FOI 23/24- 1400
DOCUMENT 10
Sensory-based therapy
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: Is sensory integration, modulation, processing all talking about the
same thing? Any other important terms to define?
Who might benefit from sensory support?
What is the evidence sensory support reduces the need for RRP?
What is the evidence for other more general outcomes?
Who might implement/qualifications for sensory support?
Date: 29/09/2022
Requestor: Karyn Mueller
Endorsed by: Researcher: Stephanie Pritchard and Aaron Harrison
Cleared by: Stephanie Pritchard
Review date:
Page 103 of 125
link to page 1 link to page 1 link to page 2 link to page 3 link to page 3 link to page 4 link to page 7 link to page 7 link to page 9 link to page 10 link to page 10
FOI 23/24- 1400
1. Contents
Sensory based interventions ...................................................................................................... 1
1.
Contents ....................................................................................................................... 2
2.
Summary ...................................................................................................................... 2
3.
Terminology .................................................................................................................. 3
3.1 Theoretical terminology ............................................................................................. 3
3.2 Types of sensory based interventions ....................................................................... 4
4.
Efficacy ......................................................................................................................... 7
4.1 Autism Spectrum Disorder ......................................................................................... 7
4.2 Mental Health ............................................................................................................ 9
4.3 Other conditions ...................................................................................................... 10
5.
References ................................................................................................................. 10
2. Summary
The terminology used in the literature on sensory disorder and sensory-based interventions
(SBIs) is inconsistent. The terms sensory integration, sensory processing and sensory
modulation are sometimes used interchangeably in the literature and sometimes given distinct
definitions. General features of these key terms can be described.
Researchers and clinicians have employed SBIs for a variety of conditions. Most of the
research available relates to interventions for Autism Spectrum Disorder (ASD) or other
neurodevelopmental disorders such as intellectual disabilities or attention deficit/hyperactivity
disorder, schizophrenia or other mental health conditions such a bipolar, depression or
obsessive-compulsive disorder. There is also research relating to interventions for cerebral
palsy, Huntington’s disease and dementia.
There is some evidence that SBIs can contribute to a reduction in restrictive practice. The
evidence is predominantly in the domain of mental health and is predominantly related to
restrictive practice in a clinical or institutional setting. However, systematic reviews show
inconsistent results. Based on the evidence collected it is not possible to say with confidence
that SBIs reduce the use of restrictive practice. There are many factors which contribute to an
institution’s use of restrictive practice that are not addressed by the introduction of SBIs.
SBIs do likely have some positive effects. There is consistent evidence that SBIs reduce
distress of people with mental health conditions and lower quality evidence that distress is
reduced for people with Huntington’s disease and dementia. There is low to moderate quality
evidence of positive effect for young people with ASD relating to some core autistic
characteristics, life outcomes and cognitive, motor and social-emotional skills. There is weak
Page 104 of 125
FOI 23/24- 1400
evidence showing improvement in functional outcomes for children with intellectual disability
and development delay.
SBIs are usually implemented by an occupational therapist. However, other professionals can
be trained to implement SBIs including nurses, psychologists and speech therapists.
3. Terminology
The literature on sensory therapies is not well organised and key terminology is not used
consistently (Ouellet et al, 2021). However, rough definitions of the major concepts are
possible.
3.1 Theoretical terminology
Underlying theoretical terms are often used in different ways. Brown et al (2019) provide an
overview of the use of the terms
sensory integration,
sensory processing, sensory
modulation and
sensory perception, showing that despite considerable variation, these
terms
have also been used interchangeably in the literature. Based on their review, the
authors propose the following definition of sensory modulation:
Sensory modulation is considered a twofold process. It originates in the central nervous
system as the neurological ability to regulate and process sensory stimuli; this
subsequently offers the individual an opportunity to respond behaviourally to the
stimulus (Brown et al, 2019, p.521).
They characterise sensory modulation as a combined neurophysiological and behavioural
process within the larger category of sensory processing. Sensory processing also includes:
receiving, organisation, perception, interpretation, registration and discrimination. They
suggest sensory integration is the framework which encompasses the sensory processing sub-
processes and the disorders associated with those subtypes (Brown et al, 2019).
However, we should also recognise that the process of proposing consistent definitions of
these terms is largely revisionary considering the disagreement in the literature. For instance,
sensory integration can refer to a neurological process, a theory or a practice depending on
the researcher. Sensory processing might be used interchangeably with sensory integration
(Camarat et al, 2020; Brown et al, 2019). Sensory processing is more often used in the
literature related to autism, but sensory modulation is often used in the literature on mental
health to refer to the same types of interventions (Brown et al, 2019; Hitch et al, 2020).
There is inconsistency in the definitions of sensory disorders as well. Diagnosis is made based
on the presence of i) difficulties translating sensory information into appropriate behavioural
responses and; ii) a demonstrable effect on activities of daily living (Ouellet, 2021). There is
some controversy about whether sensory disorders are genuinely separate conditions or
whether they are collections of symptoms associated with other conditions. The category of
sensory disorders is not included in either the DSM-5 or the ICD-11 (American Psychiatric
Association, 2013; World Health Organisation, 2019).
Page 105 of 125
FOI 23/24- 1400
3.2 Types of sensory based interventions
Terms for therapeutic practices are also used in incompatible ways (Ouellet et al, 2021). In
particular, there is an ambiguity in the use of the term
sensory based interventions.
SBI can refer to a category of therapeutic techniques that include sensory integration therapy
(SIT), auditory integration therapy (AIT), use of multi-sensory environments (MSE) and other
techniques that target sensory processing difficulties. Preis and McKenna (2014) and
Whitehouse et al (2020) use SBI in this way.
However, SBI can also refer to specific practices that are distinguished from SIT, AIT or MSE.
Ouellet et al (2021), Basic et al (2021) and Wans Yunus et al (2015) draw the distinction
between SIT and SBI based on the number of therapeutic modalities or stimuli. SBI is used to
refer to techniques that use singular discrete stimuli to achieve the desired result (e.g.,
massage, a weighted vest). SIT on the other hand, uses multiple integrated stimuli and must
include more than one sensory modality (Parham et al, 2007).
McGil and Breen (2019) note a further complication: SBI-type strategies are emerging in the
context of positive behaviour support and multi-element behavioural interventions without
being labelled as SBIs.
There does seem to be agreement that SBIs are based on the theoretical premise that sensory
processing differences affect skil acquisition and behavioural development. By targeting
sensory processing, the interventions aim to improve behavioural problems, emotional
regulation, cognitive, language and social skil s (Whitehouse et al, 2020).
Discrete SBIs, SIT, MSE and AIT are considered in further detail below. There are other
therapeutic practices that can be included under the label SBI. Whitehouse et al also consider
environmental enrichment, sensory diet and the following:
alternative seating; blanket or “body sock”; brushing with a bristle or a feather; chewing
on a rubber tube; developmental speech and language training through music; family-
centered music therapy; joint compression or stretching; jumping or bouncing; music
therapy; playing with a water and sand sensory table; playing with specially textured
toys; Qigong Sensory Treatment (QST); Rhythm Intervention Sensorimotor Enrichment;
sensory enrichment; swinging or rocking stimulation; Thai traditional massage; Tomatis
Sound Therapy; and weighted vests (Whitehouse et al, 2020, p.70).
SBIs are usually implemented by occupational therapists, although speech therapists, nurses,
psychologists and other professionals can be trained to implement programs (McGil & Breen,
2019).
3.2.1 Sensory-based interventions
SBI provides sensory stimuli that are specific or discrete to address behavioural problems
causes by dif iculties in sensory processing (Wan Yunus, 2015; Ouellet et al, 2021). The
distinction between sensory-based and sensorimotor-based approaches is drawn differently in
the literature. Ouellet et al (2021) says that sensory-based approaches involve a stimulus of
Page 106 of 125
FOI 23/24- 1400
constant intensity, such as a weighted vest, whereas sensorimotor-based approaches include
the use of movements, allowing the person to control the quantity and intensity of stimulation.
In contrast, Wan Yunus et al (2015) distinguish between tactile (eg. massage, touch therapy,
brushing), proprioceptive (eg. weighted vests) and vestibular (eg. therapy ball, cushions, horse
riding) based interventions. Vestibular interventions involve patient movements and variation in
the constancy of intensity of stimulus was not noted as a distinguishing feature of different
techniques.
3.2.2 Sensory integration therapy
Sensory integration therapy (sometimes sensory processing therapy) is defined as any
intervention that targets someone’s “ability to integrate sensory information (visual, auditory,
tactile, proprioceptive, and vestibular) from their body and environment in order to respond
using organized and adaptive behaviour” (Steinbrenner et al, 2020, p.29). Steinbrenner et al
(2020) regard SIT as synonymous with Ayers Sensory Integration (Ayers). Whereas Omairi et
al (2022) treat Ayers as just one frequently used type of SIT.
Ayers can include equipment such as mats, swings, scooter boards and bolsters in
“individually tailored sensorimotor activities that are contextualized in play at the just-right
challenge to facilitate adaptive behaviours for participation in tasks and activities” (Omairi et al,
2022, p.4; Whitehouse et al, 2020). There are 10 core elements of Ayers:
• Provide sensory opportunities – intervention includes various sensory experiences
(tactile, proprioceptive, vestibular) involving more than one sensory modality.
• Provide just-right challenges – sensory challenges are neither too dif icult nor too
easy for the individual
• Collaborate on activity choice – the participant is an active contributor to the
intervention including choice of activity
• Guide self-organisation – participant is encouraged to initiate, plan and organise
their own activities
• Support optimal arousal – the context should allow the child to maintain their optimal
level of arousal
• Create play context – the context builds on the participants intrinsic motivation and
enjoyment of activities
• Maximise child’s success – activities are tailored so that the child can experience
success
• Ensure physical safety – activities are tailored so that the child is safe and properly
supervised
Page 107 of 125

FOI 23/24- 1400
• Arrange room for engagement – the environment is organised to motivate the
participant to participate in activities
• Foster therapeutic alliance – the participant is treated with respect and allowed to
have their own emotional reactions to experiences (Parham et al, 2007; Wans
Yunus et al, 2015; Whitehouse et al, 2020).
3.2.3 Multi-sensory environment
MSEs (also called comfort rooms, sensory rooms or Snoezelen rooms) are rooms that contain
equipment used to modify the environment primarily with the aim to create sensory
experiences. This includes equipment used to create lights, sounds, smells or proprioceptive
and tactile sensations. The goal of an MSE is to soothe or stimulate a person with sensory
needs (Unwin et al, 2022; Cameron et al, 2020).
Figure 1 Multi-sensory room
MSEs are often windowless or have covered walls. They commonly include:
(1) projection equipment to provide changing light colours and patterns, (2) sound
(music) equipment, (3) bubble tubes offering visual, audible and tactile stimulation, (4)
waterbed, (5) fibre optic lighting, (6) tactile objects, (7) user-controlled switching for
changing lighting and other equipment, (8) weighted blankets, (9) self-massagers, (10)
rocking chair(s), (11) exercise balls, and (12) squeeze balls (Cameron et al, 2020,
p.631).
Rooms might also include essential oils, scented candles, sweet or salty foods (Cameron et al,
2020). Participants can control aspects of the environment thereby reducing the
unpredictability or the environment and allowing the participant to regulate their own sensory
stimulation (Unwin et al, 2022).
Page 108 of 125
FOI 23/24- 1400
3.2.4 Auditory integration training
AIT aims to ‘re-educate’ the auditory processing system of the patient’s brain with 2 half hour
electronic music listening sessions over 10 days. This re-education process is intended to
target behaviour and learning problems in people with autism (Sinha et al, 2011).
Wans Yunus et al (2015) suggest auditory integration training (AIT) is a based on the same
theory of sensory integration as SIT. However, because SIT involves multiple sensory
modalities (Parham et al, 2007), AIT can only be considered a related therapy rather than a
kind of SIT. Other related techniques include Tomatis sound therapy and Samonas sound
therapy (Sinha et al, 2011).
3.2.5 Music therapy
Music therapy is considered a type of SBI by some (Whitehouse et al, 2020; Cheung et al,
2022) and not others (Steinbrenner et al, 2020). The mechanism by which music therapy is
supposed to work does involve active listening and auditory sensory experiences, though it
also includes social and cognitive processes (Geretsegger et al, 2014).
4. Efficacy
Researchers and clinicians have suggested that sensory based interventions could benefit
people with autism spectrum disorder, ADHD, developmental coordination disorder, cerebral
palsy, down syndrome, intellectual disability, dementia, depression, schizophrenia, mood
disorders, obsessive compulsive disorder (Wan Yunus et al, 2015; Sinha et al, 2011; Hitch et
al, 2020; Ouellet et al, 2021).
4.1 Autism Spectrum Disorder
Steinbrenner et al (2020) and Whitehouse et al (2020) consider sensory-based interventions in
their reviews of evidence-based treatments for young people with ASD.
Steinbrenner et al added Ayers to their 2020 review of evidence-based practices for children
and young people with autism spectrum disorder. They note evidence of effect on
communication, social skil s, cognitive and academic outcomes, adaptive coping skil s,
challenging behaviour, and motor skil s (Steinbrenner et al, 2020). However, Steinbrenner et al
did not assess the evidence for ef icacy in detail, but only show that Ayers meet their criteria
for being considered an evidence-based practice:
To be identified as evidence-based, a category of practice had to contain (a) two high
quality group design studies conducted by two different research groups, or (b) five high
quality single case design studies conducted by three different research groups and
involving a total of 20 participants across studies, or (c) a combination of one high
quality group design study and three high quality single case design studies with the
combination being conducted by two independent research groups (Steinbrenner et al,
2020, p.24).
Page 109 of 125

FOI 23/24- 1400
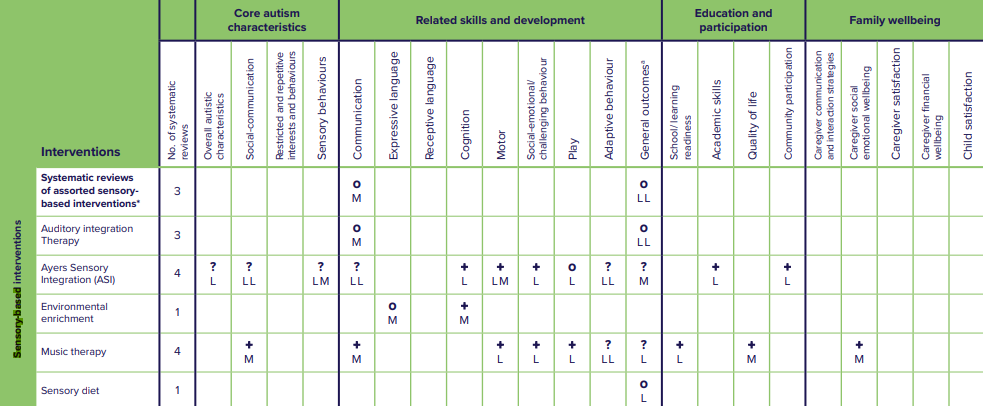
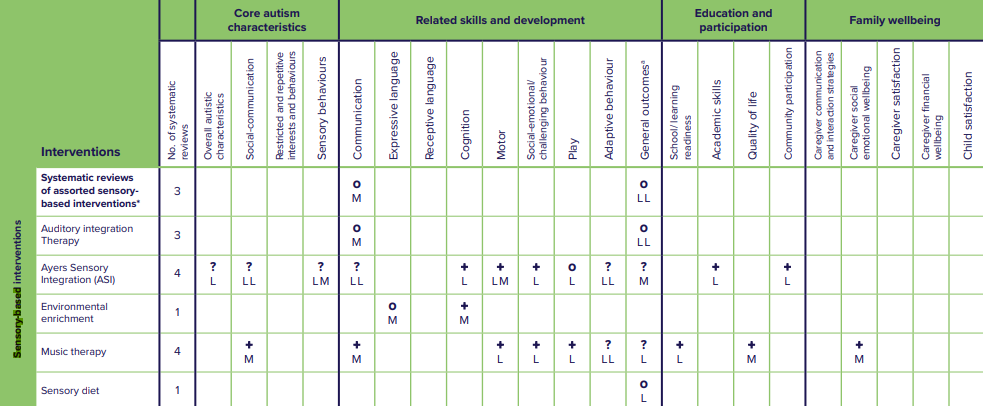
Whitehouse et al (2020) considered 9 systematic reviews. No evidence was found of a positive
effect for assorted SBIs, AIT or sensory diet. Environmental enrichment showed a positive
effect on motor skil s based on moderate quality evidence.
Ayers was considered in 4 reviews which showed low quality evidence of improvement to
cognition, motor skil s, challenging behaviours, academic skil s and community participation.
Reviewers also found moderate quality evidence of a benefit to motor skil s. Low or moderate
quality evidence showed inconsistent or null effect on autistic characteristics such as social-
communication and sensory behaviours, communication skil s, play, adaptive behaviour skil s,
and general outcomes. 1 review found evidence that SIT may contribute to increase in
stereotypical and problem behaviours (Whitehouse et al, 2020).
Music therapy demonstrated the most consistent positive effect. Reviewers found moderate
quality evidence showing positive effect on social-communication symptoms, communication
skills, and quality of life. Reviewers found low quality evidence showing positive effect on play,
motor skil s, challenging behaviours, and school readiness (Whitehouse et al, 2020).
Figure 2 Summary of evidence for sensory-based interventions. From Whitehouse et al, 2020, p.75
Wan Yunus et al (2015) argue that there is sufficient evidence that tactile stimulation (such as
massage therapy) positively affects challenging behaviours such that it can be included in
clinical practice. This contrasts with both Whitehouse et al (2020) and Steinbrenner et al
(2020) who note evidence that Ayers and music therapy can improve challenging behaviours,
but who do not recognise evidence that discrete tactile stimulation can improve challenging
behaviours.
Page 110 of 125
FOI 23/24- 1400
4.2 Mental Health
Sensory profiles of people with mental health conditions differ from the norm. Brown et al
(2020) found a general pattern of greater sensory sensitivity, sensation avoiding, and low
registration and less sensation seeking in a group of patients with either schizophrenia, high
risk for psychosis, bipolar disorder, major depressive disorder, posttraumatic stress and
obsessive-compulsive. Machingura et al (2022) confirmed higher rates of low registration and
sensory avoiding in a group of 41 people with schizophrenia.
SBIs are currently in use in mental health settings in Australia, including discrete SBIs and
MSEs. While the evidence base is stil emerging, existing studies consistently find an effect of
SBIs on distress. Multiple systematic reviews over the past 10 years have concluded that SBIs
are likely to contribute to a reduction in distress for patients with mental health issues in clinical
settings (Scanlon & Novak, 2015; Hitch et al, 2020; McGreevy & Boland, 2020; Ma et al, 2021;
Hain & Hallet, 2022). In a recent controlled trial, Machingura et al (2022) found a reduction in
distress for patients with schizophrenia when comparing pre- and post-test scores. However,
the effect was no longer statistically significant when compared with the control group.
SBIs are hypothesised to reduce the use of restrictive practice. State and national policies
aiming to reduce the use of restrictive practice are driving adoption of and research into SBIs
(Machingura et al, 2022; Baker et al, 2022; Baker et al, 2021; Hitch et al, 2020). The
suggestion is that if SBIs can reduce distress and level of arousal, then fewer episodes
requiring restrictive practice would occur. However, this assumption is questionable
considering the effect of workplace culture and institutional/state policy on rates of restrictive
practices (Scanlon & Novak, 2015). The evidence for an actual reduction in use of restrictive
practice is mixed.
Scanlon and Novak (2015) reviewed 17 papers and found that of the 9 studies reporting only
rates of restrictive practice use, all were using MSE type interventions. Of those studies 5
reported a reduction in rates of restraint or seclusion, 3 reported no change and 1 reported an
increase.
Other systematic reviews also show inconsistent evidence that MSEs used in clinical or
institutional settings can reduce restrictive practice. Haig and Hallett (2022) reviewed 6 studies
which reported rates or seclusion, restraint or violence. 4 of the 6 reported any positive results:
one out 6 studies found a reduction in seclusion episodes, 2 out of 6 found reductions in
restraint and 1 out of 6 found a reduction in aggression. One study also found an increase in
rates of seclusion. Haig and Hallett also note that all the studies reviewed had moderate to
high risk of bias.
Oostermeijer et al (2021) completed a rapid review including 14 studies on the effect of MSEs
on restrictive practices and found more positive results: 6 of the 14 studies found reduction in
restraint; 10 of the 14 found reduction in seclusion; 3 of the 14 reported no statistically
significant results; and 3 of the 14 reported an increase in restraint or seclusion.
Page 111 of 125
link to page 4 link to page 4
FOI 23/24- 1400
None of the systematic reviews were able to complete a meta-analysis. The inconsistency of
the evidence regarding MSEs effect on restrictive practice may relate to the unstructured and
heterogeneous nature of the intervention. There may be effective MSE-based practices or
protocols but existing studies have not identified them (Oostermeijer et al, 2021; Haig &
Hallett, 2022).
Most research on SBIs for people with mental health conditions occurs in a clinical or
institutional setting. Lack of research in community use of SBIs is a significant limitation of the
existing research (Hitch et al, 2020).
Hitch et al (2020) argue that despite minimal evidence, there is at least sufficient evidence to
support wider use in clinical settings due to minimal cost of implementation of many sensory
based interventions (for example, the discrete SBIs described i
n 3.2.1 Sensory-based
interventions).
4.3 Other conditions
There is some evidence that SBIs (especially MSEs, massage and music therapy) can
contribute to reduction in distress and agitation for people with dementia (Livingston et al,
2014; Pinto et al, 2020; Cheung et al, 2022).
Fisher et al (2014; 2017) show minimal evidence that SBI can reduce aggression in people
with Huntington’s disease.
Kantor et al (2022) found positive effects of Ayers on motor skil s of children with cerebral
palsy. However, better quality evidence is required to draw reliable conclusions.
A 2015 meta-analysis found only weak evidence for the efficacy of SIT in improving functional
outcomes for children with intellectual disability and development delay (Leong et al, 2015).
Subsequent studies have shown that SIT can assist children with developmental delay when
combined with a more comprehensive early intervention program (Wang et al, 2020).
5. References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental
disorders (5th ed.).
https://doi.org/10.1176/appi.books.9780890425596
Baker, J., Berzins, K., Canvin, K., Benson, I., Kel ar, I., Wright, J., Lopez, R. R., Duxbury, J.,
Kendall, T., & Stewart, D. (2021). Non-pharmacological interventions to reduce
restrictive practices in adult mental health inpatient settings: the COMPARE systematic
mapping review.
Health Services and Delivery Research,
9(5), 1–184.
https://doi.org/10.3310/hsdr09050
Baker, J., Berzins, K., Canvin, K., Kendal, S., Branthonne-Foster, S., Wright, J., McDougal , T.,
Goldson, B., Kellar, I., & Duxbury, J. (2022). Components of interventions to reduce
restrictive practices with children and young people in institutional settings: the Contrast
Page 112 of 125
FOI 23/24- 1400
systematic mapping review.
Health and Social Care Delivery Research,
10(8), 1–180.
https://doi.org/10.3310/yvkt5692
Basic, A., Macesic Petrovic, D., Pantovic, L., Zdravkovic Parezanovic, R., Gajic, A., Arsic, B.,
Nikolic, J. (2021). Sensory integration and activities that promote sensory integration in
children with autism spectrum disorders.
Journal Human Research in Rehabilitation,
11(1), 28–38.
https://doi.org/10.21554/hrr.042104
Brown, A., Tse, T., & Fortune, T. (2019). Defining sensory modulation: A review of the concept
and a contemporary definition for application by occupational therapists.
Scandinavian
Journal of Occupational Therapy,
26(7), 515–523.
https://doi.org/10.1080/11038128.2018.1509370
Brown, C., Karim, R., & Steuter, M. (2020). Retrospective analysis of studies examining
sensory processing preferences in people with a psychiatric condition.
The American
Journal of Occupational Therapy: Official Publication of the American Occupational
Therapy Association,
74(4), 7404205130p1-7404205130p11.
https://doi.org/10.5014/ajot.2020.038463
Cameron, A., Burns, P., Garner, A., Lau, S., Dixon, R., Pascoe, C., & Szafraniec, M. (2020).
Making sense of multi-sensory environments: A scoping review.
International Journal of
Disability, Development, and Education,
67(6), 630–656.
https://doi.org/10.1080/1034912x.2019.1634247
Cheung, D. S. K., Wang, S. S., Li, Y., Ho, K. H. M., Kwok, R. K. H., Mo, S. H., & Bressington,
D. (2022). Sensory-based interventions for the immediate de-escalation of agitation in
people with dementia: A systematic review.
Aging & Mental Health, 1–12.
https://doi.org/10.1080/13607863.2022.2116404
Fisher, C. A., Sewell, K., Brown, A., & Churchyard, A. (2014). Aggression in Huntington’s
disease: a systematic review of rates of aggression and treatment methods.
Journal of
Huntington’s Disease,
3(4), 319–332.
https:/ doi.org/10.3233/JHD-140127
Fisher, C. A., & Brown, A. (2017). Sensory modulation intervention and behaviour support
modification for the treatment of severe aggression in Huntington’s disease. A single
case experimental design.
Neuropsychological Rehabilitation,
27(6), 891–903.
https://doi.org/10.1080/09602011.2015.1091779
Geretsegger, M., Elefant, C., Mössler, K. A., & Gold, C. (2014). Music therapy for people with
autism spectrum disorder.
Cochrane Database of Systematic Reviews,
2016(6),
CD004381.
https://doi.org/10.1002/14651858.CD004381.pub3
Haig, S., & Hallett, N. (2022). Use of sensory rooms in adult psychiatric inpatient settings: A
systematic review and narrative synthesis.
International Journal of Mental Health
Nursing. https:/ doi.org/10.1111/inm.13065
Hitch D, Wilson C, Hillman A. (2020) Sensory modulation in mental health practice. Mental
Health Practice.
https:/ doi.org/10.7748/mhp.2020.e1422
Page 113 of 125
FOI 23/24- 1400
Kantor, J., Hlaváčková, L., Du, J., Dvořáková, P., Svobodová, Z., Karasová, K., & Kantorová,
L. (2022). The effects of Ayres sensory integration and related sensory based
interventions in children with cerebral palsy: A scoping review.
Children (Basel,
Switzerland),
9(4), 483.
https://doi.org/10.3390/children9040483
Leong, H. M., Carter, M., & Stephenson, J. R. (2015). Meta-analysis of research on sensory
integration therapy for individuals with developmental and learning disabilities.
Journal
of Developmental and Physical Disabilities,
27(2), 183–206.
https://doi.org/10.1007/s10882-014-9408-y
Livingston, G., Kelly, L., Lewis-Holmes, E., Baio, G., Morris, S., Patel, N., Omar, R. Z., Katona,
C., & Cooper, C. (2014). A systematic review of the clinical effectiveness and cost-
effectiveness of sensory, psychological and behavioural interventions for managing
agitation in older adults with dementia.
Health Technology Assessment (Winchester,
England),
18(39), 1–226, v–vi.
https://doi.org/10.3310/hta18390
Ma, D., Su, J., Wang, H., Zhao, Y., Li, H., Li, Y., Zhang, X., Qi, Y., & Sun, J. (2021). Sensory-
based approaches in psychiatric care: A systematic mixed-methods review.
Journal of
Advanced Nursing,
77(10), 3991–4004.
https://doi.org/10.1111/jan.14884
Machingura, T., Shum, D., Lloyd, C., Murphy, K., Rathbone, E., & Green, H. (2022).
Effectiveness of sensory modulation for people with schizophrenia: A multisite
quantitative prospective cohort study.
Australian Occupational Therapy Journal,
69(4),
424–435.
https://doi.org/10.1111/1440-1630.12803
McGil , C., & Breen, C. J. (2020). Can sensory integration have a role in multi‐element
behavioural intervention? An evaluation of factors associated with the management of
challenging behaviour in community adult learning disability services.
British Journal of
Learning Disabilities,
48(2), 142–153.
https:/ doi.org/10.1111/bld.12308
McGreevy, S., & Boland, P. (2020). Sensory-based interventions with adult and adolescent
trauma survivors: An integrative review of the occupational therapy literature.
Irish
Journal of Occupational Therapy,
48(1), 31–54.
https://doi.org/10.1108/ijot-10-2019-
0014
Omairi, C., Mail oux, Z., Antoniuk, S. A., & Schaaf, R. (2022). Occupational therapy using
Ayres Sensory Integration®: A randomized controlled trial in Brazil.
The American
Journal of Occupational Therapy: Official Publication of the American Occupational
Therapy Association,
76(4).
https://doi.org/10.5014/ajot.2022.048249
Oostermeijer, S., Brasier, C., Harvey, C., Hamilton, B., Roper, C., Martel, A., Fletcher, J., &
Brophy, L. (2021). Design features that reduce the use of seclusion and restraint in
mental health facilities: a rapid systematic review.
BMJ Open,
11(7), e046647.
https://doi.org/10.1136/bmjopen-2020-046647
Ouellet, B., Carreau, E., Dion, V., Rouat, A., Tremblay, E., & Voisin, J. I. A. (2021). Efficacy of
sensory interventions on school participation of children with sensory disorders: A
Page 114 of 125
FOI 23/24- 1400
systematic review.
American Journal of Lifestyle Medicine,
15(1), 75–83.
https://doi.org/10.1177/1559827618784274
Parham, L. D., Cohn, E. S., Spitzer, S., Koomar, J. A., Mil er, L. J., Burke, J. P., Brett-Green,
B., Mail oux, Z., May-Benson, T. A., Roley, S. S., Schaaf, R. C., Schoen, S. A., &
Summers, C. A. (2007). Fidelity in sensory integration intervention research.
The
American Journal of Occupational Therapy: Official Publication of the American
Occupational Therapy Association,
61(2), 216–227.
https://doi.org/10.5014/ajot.61.2.216
Pinto, J. O., Dores, A. R., Geraldo, A., Peixoto, B., & Barbosa, F. (2020). Sensory stimulation
programs in dementia: a systematic review of methods and effectiveness.
Expert
Review of Neurotherapeutics,
20(12), 1229–1247.
https://doi.org/10.1080/14737175.2020.1825942
Preis, J., & McKenna, M. (2014). The effects of sensory integration therapy on verbal
expression and engagement in children with autism.
International Journal of Therapy
and Rehabilitation,
21(10), 476–486.
https://doi.org/10.12968/ijtr.2014.21.10.476
Scanlan, J. N., & Novak, T. (2015). Sensory approaches in mental health: A scoping review.
Australian Occupational Therapy Journal,
62(5), 277–285.
https://doi.org/10.1111/1440-
1630.12224
Sinha, Y., Silove, N., Hayen, A., & Wil iams, K. (2011). Auditory integration training and other
sound therapies for autism spectrum disorders (ASD).
Cochrane Database of
Systematic Reviews,
12, CD003681.
https://doi.org/10.1002/14651858.CD003681.pub3
Steinbrenner, J. R., Hume, K., Odom, S. L., Morin, K. L., Nowel , S. W., Tomaszewski, B.,
Szendrey, S., McIntyre, N. S., Yücesoy-Özkan, S., & Savage, M. N. (2020). Evidence-
based practices for children, youth, and young adults with Autism. The University of
North Carolina at Chapel Hil , Frank Porter Graham Child Development Institute,
National Clearinghouse on Autism Evidence and Practice Review Team.
Unwin, K. L., Powell, G., & Jones, C. R. (2022). The use of Multi-Sensory Environments with
autistic children: Exploring the effect of having control of sensory changes.
Autism: The
International Journal of Research and Practice,
26(6), 1379–1394.
https://doi.org/10.1177/13623613211050176
Wan Yunus, F., Liu, K. P. Y., Bissett, M., & Penkala, S. (2015). Sensory-based intervention for
children with behavioral problems: A systematic review.
Journal of Autism and
Developmental Disorders,
45(11), 3565–3579.
https:/ doi.org/10.1007/s10803-015-
2503-9
Wang, L.-J., Hsieh, H.-Y., Chen, L.-Y., Ko, K.-L., Liu, H.-H., Chou, W.-J., Chou, M.-C., & Tsai,
C.-S. (2020). Adjunctive sensory integration therapy for children with developmental
disabilities in a family-based early intervention program.
Taiwanese Journal of
Psychiatry,
34(3), 121.
https://doi.org/10.4103/tpsy.tpsy 26 20
Page 115 of 125
FOI 23/24- 1400
Whitehouse, A., Varcin, K., Waddington, H., Sulek, R., Bent, C., Ashburner, J., Eapen, V.,
Goodall, E., Hudry, K., Roberts, J., Silove, N., Trembath, D. (2020). Interventions for
children on the autism spectrum: A synthesis of research evidence. Autism CRC,
Brisbane
World Health Organization. (2019). ICD-11: International classification of diseases (11th
revision).
https://icd.who.int/
Page 116 of 125