FOI 24/25-0514
DOCUMENT 1
Research paper
OFFICIAL
For Internal Use Only
Applied behaviour analysis and positive
behaviour support
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be
shared external to the Branch. These are for internal TAB use only and are intended to
assist our advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If
Delegates require further information on access or planning matters, they are to call the
TAPS line for advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: What is the difference between Applied Behaviour Analysis and positive
behaviour support? Is intensive ABA effective for managing behaviours of concern? What
qualifications and legislative requirements are required for a practitioner to develop or
implement a positive behaviour support programme?
Date: 21/07/2022
Requestor: Kim s22(1)(a)(ii)
- irr
Endorsed by (EL1 or above): Naomi s22(1)(a)(ii)
- irrelevan
Researcher: Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Shane s22(1)(a)(ii) - irre
1. Contents
Applied behaviour analysis and positive behaviour support ....................................................... 1
1.
Contents ....................................................................................................................... 1
2.
Summary ...................................................................................................................... 2
3.
Applied behaviour analysis ........................................................................................... 2
4.
Positive behaviour support ............................................................................................ 3
5.
Intensive Applied Behaviour Analysis and behaviours of concern ................................ 4
6.
Practitioner qualifications and registration requirements ............................................... 5
6.1 Board Certified Behaviour Analysts ........................................................................... 5
V1.0 25-07-2022
ABA and PBS
Page 1 of 9
OFFICIAL
Page 1 of 16

FOI 24/25-0514
Research paper
OFFICIAL
For Internal Use Only
6.2 Behaviour support and the NDIS ............................................................................... 7
7.
References ................................................................................................................... 8
8.
Version control .............................................................................................................. 9
2. Summary
There is ambiguity in the way Applied Behaviour Analysis (ABA) and Positive Behaviour
Support (PBS) are used to describe interventions or disciplines. ABA as a label can be used in
wider or more narrow ways and depending on how the term is used it might encompass PBS
as well. In the sense employed in much NDIS documentation, PBS is theoretically informed by
ABA as an applied research program, while being distinguished from ABA as a specific
intervention or therapy programme.
There is moderate level evidence that intensive ABA programs reduce behaviours of concern.
However, no information on dosage was found.
While there are some intensive ABA programmes that can only be run by Board Certified
Behaviour Analysts, some ABA-informed programs can be run by qualified health
professionals (e.g Occupational Therapists, Speech Therapists) for which the programme is
within their scope of practice. Positive behaviour support practitioners require specific
registration through the NDIS Quality and Safeguards Commission in order to provide
behavioural assessments and behaviour support plans for NDIS participants. However, I
cannot find any evidence that “behaviour support practitioner” or “positive behaviour support
practitioner” are regulated terms outside of their use in the context of NDIS registered
providers.
3. Applied behaviour analysis
The definition of ABA used in the NDIA commissioned AutismCRC report
Interventions for
children on the autism spectrum: A synthesis of research evidence is:
the scientific application of behavioural principles to, first, identify variables that are
responsible for behavioural change, and second, to use these variables to improve
socially significant behaviours (Whitehouse et al., 2020, p.31).
This definition is derived from Cooper et al (2020), who say:
Applied behaviour analysis is the science in which tactics derived from the principles of
behaviour are applied systematically to improve socially significant behaviour and
experimentation is used to identify the variables responsivle for behaviour change
(Cooper et al., 2020, p.19).
As both these definitions show, the practice of ABA is intended to improve socially significant
behaviours. This is a very broad category of behaviours that can include:
V1.0 25-07-2022
ABA and PBS
Page 2 of 9
OFFICIAL
Page 2 of 16

FOI 24/25-0514
Research paper
OFFICIAL
For Internal Use Only
social, language, academic, daily living, self-care, vocational, and/or recreation and
leisure behaviours that improve the day-to-day life experience of the participants and/or
affect their significant others (parents, teachers, peers, employers) in such a way that
they behave more positively with and toward the participant (Cooper et al., 2020, p.16).
For reasons of terminological clarity, we should also note that ABA is used by Cooper et al to
refer to an applied research program. Cooper et al (2020) distinguish between ABA as a
research discipline on the one hand, and on the other, professional practice in which insights
from ABA are integrated into frontline services for use by participants, family, teachers or
trained therapists. Whitehouse et al. (2020) use ABA to refer to both the applied research
program and its application by Board Certified Behaviour Analysts. They distinguish ABA as
applied by Board Certified Behaviour Analysts from derivative forms of behavioural
intervention which might depend on ABA principles but diverge in some way. They cite, for
example, Naturalistic Development Behavioural Interventions, Picture Exchange
Communication System, Early Start Denver Model and Positive Behaviour Support. Rogers et
al list interventions they consider a kind of intensive ABA-type therapy, including Murdoch
Early Intervention Program, Early intensive behavioural intervention, Early start denver model,
Comprehensive intensive early intervention and Intensive behaviour analytic treatment
(Rogers et al, 2020).
4. Positive behaviour support
The NDIS Quality and Safeguard Commission Positive Behaviour Support Capability
Framework defines PBS as:
the integration of the contemporary ideology of disability service provision with the
clinical framework of applied behaviour analysis. Positive behaviour supports are
supported by evidence encompassing strategies and methods that aim to increase the
person’s quality of life and reduce challenging behaviour (NDIS Quality and Safeguards
Commission, 2019, p.5).
The idea that PBS is ABA plus “the contemporary ideology of disability” refers to Carr et al.’s
suggestion that PBS emerged from three sources including ABA, the normalisation/inclusion
movement and person-centred values (Carr et al, 2002). There is some question about
whether PBS is a kind of ABA, or just informed or otherwise related to it (Whitehouse et al,
2020). It is also not clear what the practical implications of this question are.
Like ABA, PBS focusses on socially significant behaviours though its target behaviours are
restricted to challenging or problematic behaviours. There is no agreed terminology used to
describe challenging or problematic behaviours. Synonyms used include: behaviours of
concern, challenging behaviour, behaviour that challenges, maladaptive behaviour, interfering
behaviour, disruptive behaviour, problem behaviour and problematic behaviour (Whitehouse et
al, 2020; Rogers et al, 2020).
UK’s National Autism Centre defines problem behaviours as behaviour that:
V1.0 25-07-2022
ABA and PBS
Page 3 of 9
OFFICIAL
Page 3 of 16

FOI 24/25-0514
Research paper
OFFICIAL
For Internal Use Only
can harm the individual or others OR result in damage to objects OR interfere with the
expected routines in the community. Problem behaviors may include but are not
restricted to self-injury, aggression, disruption, destruction of property, or hazardous or
sexually inappropriate behaviors (National Autism Centre, 2015, p.39).
UK’s National Institute of Healthcare Excellence also considers stereotypic behaviour and
withdrawal to be challenging behaviours (NICE, 2015). Whitehouse et al. use the definition:
Challenging behavior refers to certain behaviors that a person engages in which
negatively affect his/her daily functioning. These behaviors are often recognized as
being culturally abnormal and occur at such an intensity, frequency, or duration that the
safety of the person and/or others is placed in jeopardy. Challenging behaviors may be
related to social, academic, communicative, cognitive, vocational, or physical domains,
may serve various functions, and should be examined systematically in order to identify
these functions (Whitehouse et al, 2020, pp.122-123).
While PBS targets specific behaviours, strategies to address those behaviours take account of
“a person’s needs, their home environment and overall quality of life through assessment,
planning and intervention” (Practice Guidance – Behaviour Support and Behaviours of
Concern). This relates to another core feature of PBS cited by the NDIS commission: PBS
aims to reduce and eliminate restrictive practice (NDIS Quality and Safeguards Commission,
2022, Glossary).
5. Intensive Applied Behaviour Analysis and behaviours
of concern
Whitehouse et al. (2020) summarise evidence from systematic reviews which track the effect
of behavioural techniques on challenging behaviours. In three systematic reviews including a
variety of behavioural interventions, they note a moderate level of evidence indicating a
positive effect on challenging behaviours. Regarding specific interventions, they note that there
is low level evidence that Functional Communication Training and Discrete Trial training have
a positive effect on challenging behaviours and moderate level of evidence that Early intensive
behavioural intervention has a null effect on challenging behaviours.
The UK’s National Autism Centre report (2015) notes that behavioural interventions can
reduce problem behaviours for people aged 3 – 22 years old. More specifically, ABA type
programs delivered 25-40 hours per week for 2-3 years are shown to reduce problem
behaviours for children aged 0 – 9. More recently, a team from the US-based National
Clearinghouse on Autism Evidence and Practice found Functional Communication Training –
an off-shoot of ABA – has a positive effect on reducing behaviours of concern for children 3 –
18 years. They also found Discrete Trial Training – another ABA off-shoot – can be effective at
reducing behaviours of concern in children aged 6 – 11 years (Steinbrenner et al, 2020).
V1.0 25-07-2022
ABA and PBS
Page 4 of 9
OFFICIAL
Page 4 of 16

FOI 24/25-0514
Research paper
OFFICIAL
For Internal Use Only
However, due to the layout of both the National Autism Centre report and the Clearinghouse
on Autism Evidence and Practice report, it is not clear from which studies they derived the
confident assessment that ABA-type therapies can reduce problem behaviours. This is
important as other reviews make more tentative claims. Rogers et al (2020) reviewed 20
intensive ABA studies and found one noting reduction in behaviours of concern but results
were not statistically significant. In their systematic review, Reichow et al (2018) considered 2
studies which tracked problem behaviours. They found very low-quality evidence that EBEI did
not have a statistically significant difference effect at reducing behaviours of concern
compared to therapy as usual control. However, given the growth of autism research in the last
5 years, currency is a problem for this review (Whitehouse et al, 2020).
This brief summary does show some evidence for effectiveness of ABA-type therapies in
reducing behaviours of concern. There are some inconsistencies in results and the research
could be of higher quality. It is also worth noting that none of the reviews spoke to the dosage
required to effect a reduction in behaviours of concern. While 25-40 hours per week is noted
as the dosage in the National Autism Centre report, it is not clear from the evidence reviewed
that this level of therapy is required to achieve the outcomes stated or that other therapies
derived from ABA have this level of implementation.
Also of note, there is evidence that other types of therapies are also effective at reducing
behaviours of concern. For example, of 28 evidence-based practices that Steinbrenner et al
consider, only 2 did not show some effect at reducing behaviours of concern for some age
group of children or young adults.
Reichow et al conclude their review by saying:
Given the lack of high-quality, generalizable evidence to determine the effects of Early
Intensive Behavioural Intervention (EIBI) for ASD, it is important that decisions about its
use are made on a case-by-case basis. It is also important that providers of EIBI are
aware of the limited quality of the current evidence and use clinical decision-making
guidelines, such as seeking the family’s input and drawing upon prior clinical
experience, when making recommendations to clients on the use of EIBI (Reichow et al,
2018, p.17).
6. Practitioner qualifications and registration
requirements
6.1 Board Certified Behaviour Analysts
ABA practitioners should be qualified, regulated and deliver services that are within the scope
of their clinical practice. Unlike other allied health professionals in Australia, ABA practitioners
are currently accredited internationally by the Behavior Analyst Certification Board (BACB)
based in USA (Whitehouse et al, 2020; Association for Behaviour Analysis Australia, n.d).
BACB provide certification for:
V1.0 25-07-2022
ABA and PBS
Page 5 of 9
OFFICIAL
Page 5 of 16

FOI 24/25-0514
Research paper
OFFICIAL
For Internal Use Only
• Registered Behavior Technician (RBT) – works under supervision of BCaBA and
BACB
• Board Certified Assistant Behavior Analyst (BCaBA) – works under supervision of
BACB
• Board Certified Behavior Analyst (BCBA) – works independently and can supervise
RBT and BCaBA (Behaviour Analysis Certification Board, n.d, Board Certified
Behavior Analyst).
To gain and maintain accreditation as a BACB, a practitioner needs to:
• complete a recognised course or equivalent professional experience
• pass an exam
• meet continuing education requirements
• adhere to ethics requirements
• recertify every 2 years (Behaviour Analysis Certification Board, n.d, Credentials).
Association for Behaviour Analysis Australia has expressed their intention to take up regulation
and accreditation of ABA practitioners in Australia:
As of December 2019 the BACB announced that it wil limit certification to a select
number of countries. Currently, Australia is one of the countries where BACB
certification is stil available but the longevity of this option is unknown. This has
highlighted the need for Australia to have its own regulatory body for behaviour analysts.
ABA Australia saw the need of our field and felt that it was inline with our mission and
objectives to take on this challenge and continue our efforts to disseminate safe and
ethical practice of ABA (Association for Behaviour Analysis Australia, n.d, Professional
Self-Regulation).
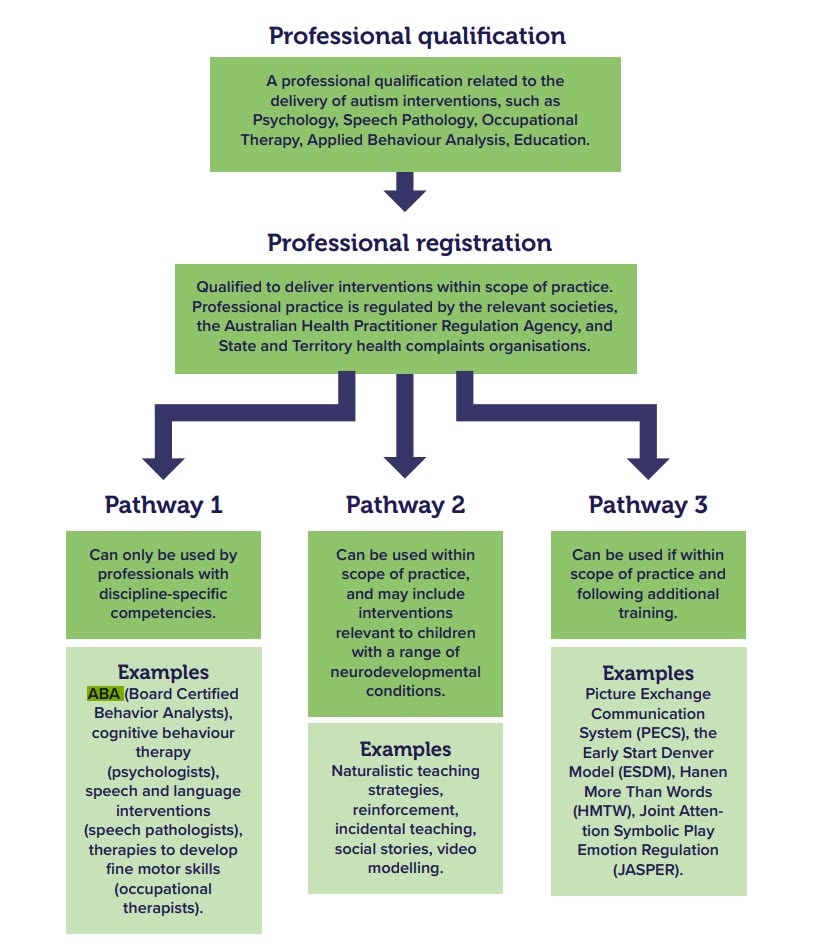
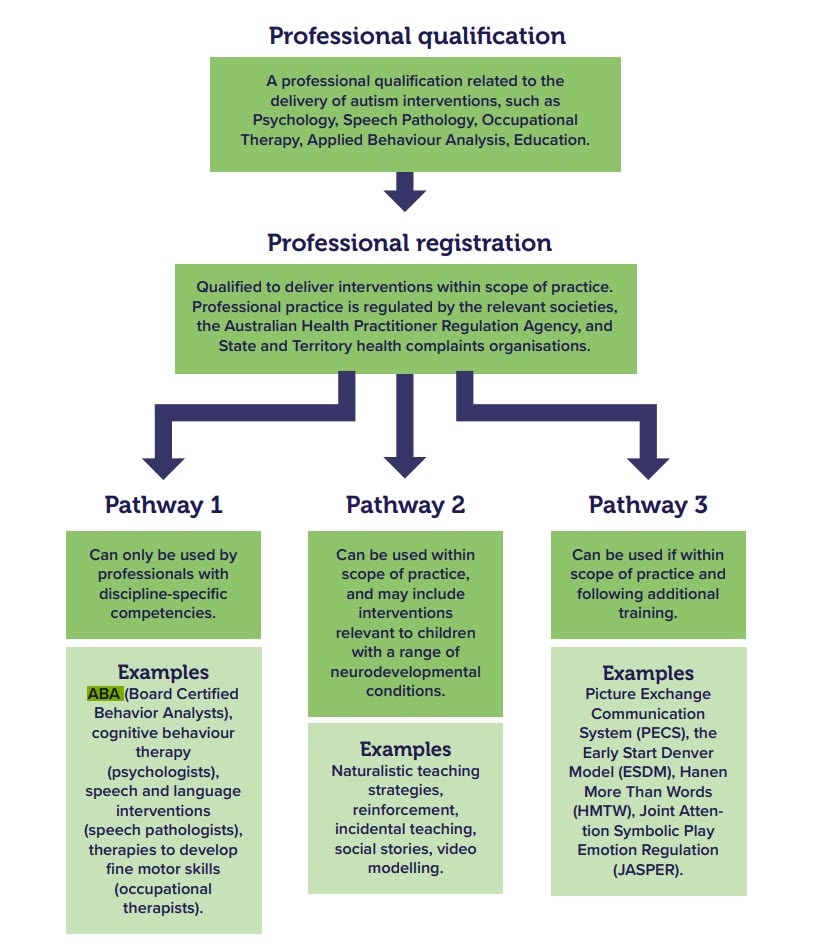
Not all interventions which incorporate the principles or strategies of ABA are restricted to
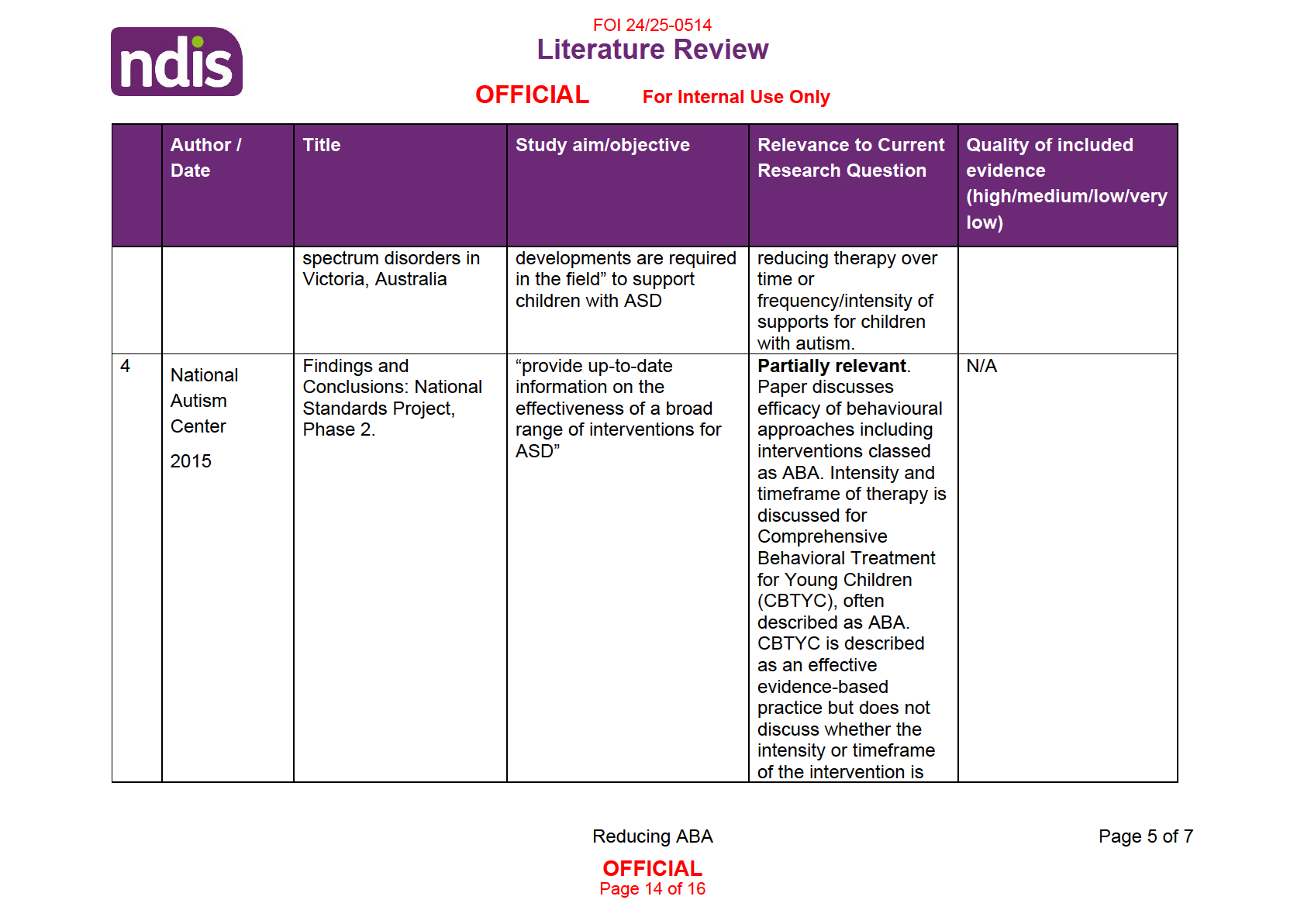
certified BCBAs. The figure below from Whitehouse et al (2020, p.47) describes different
pathways by which ABA-type or associated interventions can be practiced.
V1.0 25-07-2022
ABA and PBS
Page 6 of 9
OFFICIAL
Page 6 of 16

FOI 24/25-0514
Research paper
OFFICIAL
For Internal Use Only
6.2 Behaviour support and the NDIS
Specialist behaviour support is provided through a participant’s NDIS plan through the
Improved Relationships budget using line items:
• Specialist Behavioural Intervention Support
• Behaviour Management Plan Including Training in Behaviour Management
Strategies
A registered specialist behaviour support practitioner must develop all functional behaviour
assessments and Behaviour Support Plans, as positive behaviour support practice requires a
specific skil set and appropriate safeguards (Practice Guidance – Behaviour Support and
Behaviours of Concern). An NDIS behaviour support practitioner must be deemed suitable by
the NDIS Quality and Safeguard Commission (NDIS Restrictive Practices and Behaviour
Support Rules 2018, s17). To be deemed suitable the practitioner must be qualified,
experienced and must have considered their professional development alongside the Positive
Behaviour Support Capability Framework (NDIS Quality and Safeguards Commission, 2022,
Fact sheet: New behaviour support practitioners).
V1.0 25-07-2022
ABA and PBS
Page 7 of 9
OFFICIAL
Page 7 of 16

FOI 24/25-0514
Research paper
OFFICIAL
For Internal Use Only
The above is required for a practitioner to provide positive behaviour support to NDIS
participants. There may be qualified and practicing behaviour support practitioners who are not
NDIS behaviour support practitioners. I cannot find any evidence that “behaviour support
practitioner” or “positive behaviour support practitioner” are regulated terms outside of their
use in the context of NDIS registered providers.
7. References
Association for Behaviour Analysis Australia. (n.d). https://auaba.com.au/
Behavior Analysis Certification Board. (n.d). https://www.bacb.com/bcba/
Carr EG, Dunlap G, Horner RH, et al. (2002). Positive Behavior Support: Evolution of an
Applied Science.
Journal of Positive Behavior Interventions,
4(1):4-16.
doi:10.1177/109830070200400102
Cooper, J. O., Heron, T. E., & Heward, W. L. (2020). Applied Behaviour Analysis (Vol. 3rd Ed).
United Kingdom: Pearson
National Autism Center. (2015). Findings and conclusions: National standards project, phase
2. https://www.nationalautismcenter.org/national-standards-project/phase-2/
National Institute for Health and Care Excellence (NICE). (2015). Challenging behaviour and
learning disabilities: Prevention and interventions for people with learning disabilities
whose behaviour challenges. Retrieved from https://www.nice.org.uk/guidance/ng11
NDIS Quality and Safeguards Commission (2019). Positive behaviour support capability
framework: For NDIS providers and behaviour support practitioners. Penrith, Australia:
NDIS Quality and Safeguards Commission. Available:
https://www.ndiscommission.gov.au/pbscapabilityframework
NDIS Quality and Safeguards Commission. (2022). Fact sheet: New entry level behaviour
support practitioners applying for suitability.
https://www.ndiscommission.gov.au/sites/default/files/2022-07/New entry level
behaviour support practitioners suitability.pdf
Reichow, B., Hume, K., Barton, E. E., & Boyd, B. A. (2018). Early intensive behavioral
intervention (EIBI) for young children with autism spectrum disorders (ASD).
Cochrane
Database of Systematic Reviews (5). doi:10.1002/14651858.CD009260.pub3
Rodgers M, Marshall D, Simmonds M, Le Couteur A, Biswas M, Wright K, et al. (2020)
Interventions based on early intensive applied behaviour analysis for autistic children: a
systematic review and cost-effectiveness analysis.
Health Technol Assess, 24(35).
Steinbrenner, J. R., Hume, K., Odom, S. L., Morin, K. L., Nowel , S. W., Tomaszewski, B.,
Szendrey, S., McIntyre, N. S., Yücesoy-Özkan, S., & Savage, M. N. (2020). Evidence-
based practices for children, youth, and young adults with Autism. The University of
V1.0 25-07-2022
ABA and PBS
Page 8 of 9
OFFICIAL
Page 8 of 16

FOI 24/25-0514
DOCUMENT 2
Literature Review
OFFICIAL
For Internal Use Only
Reducing Applied Behaviour Analysis over time
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: Is there substantial evidence that a step-down transition away from
Applied Behaviour Analysis (ABA) therapy can provide outcomes and be of benefit?
Date: 3/1/24
Requestor: Star s22(1)(a)(ii) -
Endorsed by: Naomi s22(1)(a)(ii) - irreleva
Researcher: Stephanie s22(1)(a)(ii)
,
- irrelevant mate Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Stephanie s22(1)(a)(ii) - irrelevant mat
1. Contents
Reducing Applied Behaviour Analysis over time ........................................................................ 1
1.
Contents ....................................................................................................................... 1
2.
Summary ...................................................................................................................... 2
3.
Previous TAPIB research papers .................................................................................. 2
4.
Review of Provided Literature ....................................................................................... 2
5.
Other sources ............................................................................................................... 2
6.
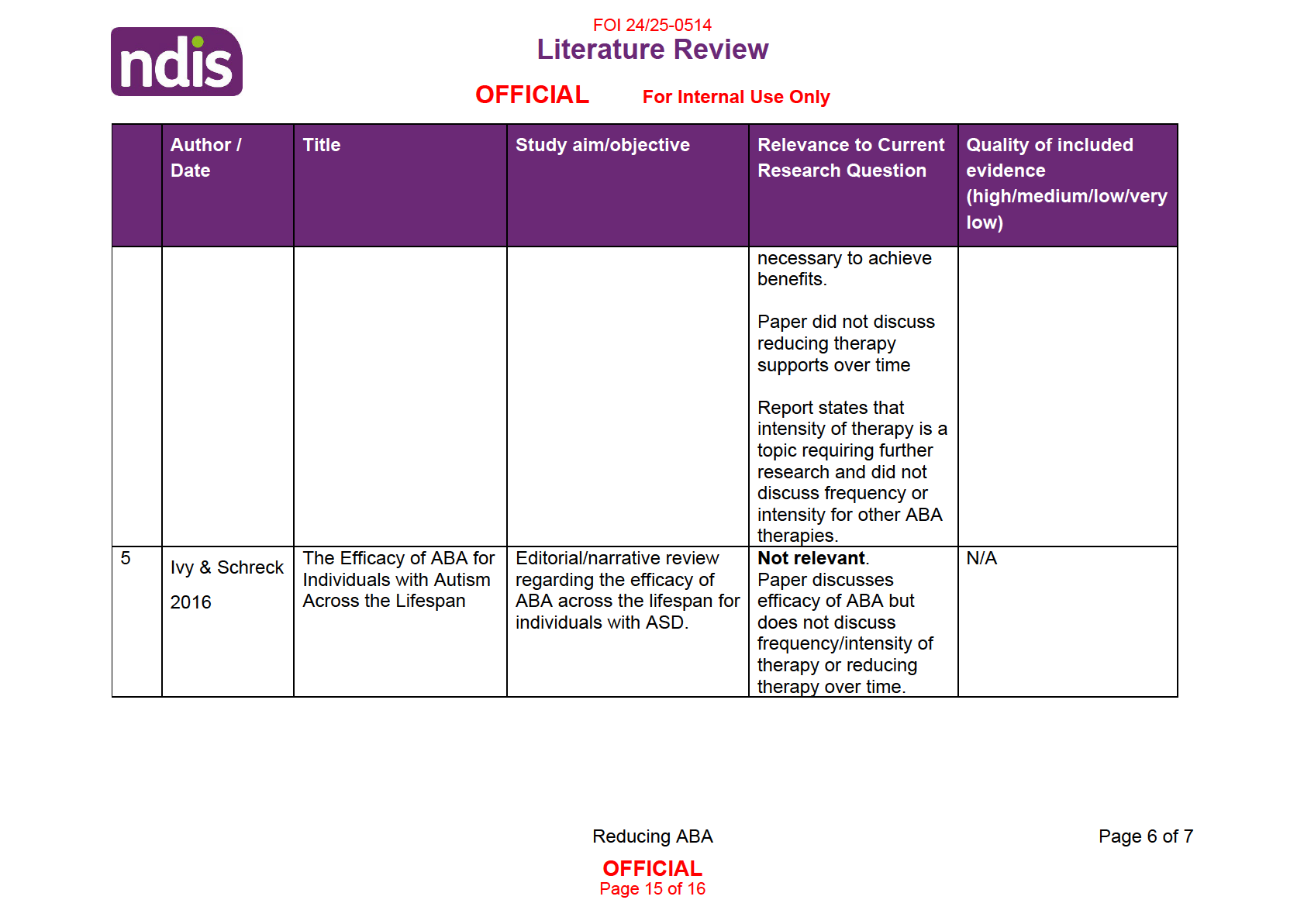
Literature review table ................................................................................................... 4
7.
References ................................................................................................................... 7
Reducing ABA
Page 1 of 7
OFFICIAL
Page 10 of 16

FOI 24/25-0514
Literature Review
OFFICIAL
For Internal Use Only
2. Summary
This paper considers the evidence for a step-down model of reducing frequency or intensity of
applied behaviour analysis (ABA). No evidence was found regarding the effectiveness of a
step-down model. One international ABA accreditation body, the Behavioral Health Center of
Excellence, recommends a gradual reduction in hours when concluding ABA therapy.
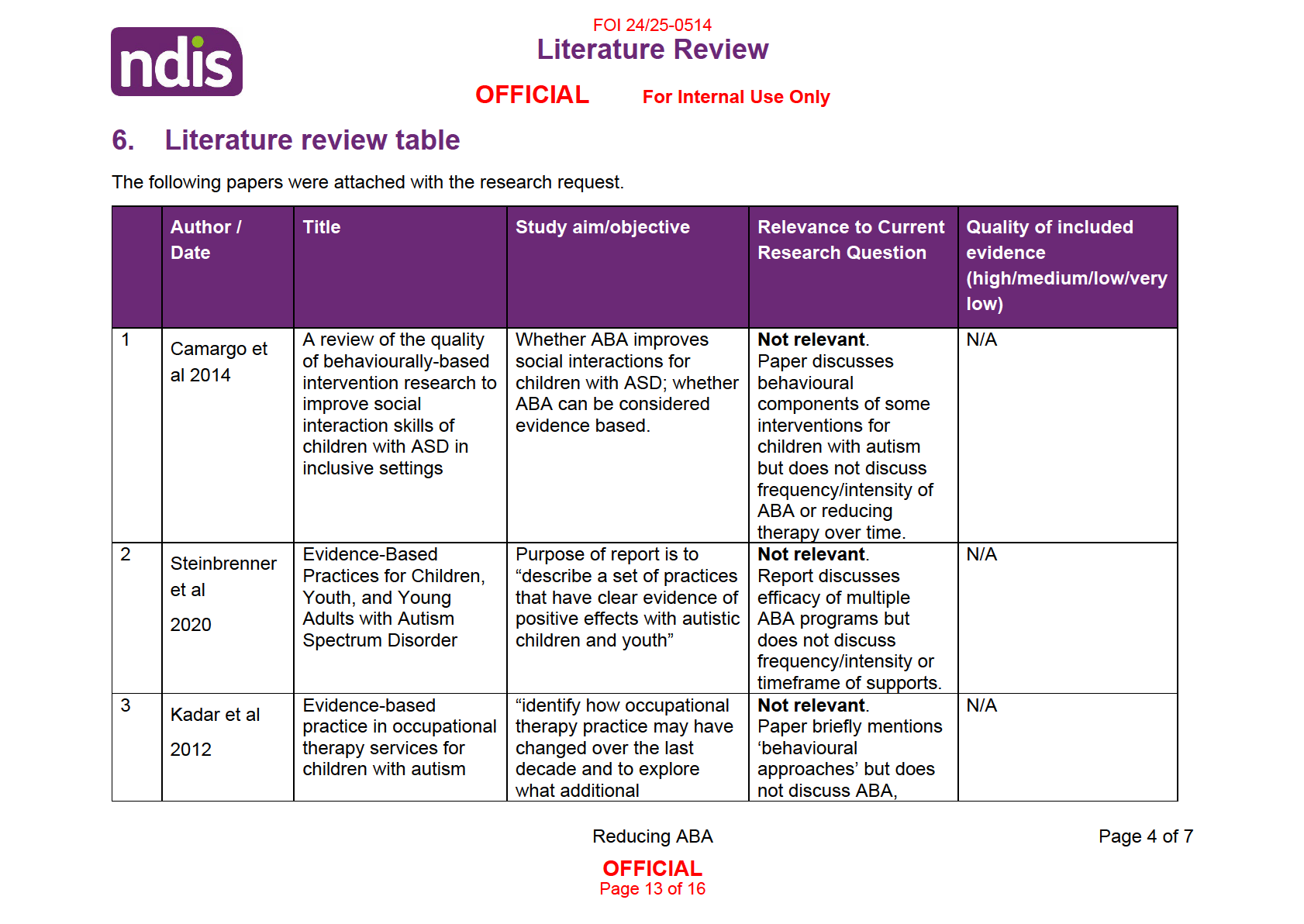
Five papers were attached with the research request. None of the papers directly relate to the
efficacy of a step-down model of reducing ABA supports.
Previous TAPIB research has found a lack of consensus regarding appropriate intensity and
duration of ABA therapy. Recent Australian guidelines on the delivery of supports for children
with autism note that supports should be individualised and there is no set number of hours of
therapy which are appropriate for every child.
3. Previous TAPIB research papers
Previous TAPIB research papers related to ABA include:
• RES 246 ABA and positive behaviour support.docx
• RES 292 Applied behaviour analysis for adults with ASD.docx
RES 246 found no evidence for appropriate frequency, intensity or timeframe of ABA required
to affect a reduction in behaviours of concern, nor any information on reducing intensity of
support over time.
RES 292 found lack of consensus regarding appropriate frequency, intensity or timeframe of
ABA. The studies review in this paper emphasised that an individualised approach to
determining frequency, intensity and timeframe of supports is required.
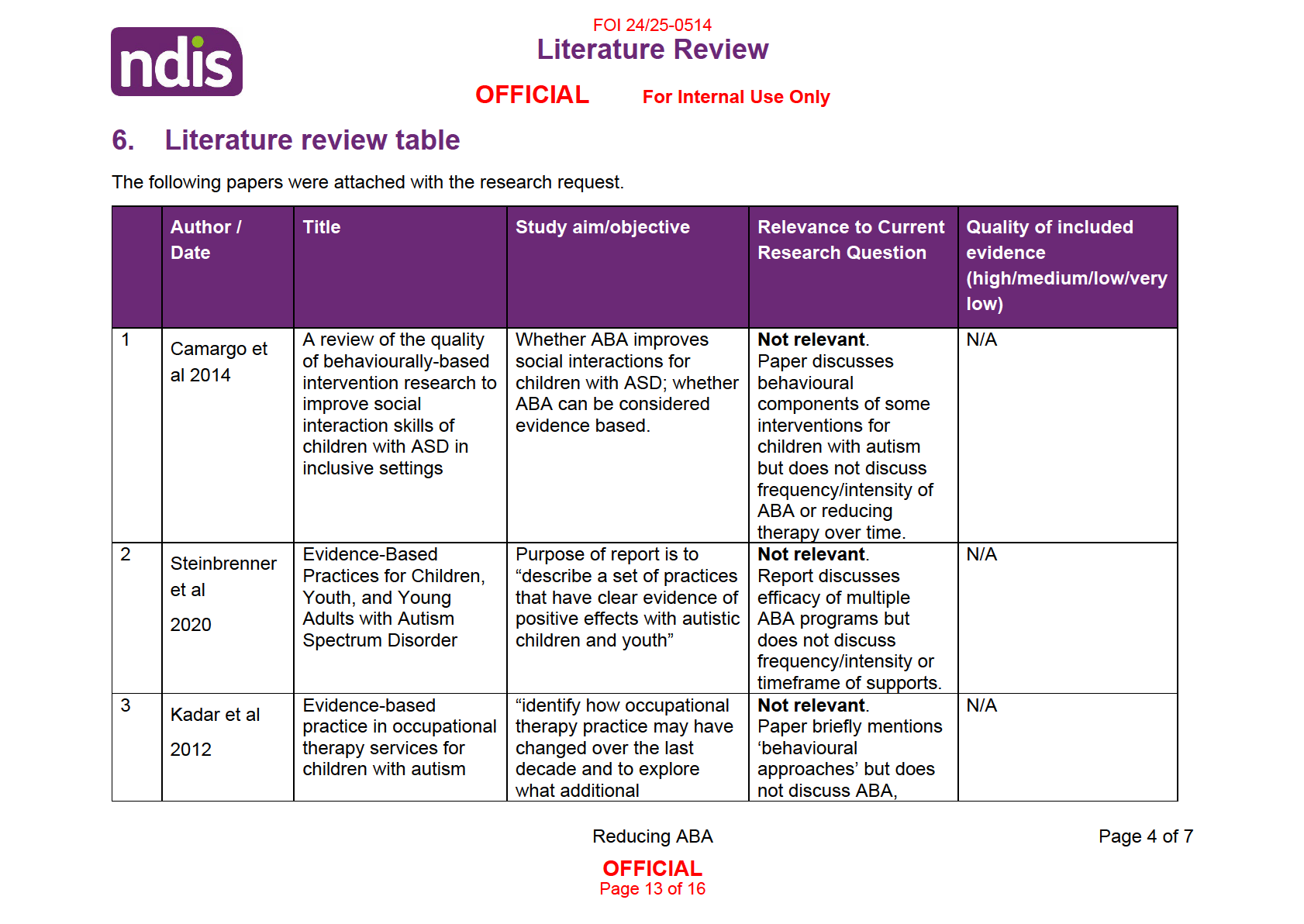
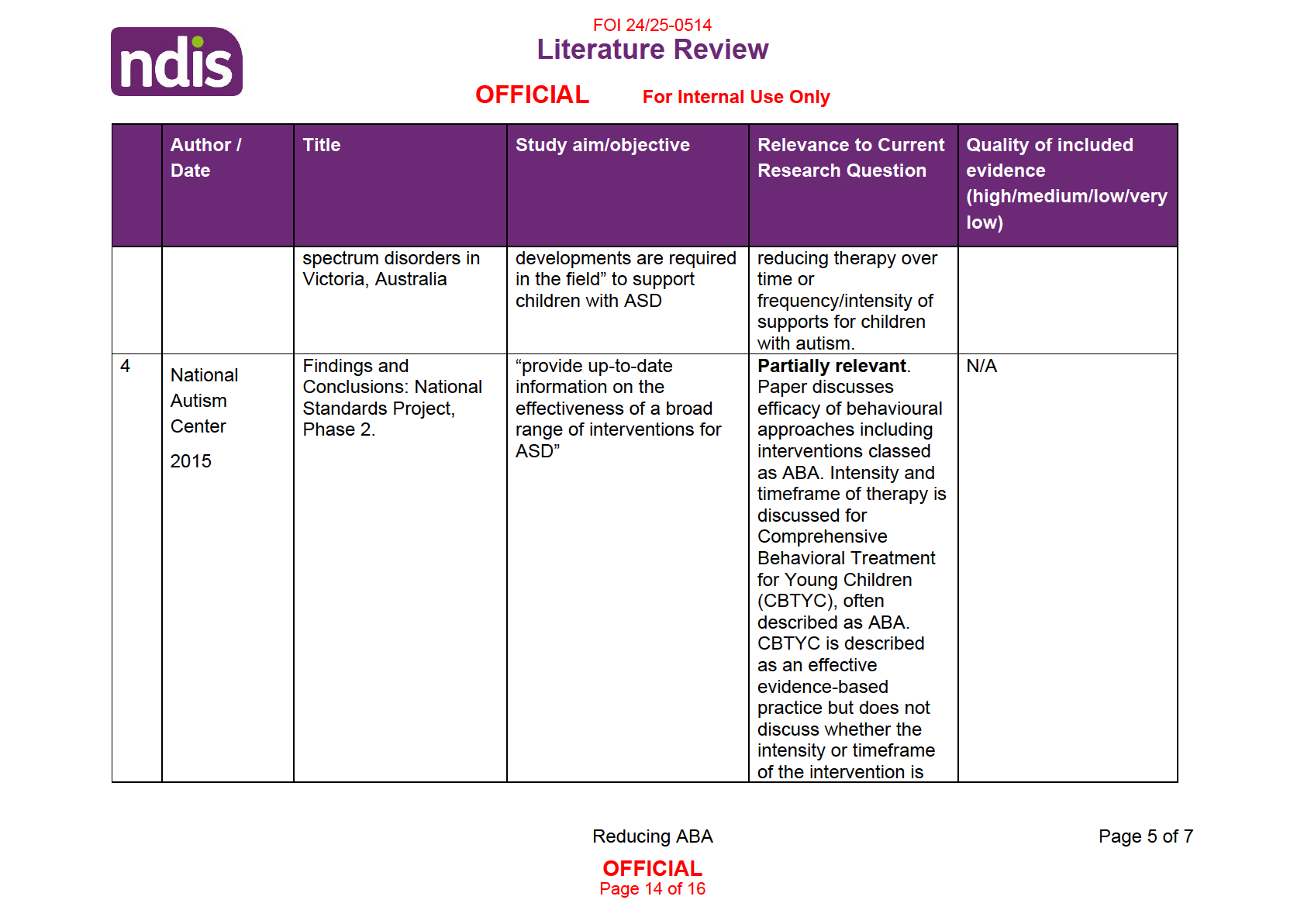
4. Review of Provided Literature
Five papers were attached with the research request (refer to 6. Literature Review table for
further details). None of the attached papers were directly relevant to the research question.
None of the papers reviewed directly addressed the benefits of an extended timeframe of
supports or the benefits of slowly reducing ABA support over time. No quality assessment was
completed due to lack of relevance to the research question.
5. Other sources
The Behavioral Health Center of Excellence (BHCE) is a private organisation that offers
accreditation of applied behaviour analysts. They suggest fading out services gradually based
on the needs of the client (BHCE, n.d.). However, BHCE provide no evidence on which they
base this recommendation.
Reducing ABA
Page 2 of 7
OFFICIAL
Page 11 of 16

FOI 24/25-0514
Literature Review
OFFICIAL
For Internal Use Only
Autism CRC’s recent
National Guideline for supporting the learning, participation, and
wellbeing of autistic children and their families in Australia (Trembath et al, 2022), makes the
following recommendations around duration of supports:
56 . 1 The amount and duration of support provision should be tailored to the individual
needs of the child and family. This includes consideration of the frequency, length, and
time of day of support sessions, and variations in support needs over time.
56.3 Practitioners should inform parents that there is no set number of hours per week
of practitioner delivered child-directed supports that leads to the best outcomes for all
children.
56 . 4 Practitioners should be aware that research evidence does not support the
concept that supports delivered in greater amounts consistently lead to better child and
family outcomes (Trembath et al, 2022, pp.95-96).
The
National Guideline does not discuss reducing therapy over time.
Reducing ABA
Page 3 of 7
OFFICIAL
Page 12 of 16

FOI 24/25-0514
Literature Review
OFFICIAL
For Internal Use Only
7. References
Behavioral Health Center of Excellence. (n.d.).
Suggestions for Ethically Fading Out ABA
Services. https://www.bhcoe.org/2016/11/suggestions-ethically-fading-aba-services/
Camargo, S. P., Rispoli, M., Ganz, J., Hong, E. R., Davis, H., & Mason, R. (2014). A review of
the quality of behaviorally-based intervention research to improve social interaction
skills of children with ASD in inclusive settings.
Journal of autism and developmental
disorders,
44(9), 2096–2116. https://doi.org/10.1007/s10803-014-2060-7
Ivy, J.W. & Schreck, K.A. (2016). The Efficacy of ABA for Individuals with Autism Across the
Lifespan.
Current Developmental Disorder Reports, 3, 57–66.
https://doi.org/10.1007/s40474-016-0070-1
Kadar, M., McDonald, R., & Lentin, P. (2012). Evidence-based practice in occupational therapy
services for children with autism spectrum disorders in Victoria, Australia.
Australian
occupational therapy journal,
59(4), 284–293. https://doi.org/10.1111/j.1440-
1630.2012.01015.x
National Autism Center. (2015).
Findings and conclusions: National standards project, phase
2. https://www.nationalautismcenter.org/national-standards-project/phase-2/
Steinbrenner, J. R., Hume, K., Odom, S. L., Morin, K. L., Nowel , S. W., Tomaszewski, B.,
Szendrey, S., McIntyre, N. S., Yücesoy-Özkan, S., & Savage, M. N. (2020).
Evidence-
based practices for children, youth, and young adults with Autism. The University of
North Carolina at Chapel Hil , Frank Porter Graham Child Development Institute,
National Clearinghouse on Autism Evidence and Practice Review Team.
V0.0 XX-XX-XXXX
Abbreviated Title
Page 7 of 7
OFFICIAL
Page 16 of 16