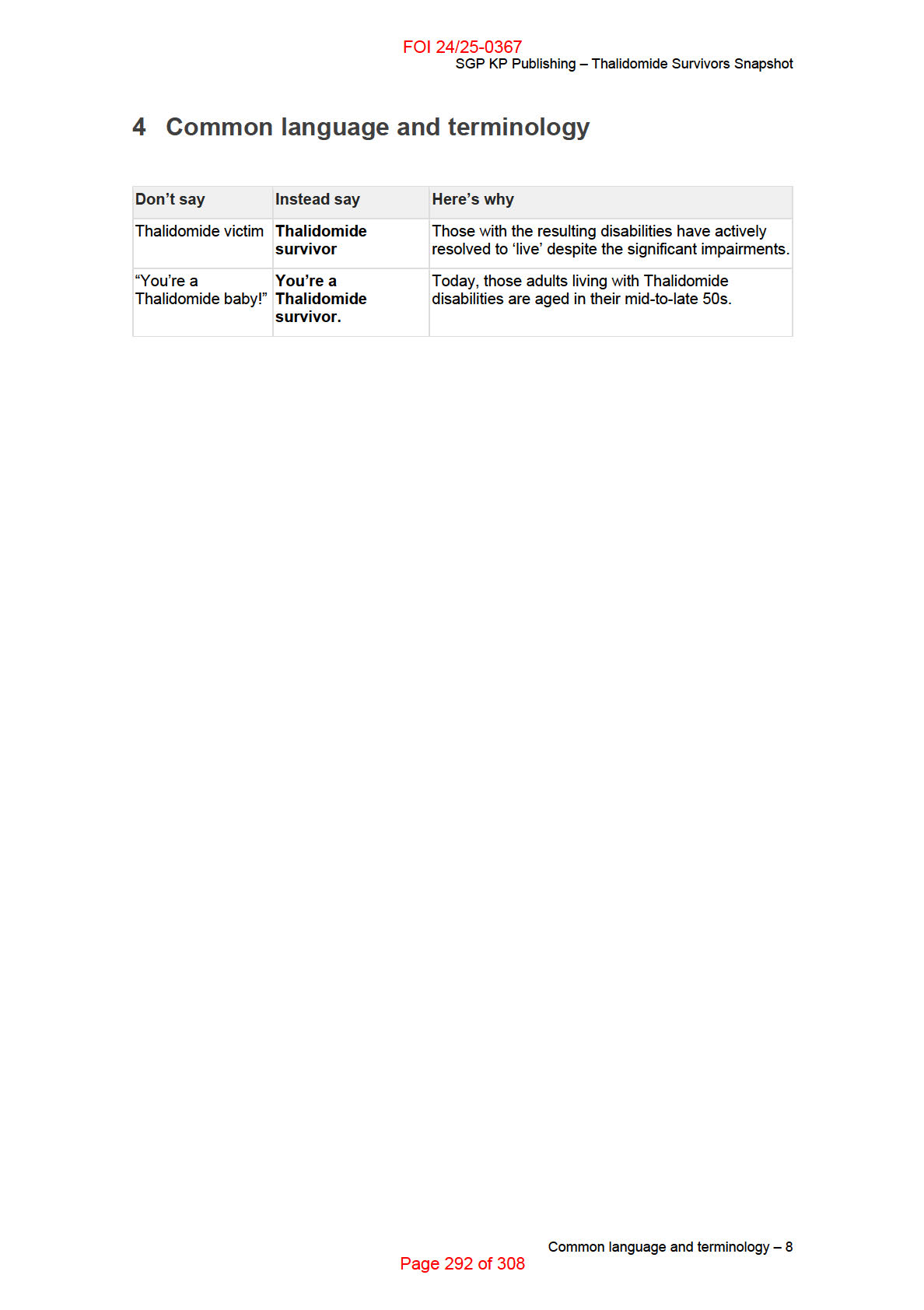
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Thalidomide Survivors Snapshot
5 Engaging with families and carers
The families of Thalidomide Survivors, particularly survivors' parents, spouses and children, live
with the effects of what Thalidomide did to the person they love. Parents of Thalidomide
Survivors experienced trauma, guilt, and life changing carer responsibilities. The spouses and
children of survivors have missed life opportunities and continue to make considerable personal
commitments as they provide care and support to their loved one.
Carers may need support and relief and, in particular, may need to take a break from time-to-
time to sustain their own wellbeing, their relationships with other family members and friends
and their capacity to continue caring.
Taking time off can reduce carers’ stress and give them an opportunity to recharge their
batteries. It can also assist their capacity to continue to provide quality care. It may also assist
participants.
Engaging with families and carers – 9
Page 293 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Thalidomide Survivors Snapshot
6 What specific supports might a Thalidomide
Survivor need?
Each Thalidomide Survivor is different and the reasonable and necessary funding in their plan
wil reflect their functional impairment and the support they need to achieve their goals.
A range of supports might be considered in determining how best to support Thalidomide
Survivors into the future, including:
• Assistive technology
• Home help - assistance with everyday needs, household cleaning and/or yard
maintenance.
• Social interactions
• Home modifications
• Vehicle modifications
• Physiotherapists and/or Occupational Therapists
• Clothing alterations specific to the disability needs
• Transport; or
• Supports that result in a break for carers.
What specific supports might a Thalidomide Survivor need? – 10
Page 294 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Thalidomide Survivors Snapshot
7 How can I tailor a meeting with a Thalidomide
survivor?
Most Australian Thalidomide Survivors have remained active members in their local
communities and many have not sought disability support services or government payments.
Ensure you talk through what mainstream community and government services and programs
might be available – ‘you don’t know what you don’t know!’
Many Thalidomide Survivors wil require a table for writing and a drink at a meeting.
Some Thalidomide Survivors are no longer able to take physical notes during a meeting. Ensure
notes are made available at the conclusion of meetings.
Consider also general preparation, prior to the meeting, during the meeting and at the
conclusion of the meeting.
How can I tailor a meeting with a Thalidomide survivor? – 11
Page 295 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Thalidomide Survivors Snapshot
8 Helpful links for further information
Thalidomide Group Australia
The Thalidomide Trust (UK)
Helpful links for further information – 12
Page 296 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
DOCUMENT 24
Younger Onset Dementia Snapshot
SGP KP Publishing
Exported on 2024-10-18 03:15:03
Page 297 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Younger Onset Dementia Snapshot
Table of Contents
1
Peak body consulted when developing this Snapshot .................................................... 4
2
What is Younger Onset Dementia? .................................................................................... 5
3
How is Younger Onset Dementia diagnosed? .................................................................. 6
4
Addressing challenges to social and economic participation ........................................ 7
5
Engaging with families and carers ..................................................................................... 9
6
Common language and terminology ................................................................................ 10
7
How can I tailor a meeting to suit a participant living with younger onset dementia?
11
8
Helpful links for further information ................................................................................ 12
Table of Contents – 2
Page 298 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Younger Onset Dementia Snapshot
This is a snapshot and is not designed to be a comprehensive guide. It provides general
information about younger onset dementia for NDIA staff and partners and is not intended for
external distribution. Each person with dementia is an individual and will have their own needs,
preferences and experiences that will impact on the planning process and considerations for
social and economic participation.
Peak body consulted when developing this Snapshot – 3
Page 299 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Younger Onset Dementia Snapshot
1 Peak body consulted when developing this
Snapshot
In developing this resource we consulted with Dementia Australia.
Peak body consulted when developing this Snapshot – 4
Page 300 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Younger Onset Dementia Snapshot
2 What is Younger Onset Dementia?
Dementia is a term used to describe a collection of symptoms that are caused by conditions
affecting the brain. It is not one specific condition.
Dementia can affect memory, thinking, behaviour, movement and the ability to perform
everyday tasks, which in turn impact on a person’s social or working life.
Younger Onset Dementia (YOD) refers to any form of dementia that occurs in a person under
the age of 65. Currently there are approximately 27,247[1] people with YOD in Australia. While
dementia is less common in people under 65, it has been diagnosed in people in their 50’s, 40’s
and 30’s. There are also rare occurrences of childhood dementia.
Alzheimer’s disease is the most common type of YOD, however Frontotemporal dementia,
Alcohol-Related dementia and Vascular dementia are also commonly identified causes.
There is also a link between Down syndrome and dementia. Studies show that by the age of 40,
almost 100% of people with Down syndrome who die have the changes in the brain associated
with Alzheimer’s disease.
Dementia is a degenerative neurological condition for which there is currently no cure.
What is Younger Onset Dementia? – 5
Page 301 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Younger Onset Dementia Snapshot
3 How is Younger Onset Dementia diagnosed?
Diagnosing dementia in a younger person can be difficult. When symptoms first appear, GP’s
and families may assume that they are caused by other factors like depression, stress, marriage
breakdown or other physiological conditions and as such, it may take a number of years before
relevant tests are carried out. In some cases it can take many years to get a diagnosis of YOD.
Diagnostic Process
Initial signs and symptoms are generally first reported to a GP who will begin to screen for
relevant medical causes. This initial testing may include a medical/family history, physical
examination, blood tests and neuropsychological or cognitive testing.
The diagnosis of dementia is undertaken by a process of elimination. As other medical causes,
e.g. depression, stroke/brain injury, urinary tract infection, etc. are ruled out, a person is likely to
be referred to a relevant medical specialist for more comprehensive assessment and testing.
This may include brain imaging/scans, extensive neuropsychological or psychiatric assessment
and laboratory testing.
Once this testing is complete, the specialist, usually a neurologist, geriatrician or
neuropsychiatrist, will make a formal diagnosis.
How is Younger Onset Dementia diagnosed? – 6
Page 302 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Younger Onset Dementia Snapshot
4 Addressing challenges to social and economic
participation
People living with dementia may experience difficulties in a range of areas which could have a
significant impact on their social and economic participation. For example:
Remembering, particularly recent events – a person may not remember to take their
medication or attend an important appointment. They may forget who a person is,
including a family member or support person. Assistive technology/memory aides might
support participants to manage their daily routines for example, reminders about
appointments, tasks to be completed.
Making decisions – sometimes even decisions that appear fairly straightforward, such
as what to wear or what to eat may become difficult. Developing routines that minimise
everyday decisions at home and work can relieve stress for people living with dementia.
Expressing their thoughts – a person may lose the ability to communicate their
thoughts and needs to others.
Understanding what others are saying – some people may find it difficult to process
and understand what is being said by others. They may not respond at all, or provide a
response that doesn’t fit the question, e.g. answering ‘yes’ to ‘what would you like to do
today?’.
Finding their way around – a person may become easily disorientated, even in
familiar environments, and find it difficult to navigate to their intended destination e.g.
returning home after going out for a short walk.
Performing more complex tasks – tasks that have multiple steps, such as using a
microwave, can become difficult for people. Similarly, responding to instructions with
multiple steps, such as ‘get ready for a shower’, can also be difficult for people to
process. Visual and audio prompts can be effective in managing complex tasks.
Behavioural changes – a person may experience mood and behaviour changes which
can include, but are not limited to, apathy, aggression, agitation, depression,
disinhibition and hallucinations. Frontotemporal dementia is more common in younger
people, and will often present as changes in ability to regulate emotions, difficulty
responding appropriately in social settings, exhibiting disinhibited behaviour, and
impaired judgement.
Managing finances – a person may have reduced insight into the appropriateness of
their purchases, e.g. buying another loaf of bread before using the one they purchased
yesterday, or have difficulty understanding or performing financial calculations. Or
indeed, understanding the value of money.
Considerations in Education and Employment
People diagnosed with younger onset dementia are often employed at the time of diagnosis.
They may have financial responsibilities such as supporting a family or paying a mortgage.
Deciding whether or not to continue their employment and whether to tell their employer about
their diagnosis is very complex. There are no rules that will work for everyone. Factors that may
affect a person’s decision include:
safety and duty of care
the extent to which the symptoms affect their ability to do the job
Addressing challenges to social and economic participation – 7
Page 303 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Younger Onset Dementia Snapshot
the pace at which the symptoms are progressing
the support that is required (or likely to be offered) by their employer
Employers and work colleagues will require information, education and support to allow for
adaptions in the workplace. This can be delivered through a participant’s plan to maximise
successful social and economic participation.
Job customisation is also an important part of supporting a person to harness their skills while
recognising certain tasks would induce stress or errors. Job customisation is an evidenced
based methodology to ensure that participant’s abilities are matched to the jobs they are asked
to perform.
Many people that decide to leave work still feel fit and capable to participate in community
activities and may wish to consider volunteering roles. Some people may also wish to become a
dementia advocate, to help raise awareness about dementia and share their story with others.
Addressing challenges to social and economic participation – 8
Page 304 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Younger Onset Dementia Snapshot
5 Engaging with families and carers
It is also important to remember that caring for a person living with dementia can be physically
and emotionally tiring and stressful. Families and carers can easily become isolated, particularly
if they are unable to leave the person they are caring for. Supports for the person living with
dementia that provide a ‘break’ for carers, such as respite or regular social support can assist
carers and family members to manage their own health and wellbeing and help them to sustain
their informal supports over a longer period of time.
Engaging with families and carers – 9
Page 305 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Younger Onset Dementia Snapshot
6 Common language and terminology
People with dementia may refer to their condition in different ways. Some terms about dementia
may be upsetting or offensive to people with dementia and their families. It is important to check
with the participant how they prefer to describe their condition. In addition you can confidently
use the following terms;
Dementia, a form or type of dementia, symptoms of dementia, a person/people with dementia, a
person/people living with dementia, a person/people with a diagnosis of dementia, a person with
Younger Onset Dementia.
The term Younger Onset Dementia is seen as preferable to other terminology, including ‘early
onset dementia’ as it specifically refers to any form of dementia where symptoms appear in
people under the age of 65.
Common language and terminology – 10
Page 306 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Younger Onset Dementia Snapshot
7 How can I tailor a meeting to suit a participant living
with younger onset dementia?
It is important to remember that everyone’s experience with dementia is very different,
even if they share the same underlying cause, e.g. Alzheimer’s disease.
Function can fluctuate on a regular basis. Even if a person presents well at their
planning meeting, it may not be representative of their normal day to day function.
People with dementia vary greatly in their level of insight. Some will be aware of their
condition, and will be able to identify their deficits and challenges. Others, and this is
more common, will have very little insight even at a very early stage. For these people,
they will present a false picture of how they are going. It is important to know that this is
not deliberate or contrived, but rather, they truly believe that nothing or little is wrong.
Include the person with dementia in discussions and ensure they feel seen and heard.
A person with dementia may not know what their needs and goals are, or be able to
express them accurately.
Informal supports, such as family and friends, play a critical role in supporting a person
living with dementia. Primary carers and other family members often have a wealth of
information regarding the person’s needs and goals and should be included in the
planning process wherever possible.
Confirm meeting details with the person’s primary carer or support person and confirm
that they can attend the meeting with the participant as required.
Travelling to appointments can be extremely stressful for a person living with dementia.
Home environments for more complex meetings can be beneficial.
How can I tailor a meeting to suit a participant living with younger onset dementia? – 11
Page 307 of 308
FOI 24/25-0367 - DISCLOSURE LOG - DOCUMENTS
SGP KP Publishing – Younger Onset Dementia Snapshot
8 Helpful links for further information
About Dementia
https://www.dementia.org.au/about-dementia/what-is-dementia
Types of Dementia
https://www.dementia.org.au/information/about-dementia/types-of-dementia
Dementia and Down Syndrome
https://www.dementia.org.au/about-dementia/types-of-dementia/down-syndrome-and-
alzheimers-disease
Diagnosing Dementia
https://www.dementia.org.au/information/diagnosing-dementia
Dementia Friendly Language
https://www.dementia.org.au/resources/dementia-language-guidelines
YOD and the NDIS
https://www.dementia.org.au/resources/younger-onset-dementia-and-the-ndis
Employment and Dementia
https://www.dementia.org.au/about-dementia/i-have-dementia/employment-and-dementia
Dementia Advocates Program
https://www.dementia.org.au/about-us/dementia-advocates-program
[1] Dementia Australia (2018) Dementia Prevalence Data 2018-2058, commissioned research
undertaken by NATSEM, University of Canberra
Helpful links for further information – 12
Page 308 of 308