FOI 23/24-1244
DOCUMENT 1
OFFICIAL
Knowledge Article
For Internal Use Only
The contents of this document are OFFICIAL.
Guide - Therapy supports Appendix B
Guidance in this document is not approved for use unless you view it in PACE.
This article provides guidance for a
planner delegate, internal review delegate, national
reassessment delegate, local area coordinator, early childhood partner, technical
advisors, liaison officers (HLO/JLO) or
complex support needs (CSN) planner to
understand:
• case examples of participants who need therapy supports.
Recent updates
October 2023
This guidance comes from the Practice Guide – Understanding Therapy Supports. We've
made minor updates to change any NDIS Business System language to PACE language. We'll
make improvements to this guidance in the future.
Before you start (optional)
You have read and understood:
• Our Guideline – Reasonable and necessary supports (external)
• Our Guideline – Creating your plan (external)
• What principles do we follow to create your plan? (external)
• Our Guideline – Mainstream and community supports (external).
Case example
Arnold is 10 years old. He lives at home with his parents and two siblings. He has a diagnosis
of Down Syndrome and is experiencing difficulty with communication, social skills and mobility.
He attends a mainstream school where he receives support from a teacher’s aide.
During his previous plan, Arnold had difficulties building rapport with his therapists. This was
due to negative behaviours and difficulty travelling to and waiting in his therapist’s office. This
resulted in intermittent engagement and Arnold not using all of his capacity building supports.
The Allied Health Professionals (AHPS) progress report from the previous plan period
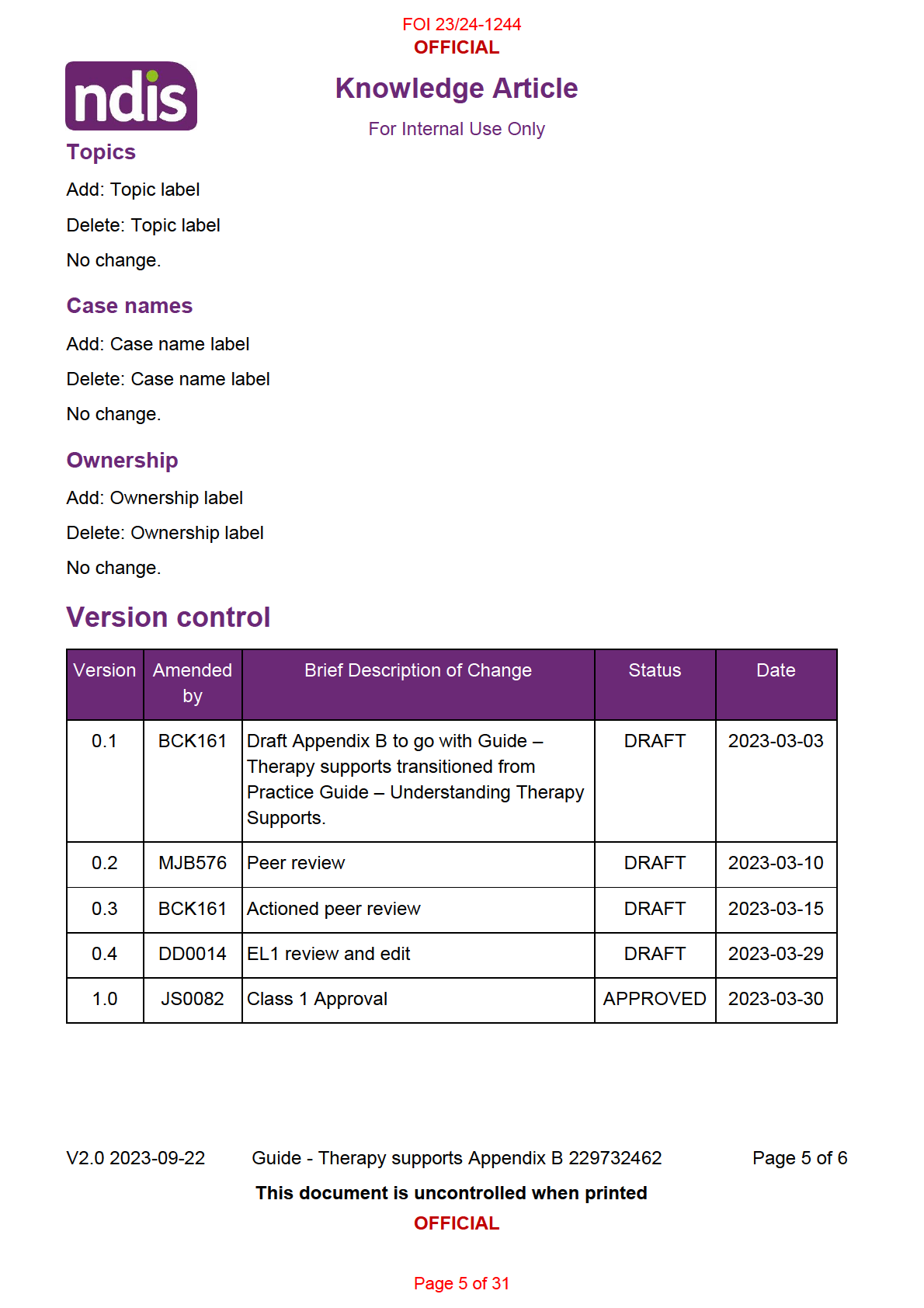
V2.0 2023-09-22
Guide - Therapy supports Appendix B 229732462
Page 1 of 6
This document is uncontrolled when printed
OFFICIAL
Page 1 of 31

FOI 23/24-1244
OFFICIAL
Knowledge Article
For Internal Use Only
recommended using a multidisciplinary approach of music, occupational and speech therapy,
focused on skill-building in Arnold’s natural environments to assist him to pursue his goals.
Progress report recommendations
16 hours of occupational therapy to work towards Arnold’s goal “To join in playground games
with friends”:
• Develop strategies to assist Arnold to increase motor control.
• Develop strategies to assist Arnold to increase social skills.
• Provide guidance to important people in Arnold’s life on ways he can be supported to join
in games and the types of exercises and games he can do to build his endurance and
muscle control.
Expected outcomes: Arnold will participate in a structured climbing activity or game with two
peers with minimal adult support.
12 hours of speech therapy to work towards Arnold’s goal of “Be able to tell people what I want
or need”:
• Communicate using 1-2 word phrases.
• Support communication through picture exchange while developing speech.
• Provide guidance to the important people in Arnold’s life on techniques specific to Arnold
to assist with communication.
Expected outcomes: Arnold will use 1-2 word picture exchange to request a motivating item
or a need.
7 hours of music therapy to develop strategies to motivate Arnold to engage with other
therapists by:
• Writing a song to motivate Arnold to participate in 1-2 word phrases.
• Use rhythmic and motivational elements of music to encourage Arnold to engage and
participate in gross and fine motor activities.
Outcomes:
Arnold will engage with the occupational therapist, speech pathologist and music
therapist to develop his communication and motor skills.
• $300 of low cost assistive technology (AT) to develop communication supports. Picture
exchange.
• Travel associated with delivery of supports in Arnold’s natural environments
V2.0 2023-09-22
Guide - Therapy supports Appendix B 229732462
Page 2 of 6
This document is uncontrolled when printed
OFFICIAL
Page 2 of 31

FOI 23/24-1244
OFFICIAL
Knowledge Article
For Internal Use Only
• 10 hours of report writing.
Check-in conversation
During the check-in, Arnold and his family discussed how they and other people in Arnold’s life
can assist him to develop his skills and become more independent. The strategies they
discussed included:
• AHPs will meet at the start and mid-way through Arnold’s plan to discuss strategies and
how these will complement each other.
• Each AHP will develop strategies to assist Arnold to work towards his goals and guide
the people in Arnold’s life on building his skills and independence.
• The school is using picture exchange with other students and will support Arnold to use
picture exchange if he is unable to verbalise his wants or needs.
• Arnold’s siblings are close to him and enjoy playing games. They can find it difficult when
he gets upset. Arnold’s parents and siblings have shown enthusiasm with structuring
some group activities/games with the family to help him develop his social skills.
Arnold attends Scouts on a Thursday night. He has a support worker to assist him to attend
and participate in activities. The support worker can implement strategies to assist Arnold to be
more independent in interactions with peers.
Outcome
The included information from the check-in and progress report provides enough evidence for
the planner to make a reasonable and necessary decision to include the recommended
therapy support hours in Arnold’s next plan.
Core – Consumables
$300 of low cost assistive technology has been included for the development of individualised
picture exchange cards as recommended by the speech pathologist. These cards will support
Arnold to communicate which will develop independence and increase participation in social,
school and community activities. This will reduce reliance on supports in the future. Funding
has been included in Capacity Building – Improved Daily Living Skills for Arnold’s supports to
receive training on implementing communication strategies.
Capacity Building – Improved Daily Living Skills
V2.0 2023-09-22
Guide - Therapy supports Appendix B 229732462
Page 3 of 6
This document is uncontrolled when printed
OFFICIAL
Page 3 of 31

FOI 23/24-1244
OFFICIAL
Knowledge Article
For Internal Use Only
45 hours of support has been included for a multidisciplinary team to build Arnold’s capacity in
communication, mobility and social skills. The multidisciplinary team will meet at the start and
mid-way through the plan period to create consistency in their approach.
Arnold had difficulties in the last plan period engaging with therapists and is highly motivated
by music. The progress report from the AHPs has recommended a music therapist be
engaged to develop strategies that will motivate Arnold to engage with other therapists to
develop his skills. This will increase participation in school, home and community life and is
likely to result in a reduced need of supports in the future.
Arnold will be assisted to implement communication, mobility and social skills strategies by his
family at home, teacher’s aide at school and support worker during Scouts.
Funding has been included for:
• 16 hours of occupational therapy to work with Arnold to achieve his goal of joining in
playground games with friends. The occupational therapist (OT) will provide training to
informal and formal supports on how to implement these strategies.
• 12 hours of speech therapy to work with Arnold to achieve his goal of telling people what
he wants or needs. The speech pathologist will work with Arnold to develop strategies to
communicate using picture exchange, while he develops 1-2 word phrases in speech.
The speech pathologist will provide training to informal and formal supports on how to
implement these strategies.
• 7 hours of music therapy to develop strategies to motivate Arnold to engage with other
therapists.
• 10 hours of report writing to understand the benefits and gains achieved by Arnold
across the plan period.
Funding has been included for travel of the allied health professionals to deliver supports in
Arnold’s natural environments.
Article labels
PACE user role names
Add: User role name label
Delete: User role name label
No change.
V2.0 2023-09-22
Guide - Therapy supports Appendix B 229732462
Page 4 of 6
This document is uncontrolled when printed
OFFICIAL
Page 4 of 31
FOI 23/24-1244
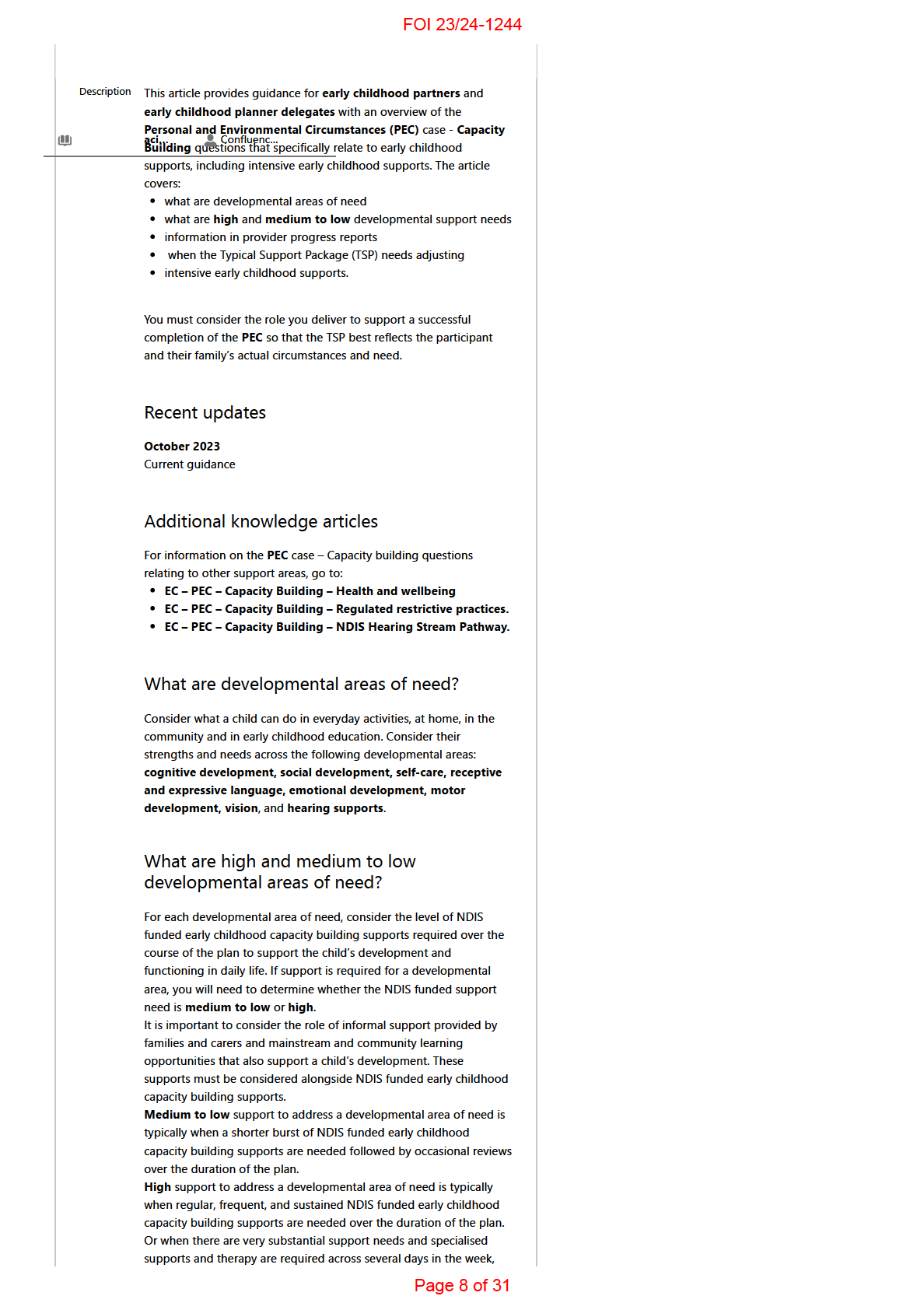
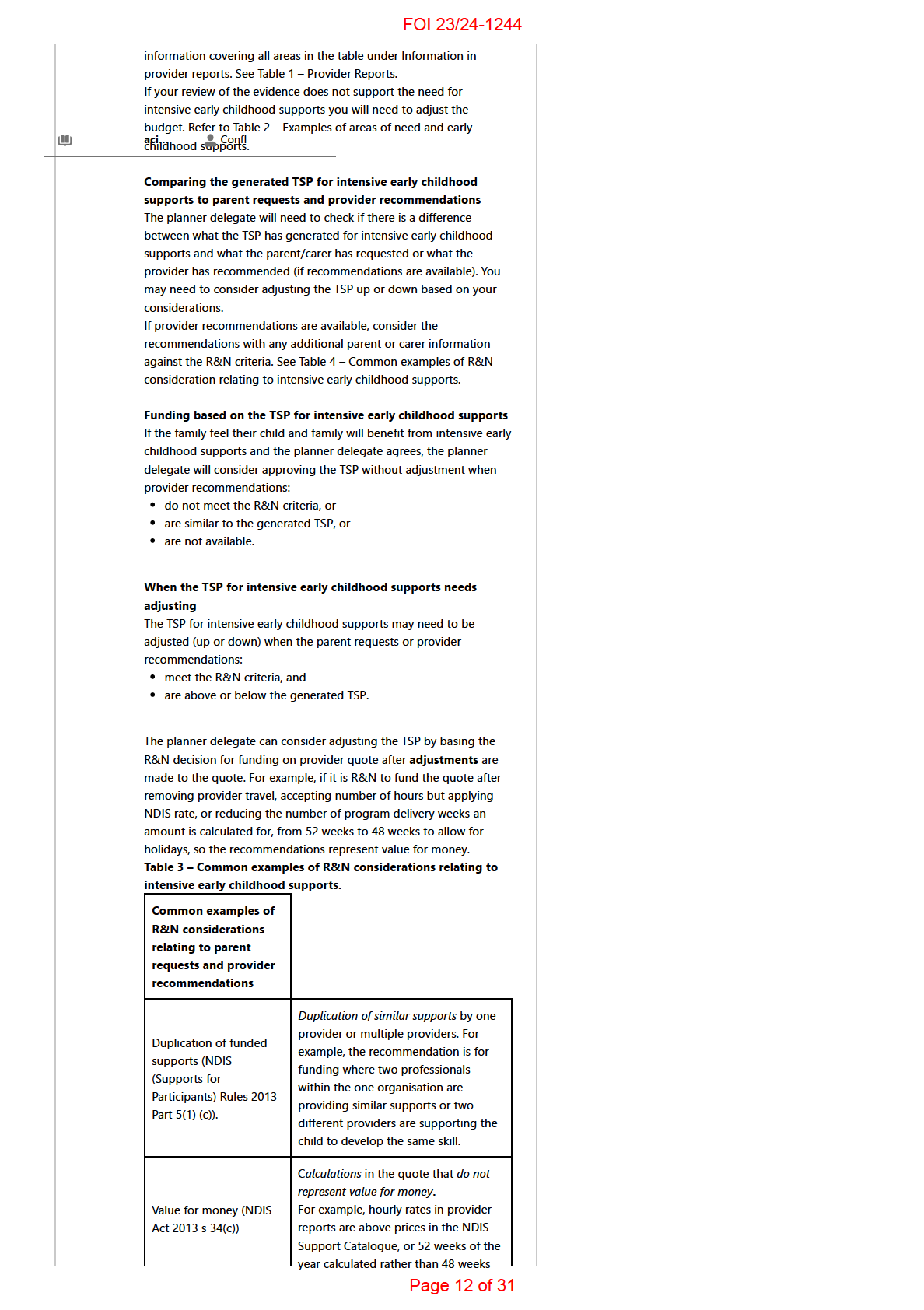
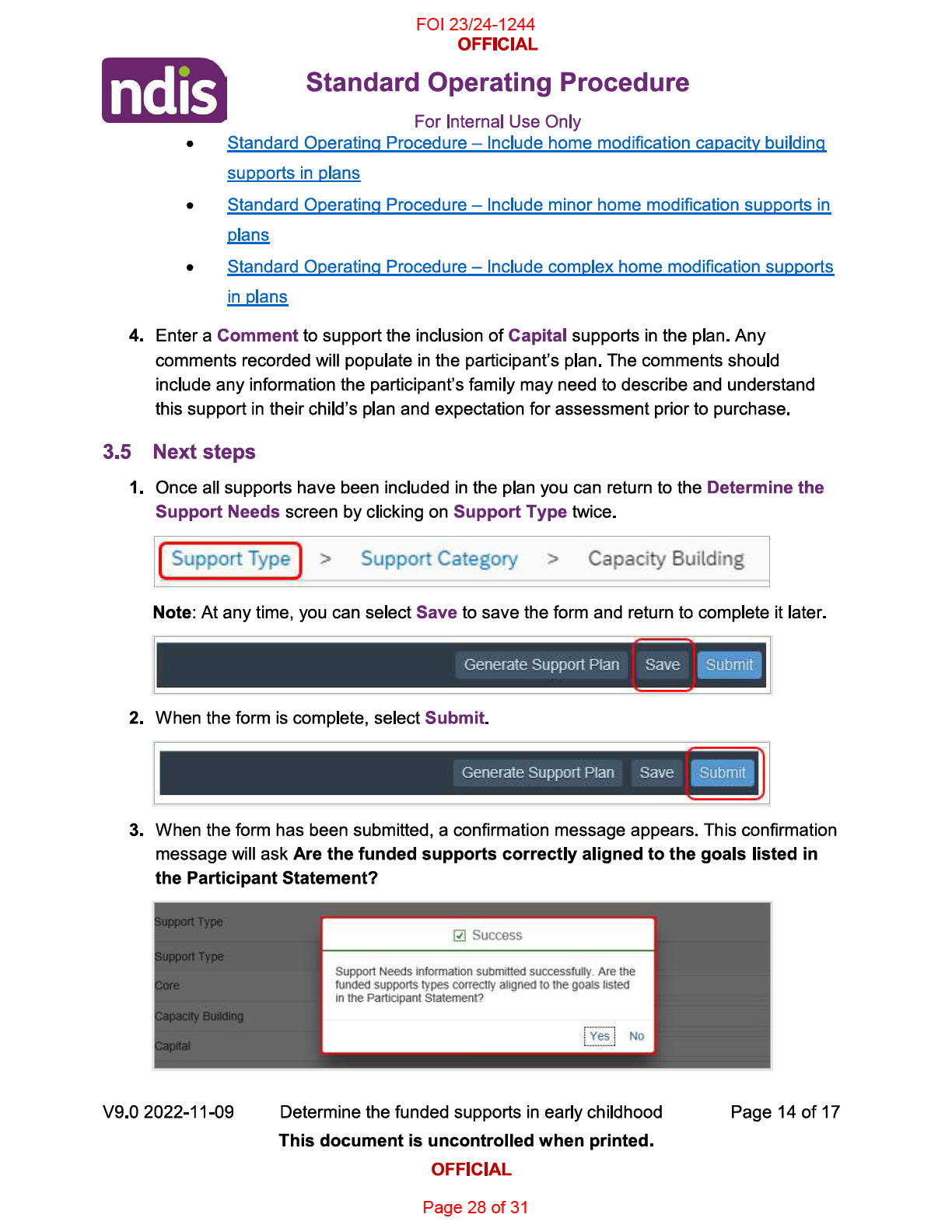
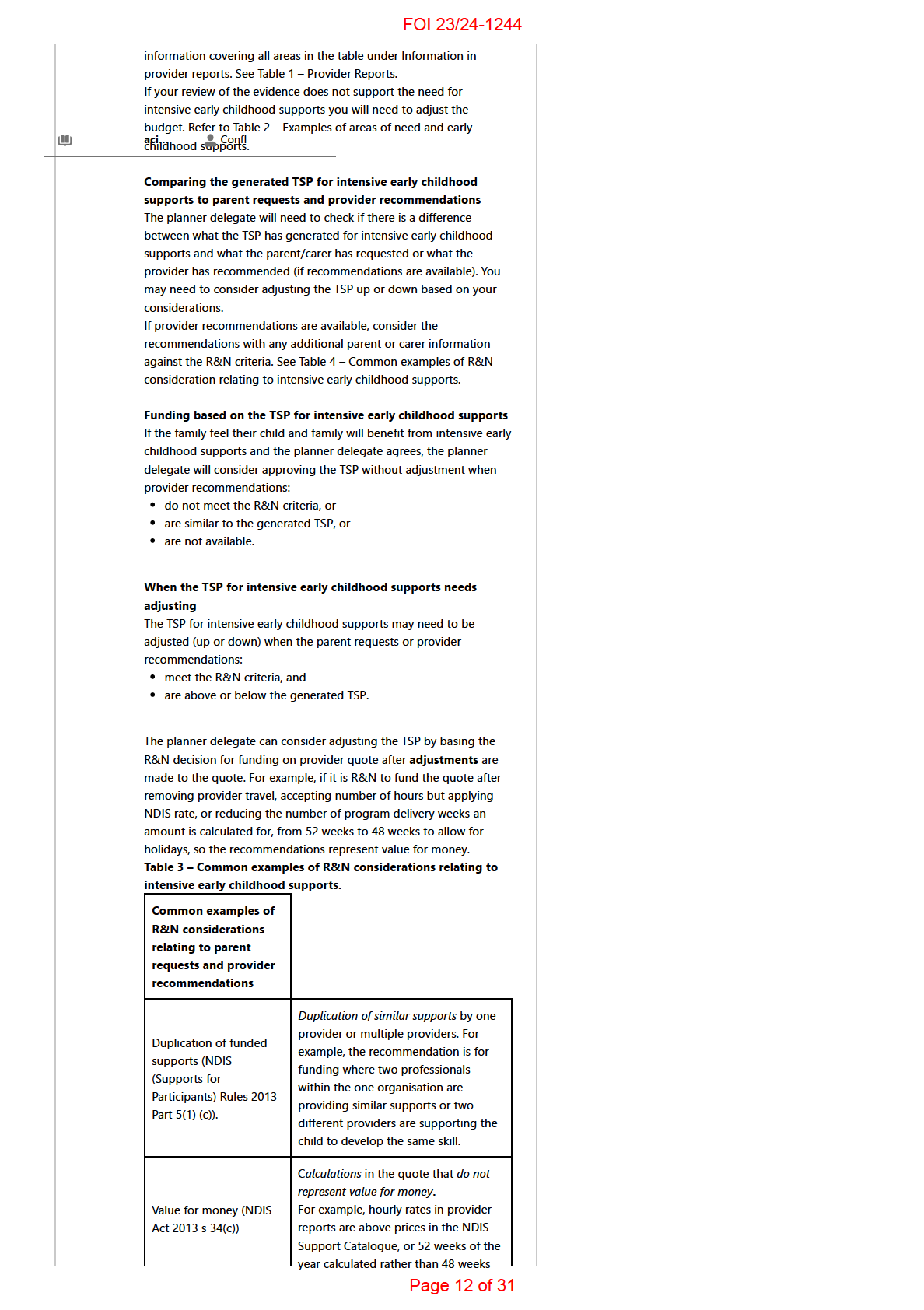
with school.
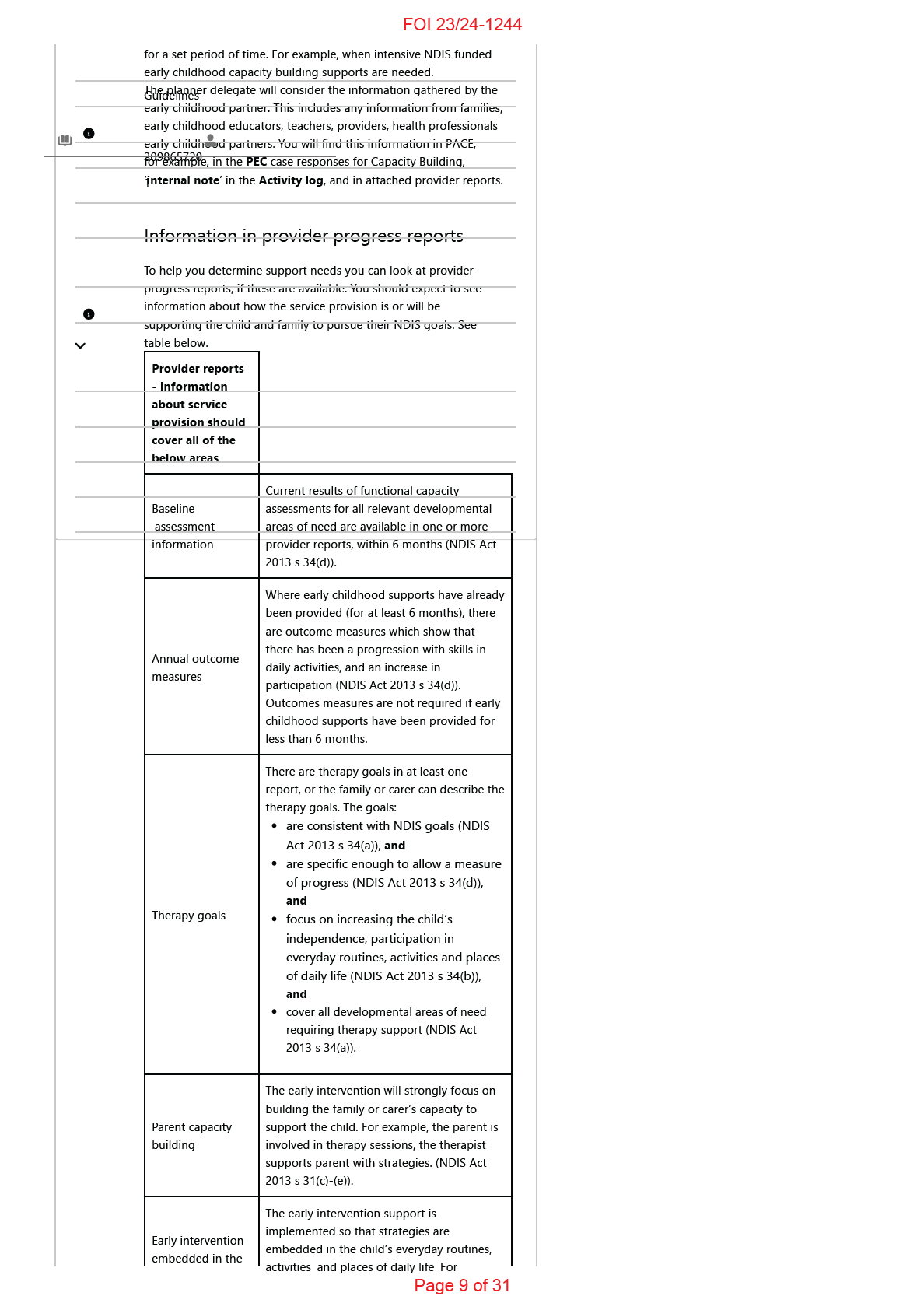
Regular early intervention supports for 12 months
(individual and/or group). Includes longer term
secondary consultation/s for all areas of need
and a progress report.
3 high areas
For a child in an early childhood setting:
+ 1 to 3
Fortnightly key worker visits for 1 term, followed
medium to
by less frequent visits for remaining terms, per
low areas
setting by key worker.
For a child transitioning to school: Child and
family support, consultation (visits or meetings)
with school.
Regular early intervention supports for 12 months
(individual and/or group). Includes longer term
secondary consultation/s for all areas of need
and a progress report.
For a child in an early childhood setting:
4 or more
Fortnightly key worker visits for 1 term, followed
high areas
by less frequent visits for remaining terms, per
setting by key worker.
For a child transitioning to school: Child and
family support, consultation (visits or meetings)
with school.
Intensive early childhood supports
Intensive early childhood supports are for children who have very
substantial capacity building support needs to maximise their
independence and participation in daily life. Most children with
developmental delay or disability do not need intensive early
childhood supports.
Intensive early childhood supports do not include supports relating
to: core supports, disability-related health supports, assistive
technology (or capacity building supports for assistive technology) or
behaviour support plans with restrictive practices.
The requests or recommendations for intensive early childhood
supports can come from a family or carer, a provider, a health
professional, or an early childhood partner.
Consideration for intensive early childhood supports is given to
requests or recommendations that are greater than $24,000.
When more than 1 provider is engaged, this refers to the total
amount recommended across all providers that the family is
requesting support for.
A TSP will generate for intensive early childhood supports if in the
PEC case the early childhood partner has indicated that a parent or
provider has identified that there is need for intensive early childhood
supports and this is supported by the family. The early childhood
partner is required to attach any relevant reports available that are
related to the request.
To approve intensive early childhood supports you must ensure there
is evidence to show that the support is required for the main areas of
need related to a child’s diagnosis. You must also ensure that very
substantial support is required for capacity building to support
participation in a range of activities in all of the following:
daily life in the home, and
daily life in the community, and
early childhood education and care or school, and
family life.
You can look for this information within PACE which was gathered by
the early childhood partner. For example, in the PEC case responses
for Daily Support and Capacity Building.
If a provider is already providing services to the child and family you
should expect to see a report attached in PACE that includes
Page 11 of 31
FOI 23/24-1244
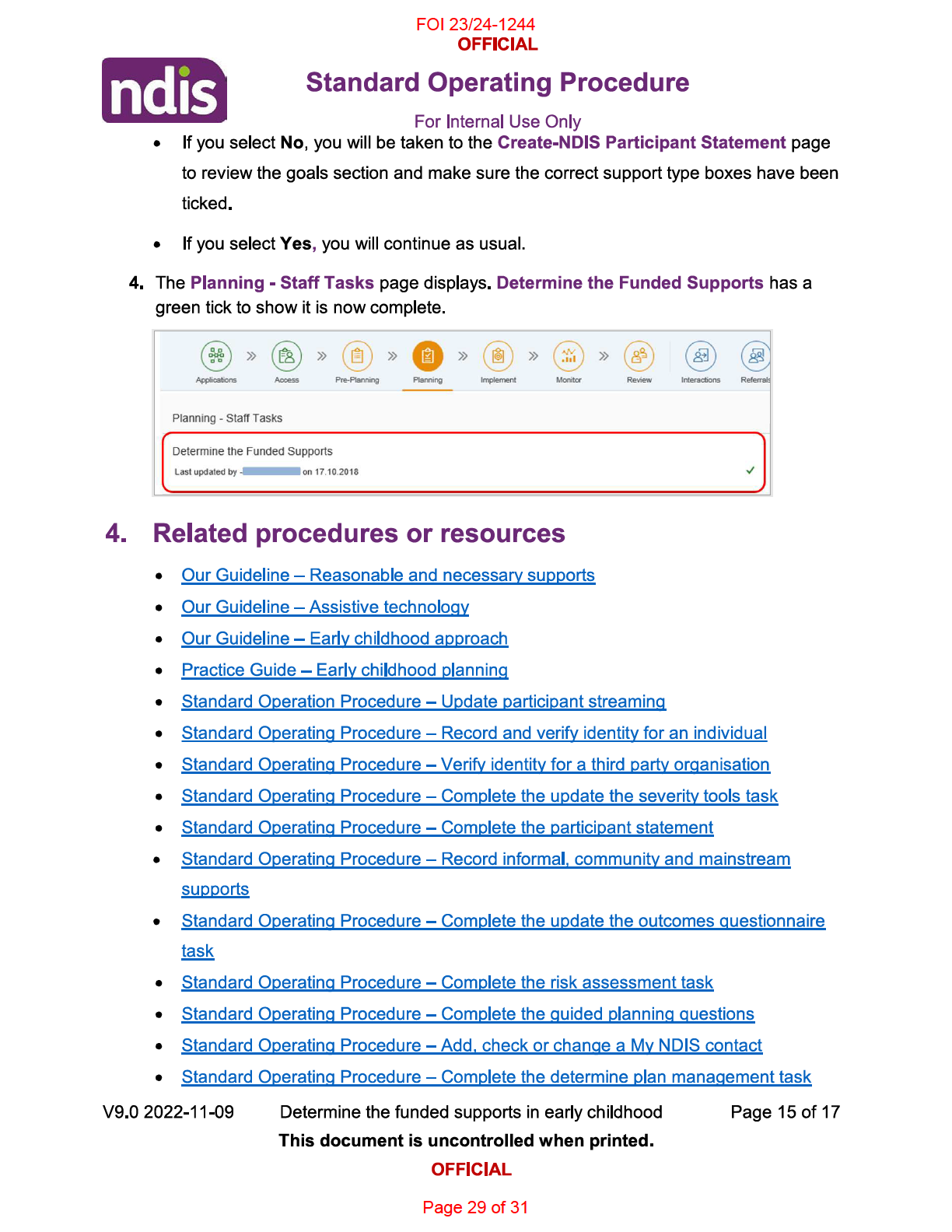
Requested supports that are excessive
compared to the outcomes to be
achieved. For example, the provider
recommends an increase in funding
which is not justified in reports, the
provider recommends funding for an
intensive toilet training program in
addition to a comprehensive early
intervention program which supports
the area of self-care.
Hours for
provider travel (not including
remote MMM6, very remote MMM7),
Value for money (NDIS
report writing, multiple staff attending
Act 2013 s 34(c))
the same meeting, professional
development,
do not represent value
for money.
Delivery of service or recommendations
made by a
professional who is
not
qualified.
Effective and beneficial,
For example, a therapy assistant has
having regard to current
written the therapy program, or
good practice (NDIS Act
recommendations include funding for
2013 s 34(d))
a behaviour therapist (rather than
allied health professional) to supervise
a therapy program.
Supports and programs with a
low
Effective and beneficial,
evidence base when considering the
having regard to current
best available research evidence. For
good practice (NDIS Act
example, equine therapy, dance
2013 s 34(d))
therapy.
Recommendation includes funding for
a support which is more appropriately
More appropriately
provided by mainstream and
funded or provided
community supports. For example, a
through other general
therapy assistant in a preschool, a
systems (NDIS Act 2013
therapist to teach a child to read, or
s 34(f)).
therapy that is recommended on days
when the child should be at a
mainstream setting.
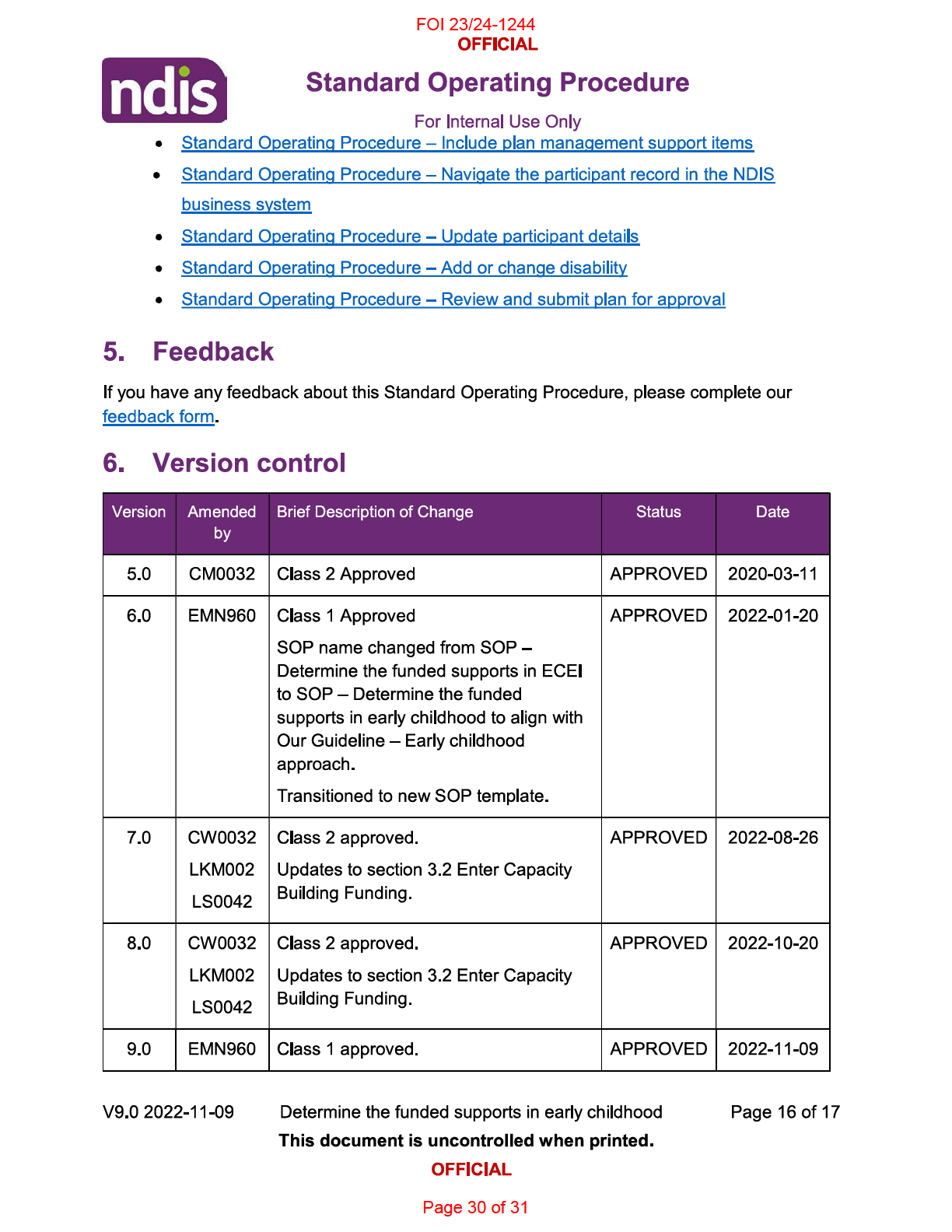
How long can intensive supports be funded in a plan?
If a child’s NDIS plan has intensive early childhood supports, it will
typically go for 12 months.
When approving intensive early childhood supports in a plan, it is
important that you discuss with parents or carers that, almost always,
the need for intensive supports will reduce over time. This is because:
their child’s disability support needs are likely to change as their
child independence and participation increases
their child is likely to start participating in other services such as
early childhood education and care or school. The early
childhood education and care service or school will provide some
of the supports their child needs.
When you reassess the child’s plan some of things you will need to
consider include:
how the support has helped to build the family and child’s skills
to maximise their independence
how the child takes part at home, in the community, and in
mainstream settings
if the supports have helped the child use the skills they have
learned with different people, across different settings and
activities.
whether the child continues to use the things they have learned
Page 13 of 31
FOI 23/24-1244
over time.
Page 14 of 31

FOI 23/24-1244
Page 31 of 31