FOI 24/25- 0013
DOCUMENT 21
Research – Dialectical Behavioural Therapy
The AAB have requested further information Dialectical Behavioural Therapy
(DBT).
The Applicant is a 23yo female with Asperger’s Syndrome, ASD and/or
Dissociative Identity Disorder.
In preparation for hearing of the matter, the AAB have requested a high level
review of DBT, in particular in application and effectiveness. They would also like
information to assist in determining whether DBT constitutes a treatment for
mental health and who would be responsible for funding treatment under
APTOS.
Further to above, please provide information on the treatment DBT, e.g. :
• What is DBT?
Brief
• What is the evidence base for DBT?
• What is the effectiveness of DBT?
• What is the general application of DBT?
• What conditions is DBT recommended for? (Particularly interested
in any application/ evidence for Asperger’s Syndrome, ASD and/or
Dissociative Identity Disorder)
• Is DBT a recommended for mental health conditions?
• What funding options are available for treatment of DBT? E.g.
under Health or Mental Health services
• Please provide a list of possible experts in DBT in Australia.
Date
23/06/21
Requester(s)
Michelle s22(1)(a)(ii) - irrelevant material - Senior Technical Advisor (TAB/AAT)
Researcher
Jane s22(1)(a)(ii) - irrelev - Research Team Leader (TAB)
Cleared
Please note:
The research and literature reviews col ated by our TAB Research Team are not to be shared external to the Branch. These
are for internal TAB use only and are intended to assist our advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates require further information on
access or planning matters they are to call the TAPS line for advice.
Page 202 of 425
FOI 24/25- 0013
The Research Team are unable to ensure that the information listed below provides an accurate & up-to-date snapshot of
these matters.
The contents of this document are OFFICIAL
1 Contents
2 Summary ......................................................................................................................................... 2
3 What is dialectical behavioural therapy? ........................................................................................ 3
4 Evidence base and effectiveness of dialectical behaviour therapy ................................................ 3
4.1
Other conditions where evidence of effectiveness exists ...................................................... 4
4.2
Dialectical behaviour therapy for the treatment of dissociative identity disorder ................ 4
4.3
Dialectical behaviour therapy for the treatment of autism spectrum disorder ..................... 5
5 What is the general application of DBT? ........................................................................................ 5
6 Available funding options ............................................................................................................... 7
6.1
Public services ......................................................................................................................... 7
6.2
Private services ....................................................................................................................... 7
7 Please provide a list of possible experts in DBT in Australia........................................................... 7
8 References ...................................................................................................................................... 9
2 Summary
• Dialectical Behaviour Therapy (DBT) is the gold standard psychological treatment for
borderline personality disorder (BPD).
• The use of DBT has been suggested as an effective treatment option for the
treatment of Dissociative Identity Disorder (DID). Although no randomised controlled
trials exist, expert consensus and empirical research have found that DBT can be
adapted without significant changes to treat DID given the many similarities to BPD
such as self-harm, suicidal behaviour, emotion dysregulation, identity disturbance,
and dissociation.
• There are no studies to suggest DBT is useful for autism spectrum disorders.
• DBT can be funded through public and private mental health clinics.
• Treatment consists of one on one sessions, group skills training and telephone
coaching sessions.
Page 203 of 425
FOI 24/25- 0013
3 What is dialectical behavioural therapy?
DBT is a type of psychotherapy/talk therapy and a form of cognitive behavioural therapy
(CBT). It was originally designed to treat the problems of chronically suicidal individuals with
BPD. People with this BPD feel intense, uncontrol able emotions, have
troubled relationships and have a disturbed sense of self.
The approach is cal ed "dialectical" because it involves the interaction of two conflicting
ideas, which are that improving the symptoms of BPD involves both acceptance and change
[1].
It is designed to help people change unhelpful ways of thinking and behaving while also
accepting who they are. It helps patients learn to manage emotions by letting them
recognise, experience and accept themselves. DBT can also help patients understand why
they might harm themselves, so they are more likely to change their harmful behaviour.
DBT usual y includes [2]:
• individual sessions with a therapist
• skills training in groups
• telephone coaching sessions with a therapist if you are experiencing a crisis
DBT therapists often work in teams and help each other, so they can provide the best
treatment possible.
A typical course of DBT involves weekly individual therapy sessions (approximately 1 hour),
a weekly group skills training session (approximately 1.5–2.5 hours), and a therapist
consultation team meeting (approximately 1–2 hours) [2].
4 Evidence base and effectiveness of dialectical
behaviour therapy
DBT is currently the gold standard treatment for borderline personality disorder (BPD) and
an effective treatment for associated problems such as repeated self-harming, attempting
suicide, alcohol or drug problems, eat disorders, unstable relationships, depression, feelings
of hopelessness and post-traumatic stress disorder in this population [3]. It has been shown
to reduce the need for medical care and medications by as much as 90% [1].
A Cochrane Review which assessed the beneficial and harmful effects of psychological
therapies for people with BPD was conducted in 2020 [4]. Twenty-four randomised
Page 204 of 425
FOI 24/25- 0013
control ed trials (RCTs) were included that investigated DBT or modified DBT related
treatments.
Compared to treatment as usual (TAU), which includes various forms of psychotherapy,
DBT:
• Reduced BPD symptom severity, self-harm, anger, impulsivity, dissociation and
psychotic-like symptom and improved psychosocial functioning at end of treatment.
o These treatment effects are small to moderate in size, however, the evidence
was graded as low which means there is some uncertainty around the results.
• Did not reduce suicide related outcomes, affective instability, interpersonal
problems, depression or chronic feelings of emptiness compared to TAU.
No adverse effects were found.
Earlier systematic reviews and meta-analyses have come to similar conclusions in relation to
DBT for stabilising self-destructive behaviour, reducing suicide attempts and self-injurious
behaviours in people diagnosed with BPD [5-7].
4.1
Other conditions where evidence of effectiveness exists
• Post-traumatic stress disorder (PTSD) [8, 9]
• Substance abuse and addiction disorders [10, 11]
• Depression [12, 13]
• Eating disorders [14]
4.2
Dialectical behaviour therapy for the treatment of dissociative identity
disorder
Dissociative identity disorder (DID) is a complex post-traumatic disorder which is highly
comorbid with BPD. About two-thirds of people with BPD meet the criteria for a dissociative
disorder, and display features of BPD such as a high degree of suicidality [15-17].
There are no published randomized control ed trials investigating treatments for DID [15].
Empirical data and expert consensus developed by the International Society for the Study of
Trauma and Dissociation suggests that carefully staged trauma-focused psychotherapy can
result in a significant reduction in DID symptomology [18-20].
It has been argued by Foote and Van Orden [15] that DBT can be usefully adapted without
significant changes to treat DID given the many similarities to BPD such as self-harm, suicidal
behaviour, emotion dysregulation, identity disturbance, and dissociation [15].
Page 205 of 425
FOI 24/25- 0013
4.3
Dialectical behaviour therapy for the treatment of autism spectrum
disorder
Simular to DID, autism spectrum disorder (ASD) has overlapping traits with BPD such as
emotional dysregulation, self-harm and social difficulties [21].
Adapting DBT for the treatment of ASD has been suggested by various authors [22, 23].
However, only one non-randomised trial could be located that investigates DBT for ASD
[24]. This included delivering radically open dialectical behaviour therapy (RO DBT) which
has been developed as an adapted form of DBT to directly target over control. The study
showed the intervention was effective, with a medium effect size of 0.53 for improvement
in global distress. Participants with a diagnosis of ASD who completed the therapy had
significantly better outcomes than completing participants without an ASD diagnosis.
A study into the effect of DBT in ASD patients with suicidality and/ or self-destructive
behaviour is currently underway, however, no results have been published [25].
As of 2013,
Asperger’s is now considered part of the autism spectrum and is no longer
diagnosed as a separate condition [26].
5 What is the general application of DBT?
DBT is composed of four elements that the individual and therapist usual y work on over a
year or more [1, 27]:
• Individual DBT therapy, which uses techniques like cognitive restructure and
exposure to change behaviour and improve quality of life.
• Group therapy, which uses skil s training to teach patients how to respond wel to
difficult problems or situations.
• Phone calls, which focus on applying learned skil s to life outside of therapy.
• Weekly consultation meetings among the DBT therapists, which offer a means of
support for the therapists and to ensure they are fol owing the DBT treatment
model.
Some of the strategies and techniques that are used in DBT include:
Core Mindfulness
Page 206 of 425
FOI 24/25- 0013
One important benefit of DBT is the development of mindfulness skil s [28]. Mindfulness
helps to focus on the present or “live in the moment.” Mindfulness skil s help you slow
down and focus on using healthy coping skil s when you are in the midst of emotional pain.
The strategy can also help you stay calm and avoid engaging in automatic negative thought
patterns and impulsive behaviour [27, 28].
Distress Tolerance
Distress tolerance skills help patients to accept oneself and their current situation. There are
four techniques for handling a crisis [27]:
• Distraction
• Improving the moment
• Self-soothing
• Thinking of the pros and cons of not tolerating distress
Distress tolerance techniques help prepare patients for intense emotions and empower
them to cope with a more positive long-term outlook [1].
Interpersonal Effectiveness
Interpersonal effectiveness, at its most basic, refers to the ability to interact with others
[27]. It helps patients to become more assertive in a relationship (for example, expressing
your needs and be able to say "no") while stil keeping a relationship positive and healthy.
Principles include learning to listen and communicate more effectively, deal with
chal enging people, and respect yourself and others [27, 29].
Emotion Regulation
Emotion regulation lets an individual navigate powerful feelings in a more effective way. The
skills learnt will help to identify, name, and change emotions [30].
When an individual is able to recognize and cope with intense negative emotions (for
example, anger), it reduces emotional vulnerability and helps to enable more positive
emotional experiences.
Over the course of treatment, individuals will learn [1, 27]:
•
Acceptance and change: Learn strategies to accept and tolerate life circumstances,
emotions, and yourself. Develop skills that can help you make positive changes in
your behaviours and interactions with others.
•
Behavioural: Learn to analyse problems or destructive behaviour patterns and
replace them with more healthy and effective ones.
•
Cognitive: Focus on changing thoughts, beliefs, behaviours, and actions that are not
effective or helpful.
Page 207 of 425
FOI 24/25- 0013
•
Collaboration: Learn to communicate effectively and work together as a team
(therapist, group therapist, and psychiatrist).
•
Skill sets: Learn new skills to enhance your capabilities.
•
Support: Be encouraged to recognize your positive strengths and attributes and
develop and use them.
6 Available funding options
In most Australian states, DBT programs can be accessed through both the public and
private mental health system [31, 32].
6.1 Public services
Public DBT programs are free to people living in the catchment area of a hospital that offers
a program. A case manager, mental health professional or GP can assist with referral
options.
Depending on the hospital, there may be a waiting time to access the program. Some DBT
programs run continuously across the year, while others operate on a more specific
schedule.
6.2 Private services
Private DBT programs require payment. Prices will vary depending on the specific service
chosen. If you have private health insurance, check that it covers psychiatric admissions.
To join a private DBT program, a psychiatrist from the specific hospital or clinic can provide a
referral.
7 Please provide a list of possible experts in DBT in
Australia
Dr Amanda Johnson (Clinical Psychologist)
Dr Johnson have been trained at Monash University and in the United States at the
University of Denver. Her doctoral thesis evaluated a standard DBT program in a community
health setting over a three year period. She has been involved in the development of several
DBT programs in the public and private sectors in Victoria and providing specialist DBT
supervision, consultation and training.
Email xxxx@xxxxxxxxxxxxxxxxxx.xxx.xx
Ph 03 9530 9777
Dr. Julie King (Clinical Psychologist)
Page 208 of 425
FOI 24/25- 0013
Dr Julie King is a clinical psychologist who offers a range of psychological services. Her
doctorate examined the experience of intel ectual giftedness as asynchrony. She has worked
with the development of youth and antidepressant protocols in general practice. With a
passion for increasing resiliency and coping, Julie is intensively trained in DBT for Borderline
Personality Disorder.
Mob: 0414 432 623
Email: xxxxxxxxxx@xxxxx.xxx
Dr. Lillian Nejad (Clinical Psychologist)
Lillian Nejad, PhD, is a registered and endorsed clinical psychologist with over 20 years of
experience in the assessment and treatment of adults with mild to severe psychological
issues and disorders. She has applied her extensive knowledge and experience in a variety of
settings as a Monash University Lecturer and Clinical Supervisor, as a Senior Psychologist in
public mental health settings, in private practice, and within community and corporate
organisations.
Contact can be made through her website. https://www.drlilliannejad.com/letstalk
Dr. Peter King (Mental Health Nurse; Individual Psychotherapist)
Peter provides education and program development in specialty areas that include
Borderline Personality Disorder, Dialectical Behaviour Therapy, Crisis Intervention,
Psychiatric Emergencies, Somatic Trauma Therapy and Mindfulness-based approaches in
mental health care. Peter has specialist training in CBT, DBT, Somatic Trauma Therapy,
Mindfulness and his Ph.D. explores treatments for individuals with Borderline Personality
Disorder and clinicians’ training needs
xxxxx@xxxx.xxx
Australian DBT Institute: 07 56473438
Page 209 of 425
FOI 24/25- 0013
8 References
1.
May JM, Richardi TM, Barth KS. Dialectical behavior therapy as treatment for borderline
personality disorder. Mental Health Clinician [Internet]. 2016; 6(2):[62-7 pp.]. Available from:
https://doi.org/10.9740/mhc.2016.03.62.
2.
Chapman AL. Dialectical behavior therapy: current indications and unique elements.
Psychiatry (Edgmont) [Internet]. 2006; 3(9):[62-8 pp.]. Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2963469/.
3.
Lieb K, Stoffers J. AS14-01 - Comparative Efficacy of Evidence Based Psychotherapies in the
Treatment of Borderline Personality Disorder. European Psychiatry [Internet]. 2012; 27(S1):[1- pp.].
Available from: https://www.cambridge.org/core/article/as1401-comparative-efficacy-of-evidence-
based-psychotherapies-in-the-treatment-of-borderline-personality-
disorder/F16CED8DCA3E936794AF740F9BD33125.
4.
Storebø OJ, Stoffers-Winterling JM, Völ m BA, Kongerslev MT, Mattivi JT, Jørgensen MS, et
al. Psychological therapies for people with borderline personality disorder. Cochrane Database of
Systematic Reviews [Internet]. 2020; (5). Available from:
https://doi.org//10.1002/14651858.CD012955.pub2.
5.
Panos PT, Jackson JW, Hasan O, Panos A. Meta-Analysis and Systematic Review Assessing the
Efficacy of Dialectical Behavior Therapy (DBT). Research on Social Work Practice [Internet]. 2013
2014/03/01; 24(2):[213-23 pp.]. Available from: https://doi.org/10.1177/1049731513503047.
6.
Kliem S, Kröger C, Kosfelder J. Dialectical behavior therapy for borderline personality
disorder: A meta-analysis using mixed-effects modeling. Journal of Consulting and Clinical
Psychology [Internet]. 2010; 78(6):[936-51 pp.]. Available from: 10.1037/a0021015.
7.
DeCou CR, Comtois KA, Landes SJ. Dialectical Behavior Therapy Is Effective for the Treatment
of Suicidal Behavior: A Meta-Analysis. Behavior Therapy [Internet]. 2019 2019/01/01/; 50(1):[60-72
pp.]. Available from: https://www.sciencedirect.com/science/article/pi /S0005789418300492.
8.
Harned MS, Korslund KE, Linehan MM. A pilot randomized controlled trial of Dialectical
Behavior Therapy with and without the Dialectical Behavior Therapy Prolonged Exposure protocol
for suicidal and self-injuring women with borderline personality disorder and PTSD. Behaviour
Research and Therapy [Internet]. 2014 2014/04/01/; 55:[7-17 pp.]. Available from:
https://www.sciencedirect.com/science/article/pii/S0005796714000151.
9.
Bohus M, Kleindienst N, Hahn C, Mül er-Engelmann M, Ludäscher P, Steil R, et al. Dialectical
Behavior Therapy for Posttraumatic Stress Disorder (DBT-PTSD) Compared With Cognitive Processing
Therapy (CPT) in Complex Presentations of PTSD in Women Survivors of Childhood Abuse: A
Randomized Clinical Trial. JAMA Psychiatry [Internet]. 2020; 77(12):[1235-45 pp.]. Available from:
https://doi.org/10.1001/jamapsychiatry.2020.2148.
10.
van den Bosch LMC, Verheul R, Schippers GM, van den Brink W. Dialectical Behavior Therapy
of borderline patients with and without substance use problems: Implementation and long-term
effects. Addictive Behaviors [Internet]. 2002 2002/11/01/; 27(6):[911-23 pp.]. Available from:
https://www.sciencedirect.com/science/article/pii/S0306460302002939.
11.
Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, et al. Dialectical
behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid
dependent women meeting criteria for borderline personality disorder. Drug and Alcohol
Dependence [Internet]. 2002 2002/06/01/; 67(1):[13-26 pp.]. Available from:
https://www.sciencedirect.com/science/article/pii/S037687160200011X.
Page 210 of 425
FOI 24/25- 0013
12.
Lynch TR, Morse JQ, Mendelson T, Robins CJ. Dialectical Behavior Therapy for Depressed
Older Adults: A Randomized Pilot Study. The American Journal of Geriatric Psychiatry [Internet].
2003 2003/01/01/; 11(1):[33-45 pp.]. Available from:
https://www.sciencedirect.com/science/article/pii/S106474811261238X.
13.
Lynch TR. Treatment of elderly depression with personality disorder comorbidity using
dialectical behavior therapy. Cognitive and Behavioral Practice [Internet]. 2000 2000/09/01/;
7(4):[468-77 pp.]. Available from:
https://www.sciencedirect.com/science/article/pii/S1077722900800589.
14.
Telch CF, Agras, W. S., & Linehan, M. M. Dialectical behavior therapy for binge eating
disorder2001; 69:[1061-5 pp.]. Available from: https://psycnet.apa.org/record/2001-05666-020.
15.
Foote B, Van Orden K. Adapting Dialectical Behavior Therapy for the Treatment of
Dissociative Identity Disorder. American Journal of Psychotherapy [Internet]. 2016 //; 70(4):[343-64
pp.]. Available from:
https://www.ingentaconnect.com/content/afap/ajp/2016/00000070/00000004/art00001.
16.
Ross CA, Ferrell L, Schroeder E. Co-Occurrence of Dissociative Identity Disorder and
Borderline Personality Disorder. Journal of Trauma & Dissociation [Internet]. 2014 2014/01/01;
15(1):[79-90 pp.]. Available from: https://doi.org/10.1080/15299732.2013.834861.
17.
Ross CA. A Proposed Trial of Dialectical Behavior Therapy and Trauma Model Therapy.
Psychological Reports [Internet]. 2005 2005/06/01; 96(3_suppl):[901-11 pp.]. Available from:
https://doi.org/10.2466/pr0.96.3c.901-911.
18.
Brand BL, Loewenstein RJ, Spiegel D. Dispelling Myths About Dissociative Identity Disorder
Treatment: An Empirically Based Approach. Psychiatry: Interpersonal and Biological Processes
[Internet]. 2014 2014/06/01; 77(2):[169-89 pp.]. Available from:
https://doi.org/10.1521/psyc.2014.77.2.169.
19.
Brand BL, Classen CC, McNary SW, Zaveri P. A Review of Dissociative Disorders Treatment
Studies. The Journal of Nervous and Mental Disease [Internet]. 2009; 197(9). Available from:
https://journals.lww.com/jonmd/Fulltext/2009/09000/A Review of Dissociative Disorders Treatm
ent.2.aspx.
20.
International Society for the Study of Trauma and Dissociation. Guidelines for treating
dissociative identity disorder in adults, third revision. J Trauma Dissociation [Internet]. 2011;
12(2):[115-87 pp.].
21.
Dudas RB, Lovejoy C, Cassidy S, Allison C, Smith P, Baron-Cohen S. The overlap between
autistic spectrum conditions and borderline personality disorder. PLoS ONE [Internet]. 2017;
12(9):[e0184447 p.]. Available from: https://doi.org/10.1371/journal.pone.0184447.
22.
Hartmann K, Urbano M, Manser K, Okwara L. Modified Dialectical Behavior Therapy to
Improve Emotion Regulation in Autism Spectrum Disorders. Available from:
https://www.researchgate.net/profile/Kathrin-
Hartmann/publication/317049395 In Autism Spectrum Disorders Modified Dialectical Behavior
Therapy to Improve Emotion Regulation in Autism Spectrum Disorders/links/59230d200f7e9b9
97945b670/In-Autism-Spectrum-Disorders-Modified-Dialectical-Behavior-Therapy-to-Improve-
Emotion-Regulation-in-Autism-Spectrum-Disorders.pdf.
23.
Shkedy G, Shkedy D, Sandoval-Norton AH. Treating self-injurious behaviors in autism
spectrum disorder. Cogent Psychology [Internet]. 2019 2019/01/01; 6(1):[1682766 p.]. Available
from: https://doi.org/10.1080/23311908.2019.1682766.
24.
Cornwall PL, Simpson S, Gibbs C, Morfee V. Evaluation of radically open dialectical behaviour
therapy in an adult community mental health team: effectiveness in people with autism spectrum
disorders. BJPsych Bul etin [Internet]. 2021; 45(3):[146-53 pp.]. Available from:
https://www.cambridge.org/core/article/evaluation-of-radically-open-dialectical-behaviour-therapy-
in-an-adult-community-mental-health-team-effectiveness-in-people-with-autism-spectrum-
disorders/2BC4B0CF8DDBFCDCFD2CD9089545B4D8.
Page 211 of 425
FOI 24/25- 0013
25.
Huntjens A, van den Bosch LMCW, Sizoo B, Kerkhof A, Huibers MJH, van der Gaag M. The
effect of dialectical behaviour therapy in autism spectrum patients with suicidality and/ or self-
destructive behaviour (DIASS): study protocol for a multicentre randomised controlled trial. BMC
Psychiatry [Internet]. 2020 2020/03/17; 20(1):[127 p.]. Available from:
https://doi.org/10.1186/s12888-020-02531-1.
26.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders
(DSM-5®): American Psychiatric Pub; 2013.
27.
Schimelpfening N. What Is Dialectical Behavior Therapy (DBT)? 2021 [Available from:
https://www.verywellmind.com/dialectical-behavior-therapy-1067402.
28.
Feliu-Soler A, Pascual JC, Borràs X, Portella MJ, Martín-Blanco A, Armario A, et al. Effects of
Dialectical Behaviour Therapy-Mindfulness Training on Emotional Reactivity in Borderline Personality
Disorder: Preliminary Results. Clinical Psychology & Psychotherapy [Internet]. 2014 2014/07/01;
21(4):[363-70 pp.]. Available from: https://doi.org/10.1002/cpp.1837.
29.
Lenz AS, Del Conte G, Hollenbaugh KM, Callendar K. Emotional Regulation and Interpersonal
Effectiveness as Mechanisms of Change for Treatment Outcomes Within a DBT Program for
Adolescents. Counseling Outcome Research and Evaluation [Internet]. 2016 2016/12/01; 7(2):[73-85
pp.]. Available from: https://doi.org/10.1177/2150137816642439.
30.
Goodman M, Carpenter D, Tang CY, Goldstein KE, Avedon J, Fernandez N, et al. Dialectical
behavior therapy alters emotion regulation and amygdala activity in patients with borderline
personality disorder. Journal of Psychiatric Research [Internet]. 2014 2014/10/01/; 57:[108-16 pp.].
Available from: https://www.sciencedirect.com/science/article/pii/S0022395614001952.
31.
SANE Australia. Fact Sheet: Dialectical behaviour therapy (DBT) 2017 [Available from:
https://www.sane.org/information-stories/facts-and-guides/dialectical-behaviour-therapy-dbt.
32.
Australian Borderline Personality Foundation Limited. How to access treatment ND
[Available from: https://bpdfoundation.org.au/how-to-access-treatment.php.
Page 212 of 425
FOI 24/25- 0013
DOCUMENT 22
1. Research – Exposure Therapy for PTSD
Exposure Therapy - Data on its efficacy in treating PTSD. Is it the
optimal treatment? Comparative data on the efficacy of other evidence
Brief
based treatments for PTSD, specifically trauma-focussed cognitive
behavioural therapy (CBT) and eye movement desensitisation and
reprocessing (EMDR).
Date
16/08/21
Requester(s) Jenni s22(1)(a)(ii)
- irreleva - Senior Technical Advisor (TAB/AAT)
Researcher
Maddie s22(1)(a)(ii) (
- irrele
and
Aaron s22(1)(a)(ii)
)
- irrelevant m
Cleared
Please note:
The research and literature reviews col ated by our TAB Research Team are not to be shared external to the
Branch. These are for internal TAB use only and are intended to assist our advisors with their reasonable and
necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates require further
information on access or planning matters they are to call the TAPS line for advice.
The Research Team are unable to ensure that the information listed below provides an accurate & up-to-date
snapshot of these matters.
The content of this document is OFFICIAL.
1 Contents
2 Summary ....................................................................................................................... 2
3 What is Post-Traumatic Stress Disorder (PTSD)? .......................................................... 2
4 Clinical Presentation ...................................................................................................... 3
5 Therapeutic treatment options ........................................................................................ 4
5.1
Exposure ................................................................................................................ 4
6 Efficacy of PTSD therapies ............................................................................................ 4
7 References .................................................................................................................... 5
Page 213 of 425
FOI 24/25- 0013
2 Summary
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop in
response to exposure to an event that threatens or is perceived to threaten a person’s life or
safety [1, 13]. This can include a serious accident, natural disaster or sexual assault.
People with PTSD can have intense intrusive thoughts such as flashbacks or distressing
dreams related to their traumatic experience lasting for months or years. PTSD is associated
with significant impacts to functioning and quality of life.
Trauma Focused Cognitive Behavioural Therapy (TF-CBT) is well-establish as an acute
treatment for PTSD. Several variants of TF-CBT are strongly recommended treatment
options. These include prolonged exposure therapy, cognitive therapy, cognitive processing
therapy and Eye Movement Desensitisation Reprocessing (EMDR) therapy.
Prolonged Exposure therapy or variants of TF-CBT that have a component of exposure are
preferred on slight weight of evidence for long term symptom reduction. Prolonged Exposure
therapy has been shown to be a highly effective method for reducing PTSD symptoms in
both the short-term and long-term.
3 What is Post-Traumatic Stress Disorder?
PTSD is a mental health condition that can develop in response to exposure to an event that
threatens or is perceived to threaten a person’s life or safety [1, 13].
PTSD can present in different ways but often involves intense intrusive thoughts and feelings
related to the traumatic experience. This can include vivid flashbacks, distressing dreams, or
repeated involuntary memories of the trauma. People with PTSD often avoid people, places
or situations which remind them of the traumatic event. PTSD also results in alterations to
cognition and mood such as memory loss or a persistent negative emotional state. It can
also cause other symptoms such as irritable behaviour, hypervigilance and issues with
concentration [1].
Symptoms usually appear within the first 3 months from exposure to trauma, however a
person may not experience symptoms until years after the traumatic event occurred.
Duration of the symptoms varies, with half of adults recovering within 3 months of developing
symptoms, but some experiencing symptoms for more than 50 years. The severity of
symptoms can vary over time. Many people experience more symptoms during stressful
periods or when they are exposed to reminders of their trauma [1].
PTSD is associated with significant impacts to functioning and quality of life. It can affect
relationships with friends and family, performance at work and can result in a reduction in
engagement in activities a person previously found rewarding [2].
PTSD has an estimated lifetime prevalence of 1.3% - 12.2% depending on social
background and country of residence [3]. Higher rates of PTSD have been documented
among women, younger people, and people who are socially disadvantaged [4]. People in
occupations that are more likely to expose them to traumatic events (for example,
emergency services, healthcare works and military personnel) are more likely to develop
PTSD [3, 5].
More than 50% of people with PTSD also have other mental health disorders, most
commonly depression, bipolar disorder, anxiety, or substance use disorders [6].
Page 214 of 425
FOI 24/25- 0013
4 Clinical Presentation
The first characteristic of PTSD is that the person has witnessed or experienced a major
traumatic event [1]. This includes:
• directly experiencing the traumatic event(s)
• witnessing the traumatic event(s) in person
• learning about the traumatic event(s) which occurred to a close family member or
friend
• experiencing repeated exposure to details of traumatic event(s) (for example police
officers repeatedly exposed to details of child abuse).
Secondly, the person will have symptoms from each of the four PTSD symptom categories,
with the symptoms lasting for at least one month [1].
1.
Intrusion: at least one of the following symptoms
• Intrusive distressing memories
• Recurrent distressing dreams
• Flashbacks of the traumatic event
• Intense or prolonged psychological distress at exposure to reminders of the
trauma
• Physiological reactions to cues resembling an aspect of the traumatic event
2.
Avoidance: at least one of the following symptoms
• Avoiding places, people, objects and situations that may trigger distressing
memories
• Avoiding remembering or thinking about the traumatic event
3.
Alterations in cognition and mood: at least two of the following symptoms
• Inability to remember important aspects of the traumatic event
• Persistent negative thoughts about themselves or the world
• Distorted thoughts about the cause or consequences of the traumatic event
• Persistent negative emotional state
• Loss of interest in activities
• Persistent inability to experience positive emotions
• Feeling detached or estranged from other people
4.
Alterations in arousal and reactivity: at least two of the following symptoms
• Irritable behaviour and angry outbursts
• Reckless/self-destructive behaviour
• Hypervigilance
• Exaggerated startle response
• Issues with concentration
• Sleep disturbance
Individuals with PTSD can exhibit any combination of these symptoms.
Symptoms usually appear within the first 3 months from exposure to trauma, however a
person may not experience these symptoms until years after the traumatic event occurred.
Page 215 of 425
FOI 24/25- 0013
5 Therapeutic treatment options
TF-CBT is the generally recommended therapeutic treatment option for PTSD [4, 10].
Cognitive behavioural therapy (CBT) is a broad category of therapies used to treat mental
health disorders based on principles of learning and cognition. For people with PTSD, TF-
CBT is commonly used, which specifically addresses the impact of a traumatic event.
There are several variants of TF-CBT. However, there is a lack of consensus about what
therapies count as components or variants. TF-CBT can include development of coping
strategies, prolonged exposure therapy, narrative exposure therapy, cognitive processing
therapy, cognitive restructuring and EMDR [4, 7, 8, 14]. There is considerable overlap
between dif erent variants of cognitive behavioural therapy and they may be used together
[14]. While the variants of TF-CBT are often treated separately for research purposes, “they
all essentially comprise emotional processing of the traumatic memory and integration of
new corrective information” [4].
5.1
Use of exposure in TF-CBT Exposure is a therapeutic technique used in varieties of cognitive behavioural therapy. It is
used for many different mental health disorders, including PTSD. Prolonged exposure
therapy is a form of cognitive behavioural therapy which requires the patient to repeatedly
confront distressing stimuli associated with their trauma under the guidance of a mental
health professional, with the aim of extinguishing the conditioned emotional response to the
traumatic stimuli [7]. This can include exposure through imagination, by describing to the
patient scenes or mental imagery related to the traumatic event, or exposure to real-life
stimuli associated with the traumatic event. Prolonged exposure therapy is typically
conducted once or twice per week for 8-12 weeks in 60-90 minute sessions [7]. Some trials
show effectiveness of the treatment at 40-60 minute sessions or even 10-20 minute sessions
[4].
Other forms of TF-CBT such as Cognitive Processing Therapy and Cognitive Therapy focus
more on changing problematic beliefs and cognitive patterns [10].
Narrative exposure therapy is based on exposure therapy and testimony therapy. It involves
the
patient developing a chronological narrative of their entire life under the guidance of a
mental health professional with a focus on retelling their traumatic experience(s). Narrative
exposure therapy is tailored to experiences of war and torture [7].
There is some reason to also treat EMDR as a variant of exposure therapy [15], though it is
also often treated separately [7]. EDMR is a treatment for a variety of mental health
disorders including PTSD. In EDMR a patient is encouraged to momentarily think about their
trauma while the practitioner stimulates eye movements with the aim of desensitising the
patient to their trauma. In EDMR the patient may not have to return to the traumatic
experience for prolonged periods of time [9].
6 Efficacy of PTSD therapies
TF-CBT is well-establish as an acute treatment for PTSD. There is also evidence of long
term efficacy of TF-CBT. However, there is no unequivocal evidence for the preference of
any particular variant of TF-CBT as a frontline treatment option. Klein et al. find that
Page 216 of 425
FOI 24/25- 0013
exposure therapies have considerably larger effect sizes in the long term [10]. They
conclude:
Exposure-focused therapies, with the principal ingredient often being imaginal
exposure, demonstrated the most robust continued improvement following treatment,
yet it is meaningful that al of the broad range of trauma-focused treatments included
in the meta-analysis produced lasting gains. [10 §4]
Prolonged Exposure Therapy, Cognitive Therapy, and Cognitive Processing Therapy are all
strongly recommended by the Australian Guidelines for the Prevention and Treatment of
Acute Stress Disorder, Posttraumatic Stress Disorder and Complex PTSD [8] and by the
American Psychological Association [16]. EMDR is strongly recommended by the Australian
Guidelines for the Prevention and Treatment of Acute Stress Disorder, Posttraumatic Stress
Disorder and Complex PTSD [8] and conditionally recommended by the American
Psychological Association [16]. Exposure is a recommended component in most treatment
guidelines [4, 8, 16].
A meta-analysis of psychological treatments for adults with PTSD from 64 randomised
control trials determined that prolonged exposure therapy had the highest strength of
evidence for reducing PTSD symptoms [7]. The high efficacy of prolonged exposure therapy
has also been supported by further meta-analyses, with exposure-based treatments showing
stronger long-term improvement in PTSD symptoms relative to TF-CBT without exposure
[10].
There is stronger evidence supporting the efficacy of prolonged exposure therapy than
narrative exposure therapy [7]. Narrative exposure therapy is generally only recommended
for adults whose trauma is related to genocide, civil conflict, political detention, or
displacement [8].
Narrative exposure therapy and CBT-mixed therapies (therapies that used many
components of CBT) were found to have moderate evidence for reducing PTSD symptoms
[7].
A 2015 meta-analysis found then current research into EMDR to have low strength of
evidence for reducing PTSD symptoms but moderate strength of evidence for loss of PTSD
diagnosis and improving depression symptoms [7]. A 2018 meta-analysis found efficacy of
EMDR at the acute stage does not significantly differ from other variants of TF-CBT [10].
Despite the evidence supporting prolonged exposure therapy, there has been some
question as to whether exposure therapy in isolation is an ef ective treatment for PTSD.
Some argue that exposure therapy alone does not address all of the symptoms of PTSD and
should be used alongside other treatments [11]. Additionally, practitioners often fear high
drop-out rates due to the distressing nature of exposure-based therapies, however evidence
suggests that the drop-out rate for exposure therapies are no dif erent from other therapies
used to treat PTSD [12].
7 References
1.
American Psychiatric Association. Post raumatic Stress Disorder. In: Diagnostic and
statistical manual of mental disorders, fifth edition. Arlington, VA, American Psychiatric
Association. 2013. p. 271-280.
Page 217 of 425
FOI 24/25- 0013
2.
Forbes D, Nickerson A, Bryant RA, Creamer M, Silove D, McFarlane AC, Van Hooff
M, Phelps A, Felmingham KL, Malhi GS, Steel Z. The impact of post-traumatic stress disorder
symptomatology on quality of life: the sentinel experience of anger, hypervigilance and
restricted affect. Australian & New Zealand Journal of Psychiatry. 2019 Apr;53(4):336-49.
3.
Shalev A, Liberzon I, Marmar C. Post-traumatic stress disorder. New England Journal
of Medicine. 2017 Jun 22;376(25):2459-69.
4.
Bryant RA. Post‐traumatic stress disorder: a state‐of‐the‐art review of evidence and
challenges. World Psychiatry. 2019 Oct;18(3):259-69.
5.
Lee W, Lee YR, Yoon JH, Lee HJ, Kang MY. Occupational post-traumatic stress
disorder: an updated systematic review. BMC public health. 2020 Dec;20:1-2.
6.
Rytwinski NK, Scur MD, Feeny NC, Youngstrom EA. The co‐occurrence of major
depressive disorder among individuals with posttraumatic stress disorder: A meta‐analysis.
Journal of traumatic stress. 2013 Jun;26(3):299-309.
7.
Cusack K, Jonas DE, Forneris CA, Wines C, Sonis J, Middleton JC, Feltner C,
Brownley KA, Olmsted KR, Greenblatt A, Weil A. Psychological treatments for adults with
posttraumatic stress disorder: A systematic review and meta-analysis. Clinical psychology
review. 2016 Feb 1;43:128-41.
8.
Phoenix Australia. Treatment Recommendations. In: Australian Guidelines for the
Prevention and Treatment of Acute Stress Disorder, Post raumatic Stress Disorder and
Complex PTSD [Internet]. Carlton (VIC ;2020 Jul.) Available from: Chapter-6.-Treatment-
recommendations.pdf (phoenixaustralia.org)
9.
De Haan KL, Lee CW, Fassbinder E, Van Es SM, Menninga S, Meewisse ML,
Rijkeboer M, Kousemaker M, Arntz A. Imagery rescripting and eye movement desensitisation
and reprocessing as treatment for adults with post-traumatic stress disorder from childhood
trauma: randomised clinical trial. The British Journal of Psychiatry. 2020 Nov; 217(5):609-15.
10. Kline AC, Cooper AA, Rytwinksi NK, Feeny NC. Long-term efficacy of psychotherapy
for posttraumatic stress disorder: A meta-analysis of randomized controlled trials. Clinical
psychology review. 2018 Feb 1;59:30-40.
11. Markowitz S, Fanselow M. Exposure therapy for post-traumatic stress disorder: factors
of limited success and possible alternative treatment. Brain sciences. 2020 Mar;10(3):167.
12. Paintain E, Cassidy S. First‐line therapy for post‐traumatic stress disorder: A
systematic review of cognitive behavioural therapy and psychodynamic approaches.
Counselling and psychotherapy research. 2018 Sep;18(3):237-50.
13.
Australian Government Australian Institute of Health and Welfare,
Australia's Health:
Glossary, [website], https:/ www.aihw.gov.au/reports-data/australias-health/australias-health-
snapshots/glossary, (accessed 31 August 2021).
14.
Institute of Medicine 2008. Evidence and Conclusions: Psychotherapy. In, Treatment
of Post raumatic Stress Disorder: An Assessment of the Evidence. Washington, DC: The
National Academies Press.
Page 218 of 425
FOI 24/25- 0013
15.
Society of Clinical Psychology,
American Psychological Association Division 12,
[website], https://div12.org/treatment/eye-movement-desensitization-and-reprocessing-for-
post-traumatic-stress-disorder, (accessed 31 August 2021).
16.
American Psychological Association, Clinical Practice Guideline for the treatment of
Posttraumatic Stress Disorder, [website], https://www.apa.org/ptsd-
guideline/treatments/index, (accessed 31 August 2021).
Page 219 of 425
FOI 24/25- 0013
DOCUMENT 23
Ratios of support
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be
shared external to the Branch. These are for internal TAB use only and are intended to
assist our advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If
Delegates require further information on access or planning matters they are to call the
TAPS line for advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters.
Research question: Is there research (national and international) available that can inform
best practice in applying Ratios of Support to participant care in group programs and
supported employment? Are there guidelines available in other insurance type schemes
(national and international)?
Date: 14/12/2021
Requestor: Tiffany s22(1)(a)(ii)
- irre
Request endorsed by (EL1): Jane s22(1)(a)(ii) - irrelev
Cleared by: Illya s22(1)(a)(ii) - irreleva
1. Contents
Ratios of support ........................................................................................................................ 1
1.
Contents ....................................................................................................................... 1
2.
Summary ...................................................................................................................... 2
3.
Assessment Tools ......................................................................................................... 2
4.
Guidelines ..................................................................................................................... 5
5.
Factors that can influence ratios of support .................................................................. 6
5.1 Manual Handling ........................................................................................................ 7
5.2 Behaviours of concern ............................................................................................... 8
6.
Social service analogues .............................................................................................. 8
7.
Appendix – Correspondence ........................................................................................ 9
Page 220 of 425
FOI 24/25- 0013
7.1
............................ 11
s22(1)(a)(ii) - irrelevant material
7.2
............................ 11
7.3
............................ 12
7.4
............................ 13
7.5
............................ 16
7.6
............................ 17
7.7 NDIS Quality and Safeguards Commission researchers ......................................... 17
8.
References ................................................................................................................. 19
9.
Version control ............................................................................................................ 21
2. Summary
Occupational Therapists (OT) use clinical judgement in determining ratios of support required
by clients for employment, community and social activities. OTs appeal to a wide variety of
considerations covering personal, environmental and institutional factors. No guidelines have
been developed by any organisation that offer clear guidance or rules for determining ratios of
support. Different assessment tools are used to inform clinical decision making depending on
the individual circumstances of the person requiring support.
3. Assessment Tools
Members of Occupational Therapy Australia (OTA) advised that the types of assessments they
use to assist with determining support ratios varies between participants. OTs employ their
clinical reasoning in determining which assessment tool wil provide the best information.
Some tools and strategies that were mentioned include:
• informal interview and history taking
• observing and analysing skil s of formal and informal supports
• Overt Behaviour Scale
• manual handling plans
• observing rosters and scheduling
• Care and Needs Scale
• Community Integration Questionnaire s22(1)(a)(ii) - irrelevant material.
Previous research completed by the TAB Research Team in March 2021 identifies one
systematic review noting that only two assessment tools have been used for both
individualised support planning and resource allocation. They are the
Support Intensity Scale
Page 221 of 425
FOI 24/25- 0013
(SIS) and the
Instrument for the Classification and Assessment of Support Needs (I-
CAN) [1,2,3,4]. These two scales are the most widely researched support needs assessment
scales [2]. Both are in use in Australia [2,5]. I-CANS is based on the World Health
Organisation’s International Classification of Functioning, Disability, and Health. SIS uses the
American Association on Intellectual and Developmental Disabilities functioning model [2].
The SIS records frequency, duration and type of support required for specific activities. The
assessor rates activities according to the following scales:
FREQUENCY – How frequently is support needed for this activity?
0 = none or less than monthly
1 = at least once a month, but not once a week
2 = at least once a week, but not once a day
3 = at least once a day, but not once an hour
4 = hourly or more frequently
DAILY SUPPORT TIME – On a typical day when support in this area is needed, how
much time should be devoted?
0 = none
1 = less than 30 minutes
2 = 30 minutes to less than 2 hours
3 = 2 hours to less than 4 hours
4 = 4 hours or more
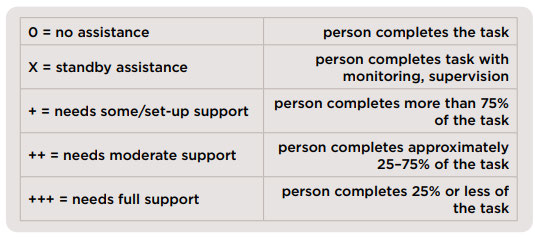
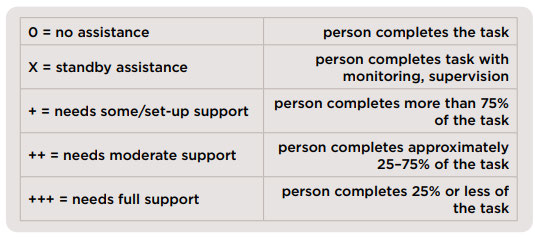
TYPES OF SUPPORT: What kind of support should be provided?
0 = none
1 = monitoring
2 = verbal/gestural prompting
3 = partial physical assistance
4 = full physical assistance [6].
The I-CAN records frequency and type of support required on a scale of 0 – 5 to then calculate
intensity of supports required:
FREQUENCY – how often support is needed
5 = Continuously
4 = Frequently
3 = Daily
Page 222 of 425
FOI 24/25- 0013
2 = Weekly
1 = Occasionally
0 = Never
TYPE – how much support is needed
5 = Pervasive
4 = Extensive
3 = Moderate
2 = Minor
1 = Managed
0 = Independent
COMBINED SUPPORT INTENSITY – sum of
Frequency and
Type scores
10 = Continuous / Pervasive
8 = Frequent/ Extensive
6 = Daily / Moderate
4 = Weekly / Minor
2 = Occasionally / Managed
0 = No support [7].
Paying particular attention to the
Type scores in both assessment scales, a suitably qualified
clinician may be able to interpret these scores in such a way as to suggest ratios of support or
at least suggest something about possible ratios of support. For example, a person with a SIS
Type score of 1 or 2 (monitoring, verbal/gestural prompting) for community access or
employment activities may thrive with a higher ratio environment compared to a person with a
SIS score of 4 (full physical assistance). Similarly, a person with an I-CAN
Type score of 1 or 2
(managed, minor) may benefit from group social activities with a shared support worker while a
person with a score of 4 or 5 (extensive, pervasive) may require direct individual support at a
1:1 or 2:1 ratio. However, the assessment tools do not specifically recommend ratios of
support and any conclusions about ratios would be significantly based on clinician’s expertise
or judgement.
It is also worth noting that these assessment tools do not determine support needs but are
based on the assessor’s observations of support needs. Both tools record support needs
based on the assessor’s understanding and then quantify and aggregate scores to indicate
overall support needs. In that sense, the contribution of these assessment tools to determining
ratios of support may be limited.
Page 223 of 425
FOI 24/25- 0013
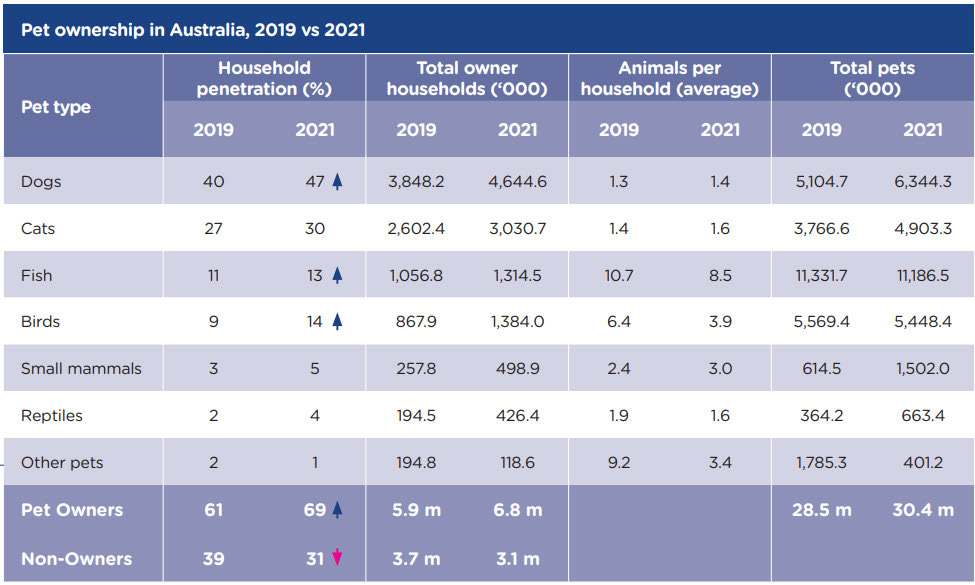
4. Guidelines
Previous research completed by the TAB Research Team in March 2021 states that there are
no available professional or governmental guidelines that can be used to support determining
personal care hours required for a range of tasks, disabilities and severity levels [1].
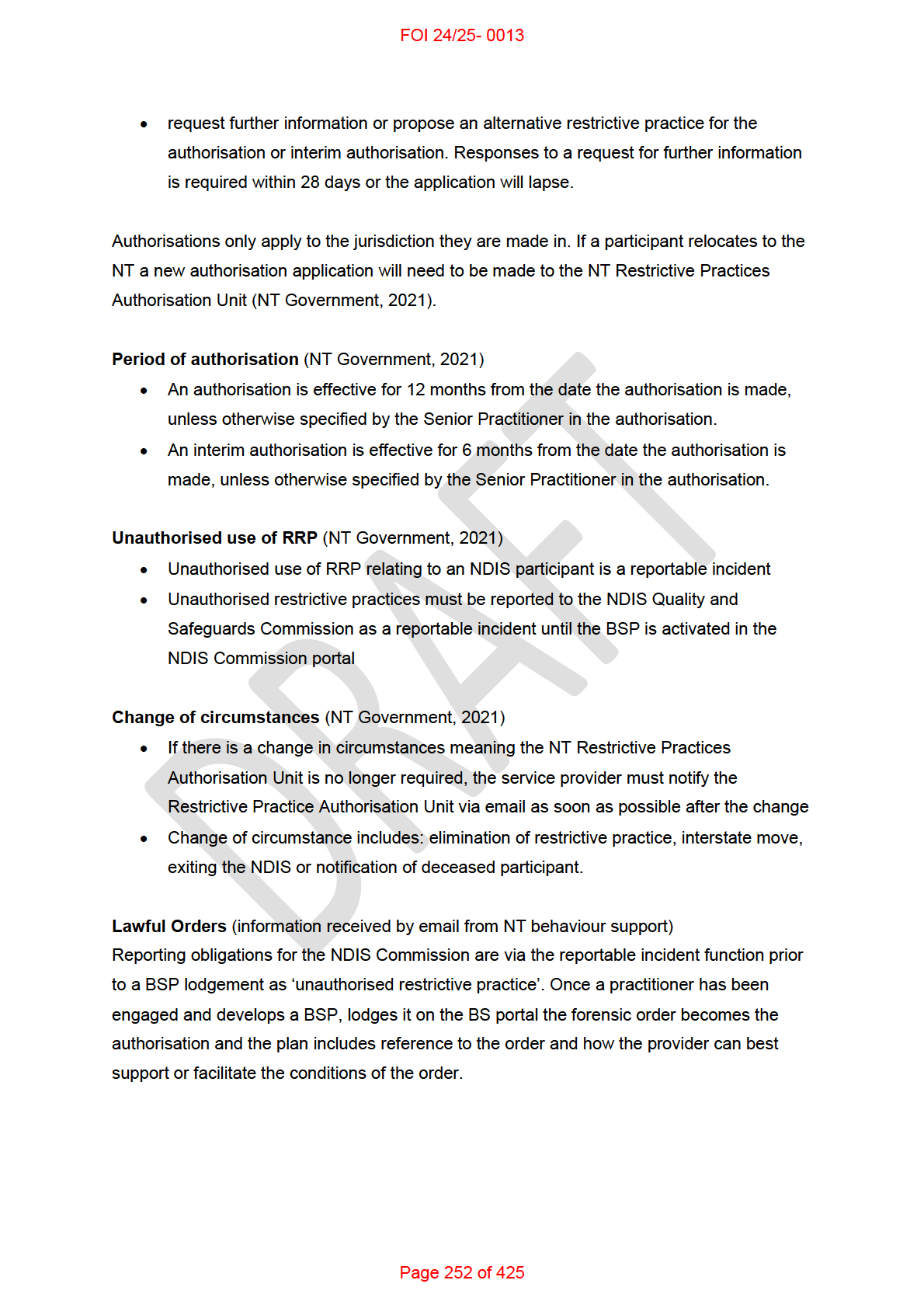
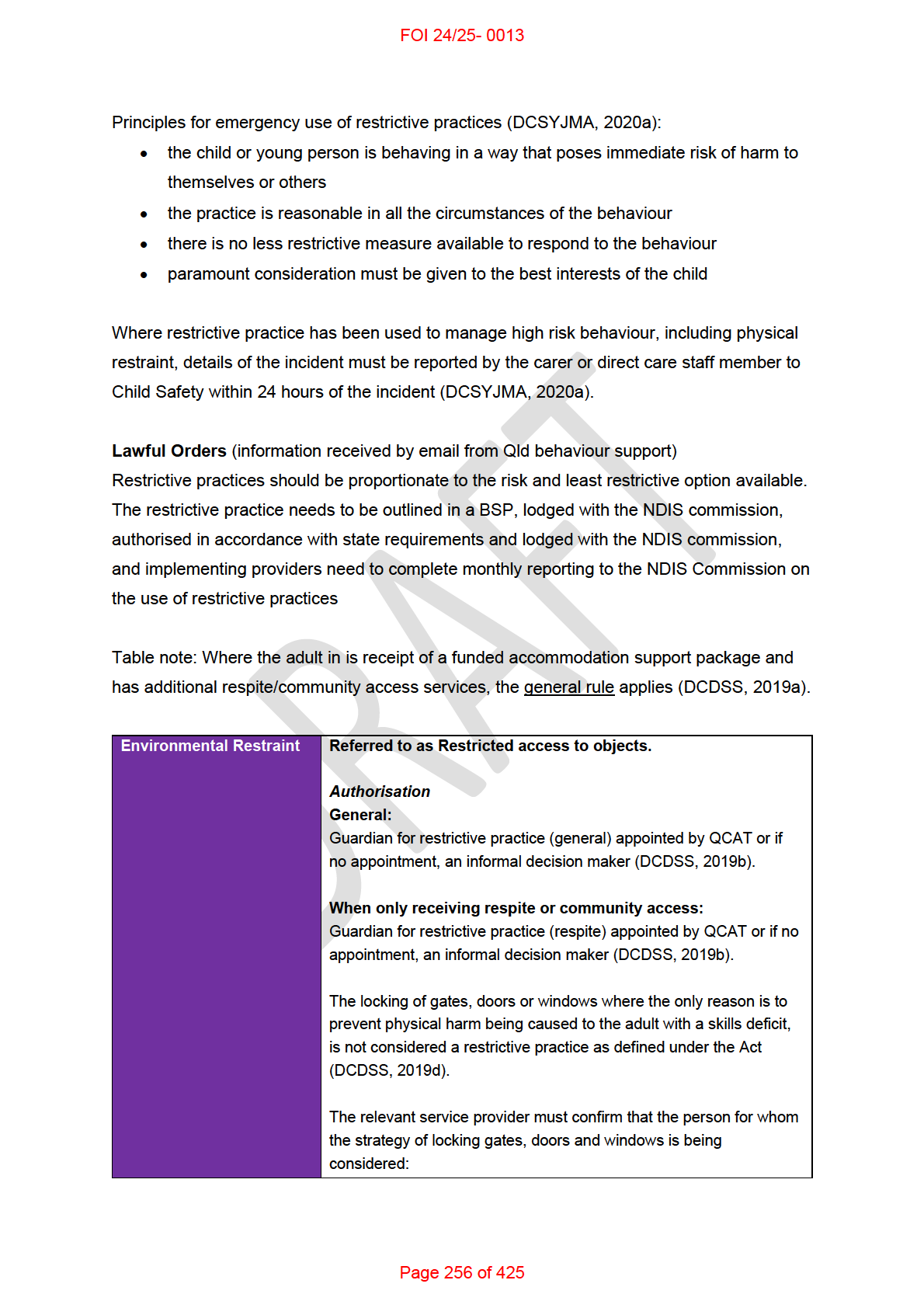
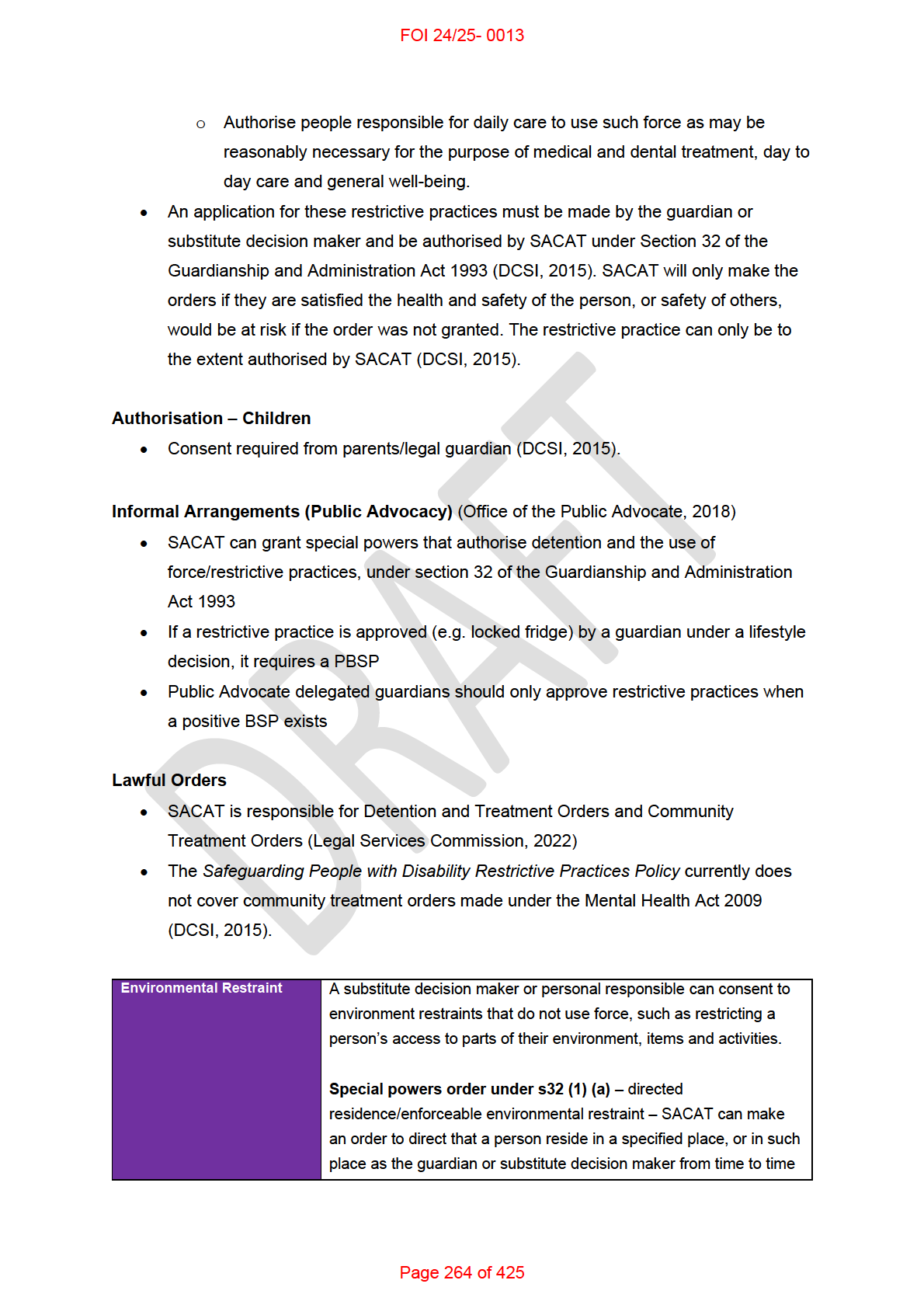
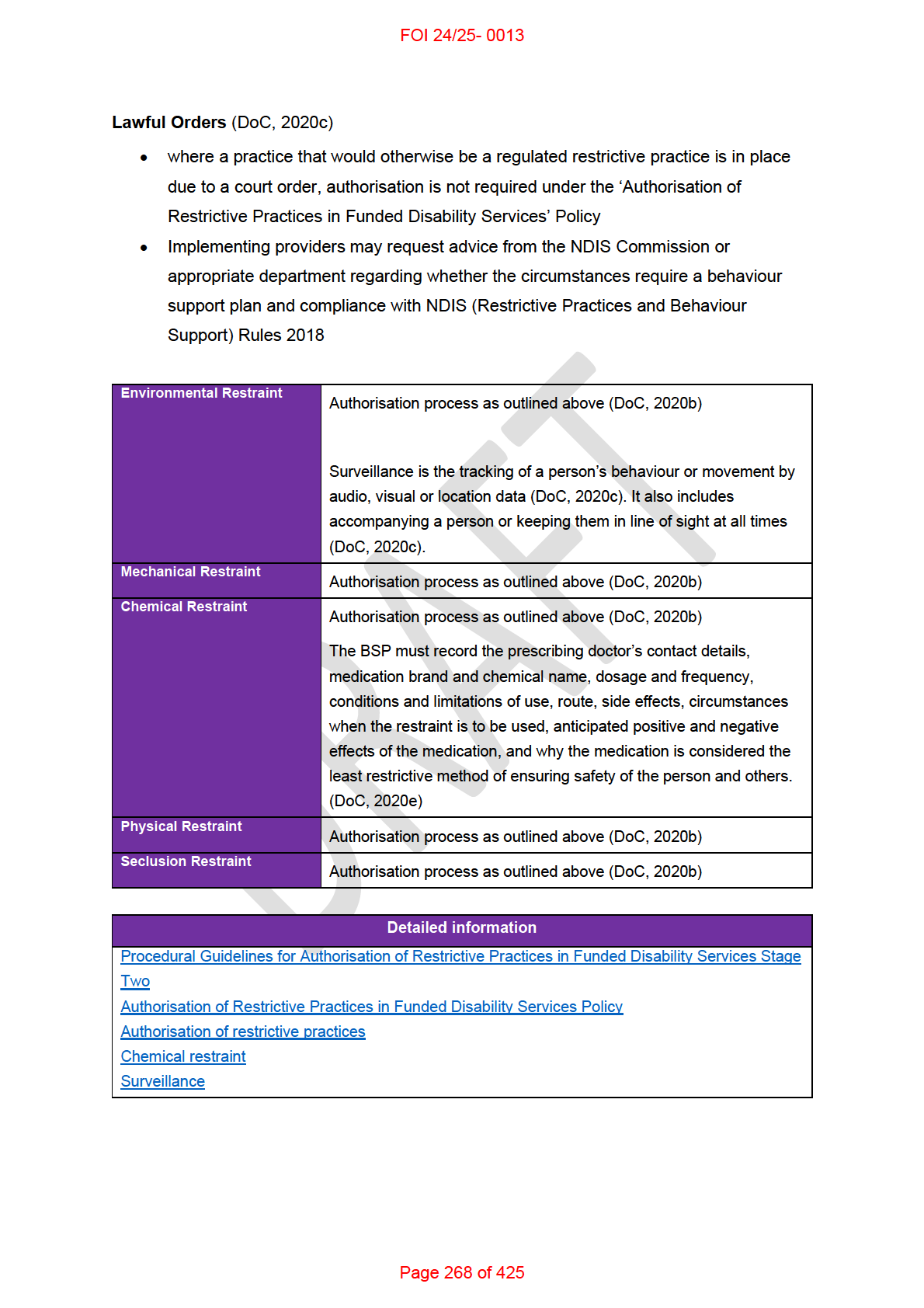
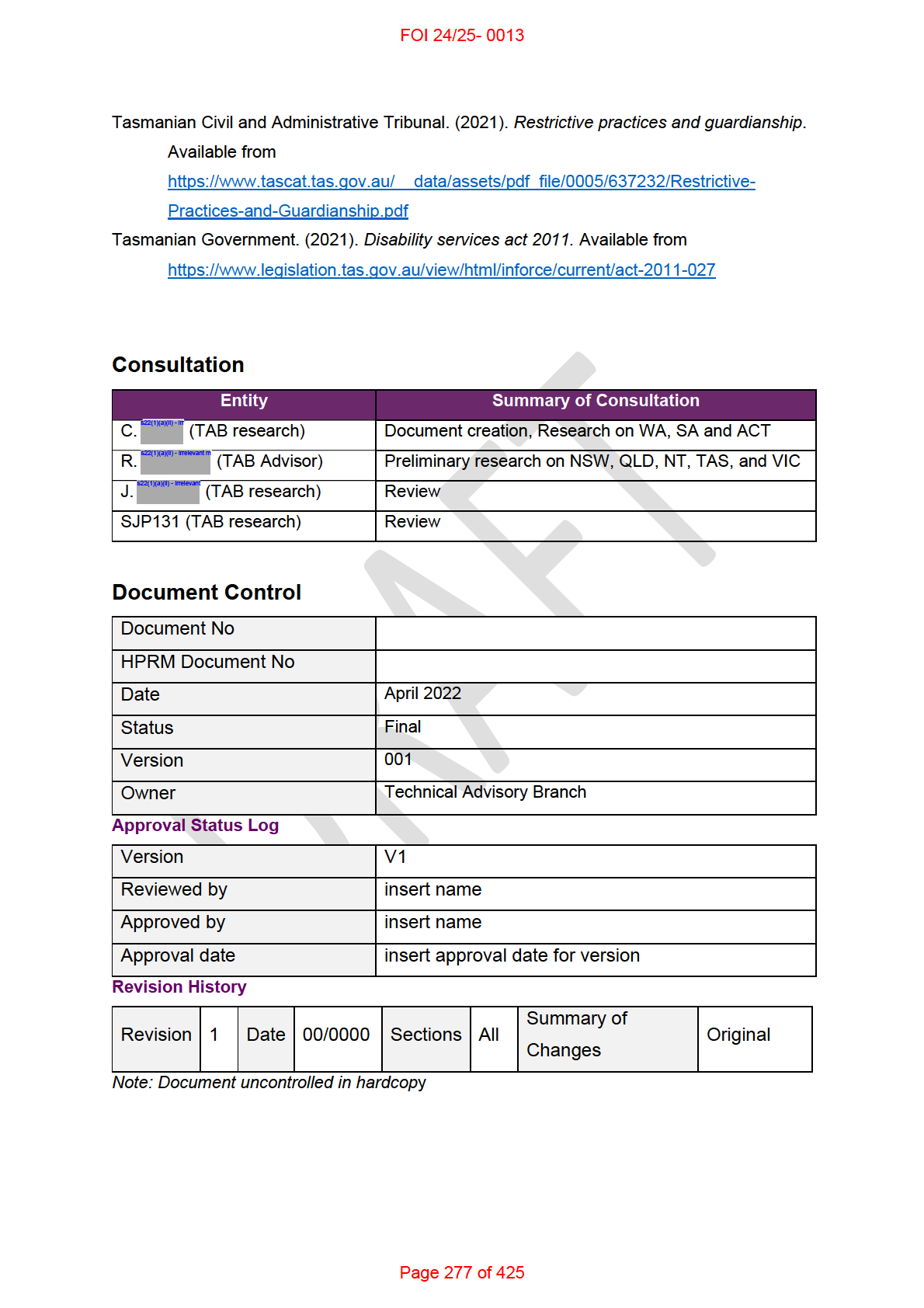
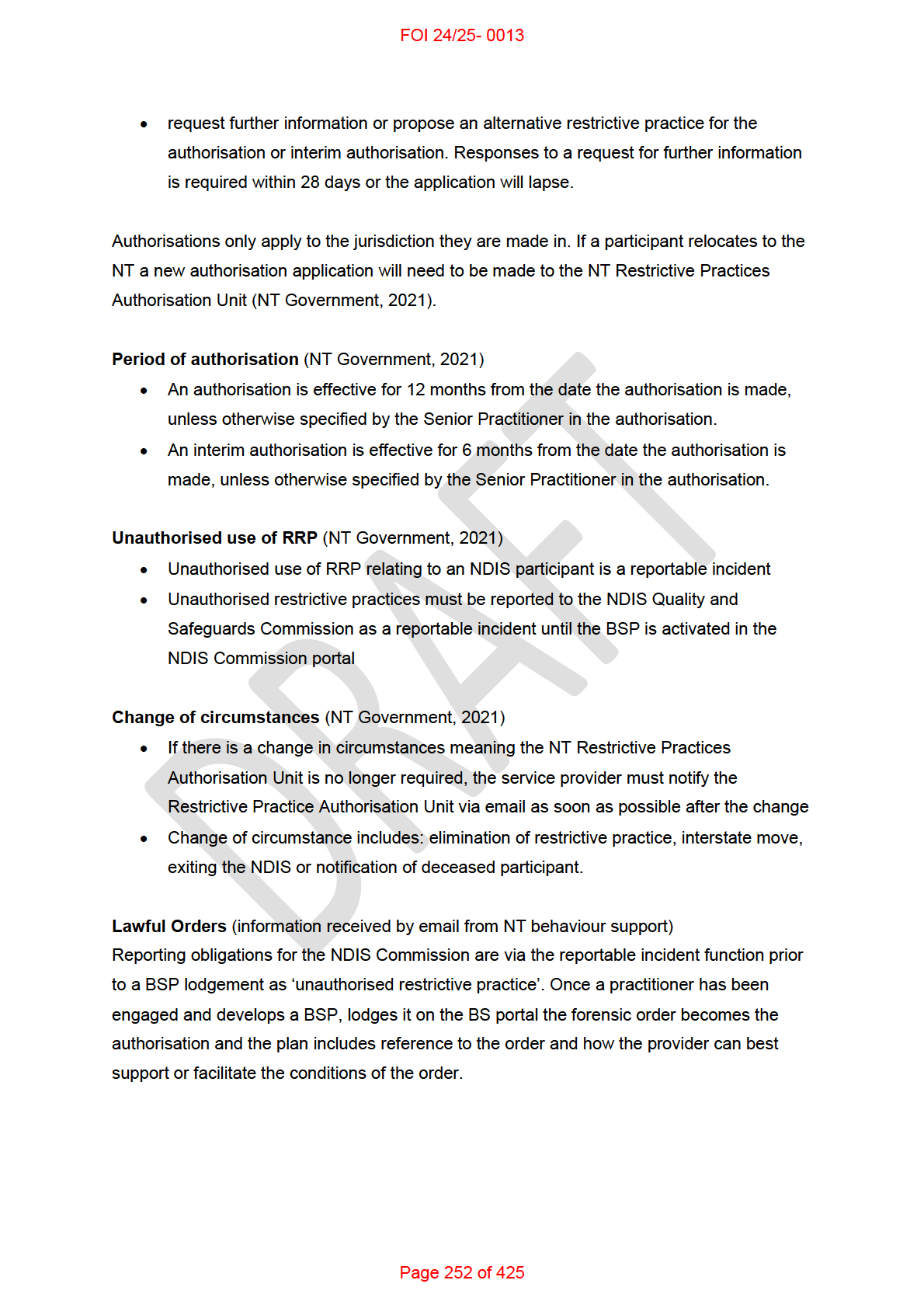
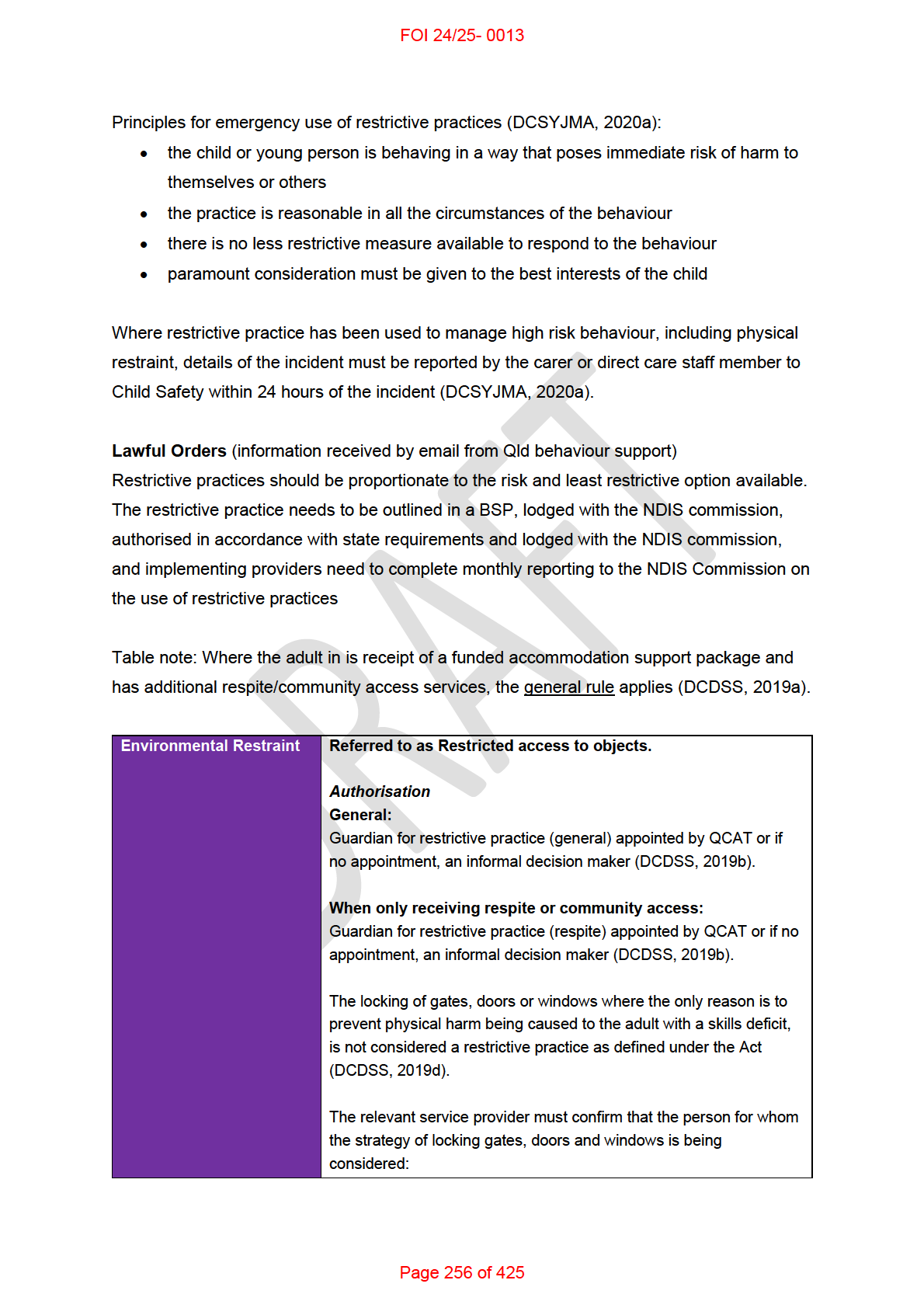
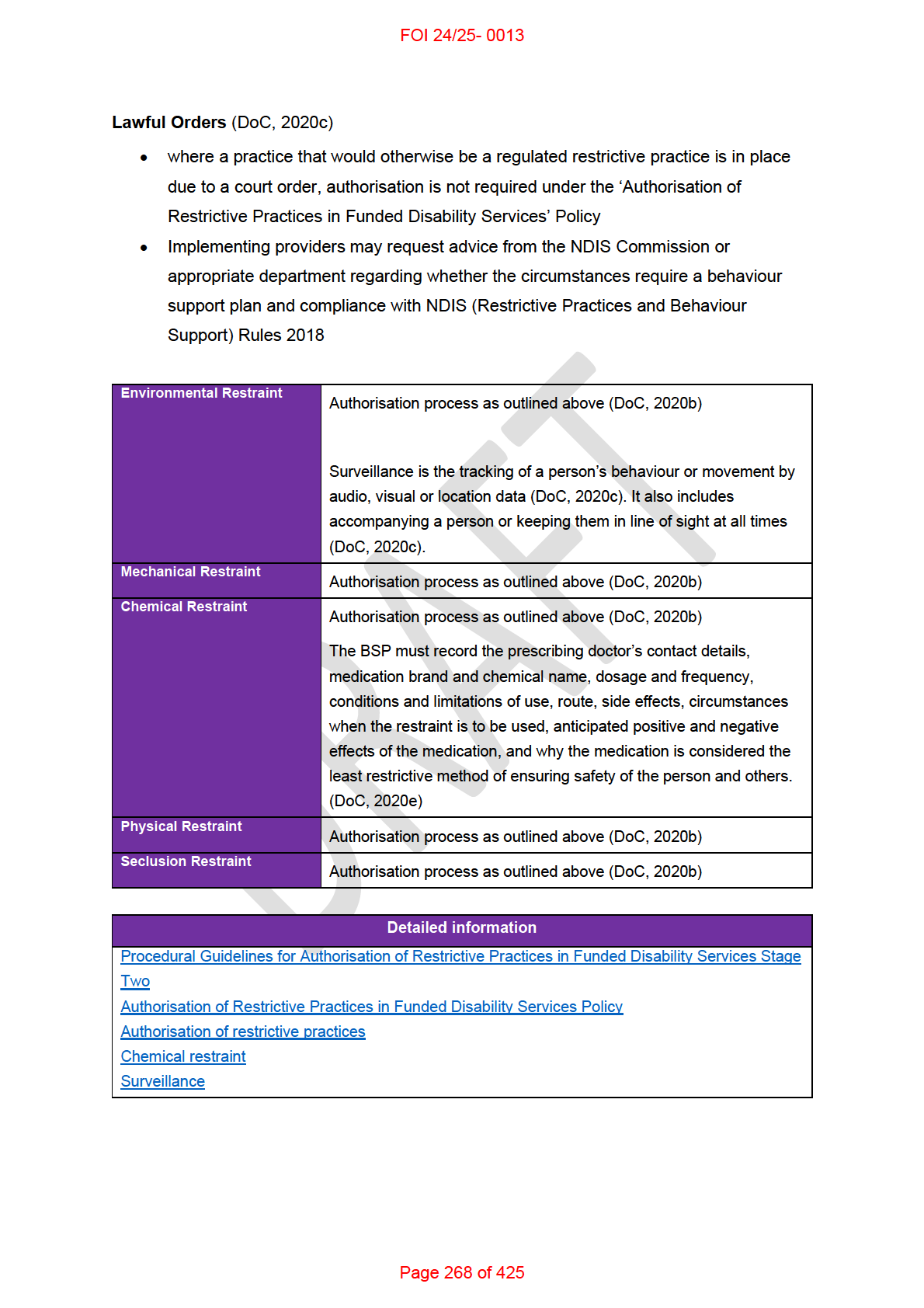
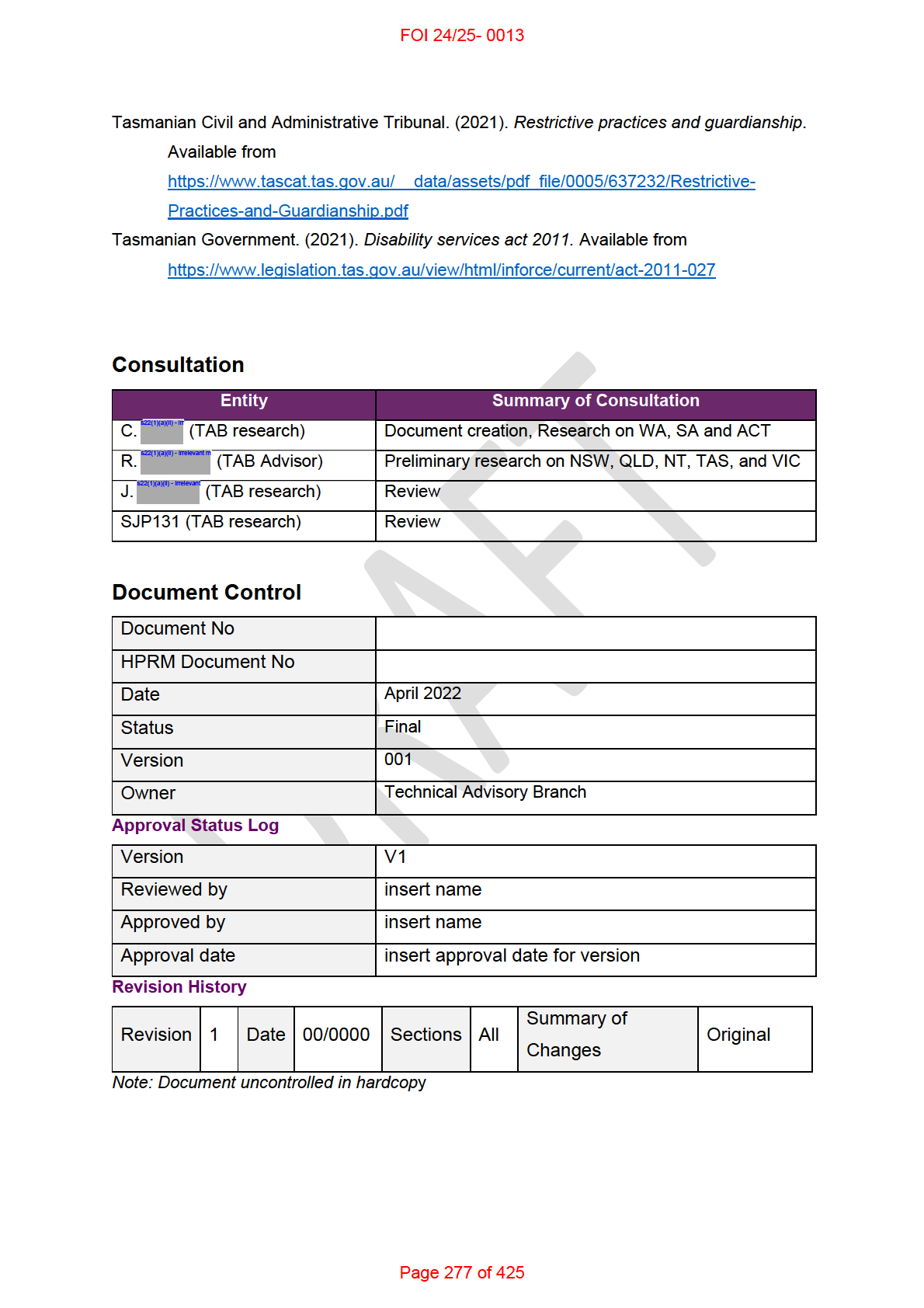
ICARE NSW has produced guidance relevant to people with Spinal Cord Injury. This
document estimates support needs for different levels of spinal cord injury. Considerable
clinical judgement is required to determine appropriate support hours. Ratios of support are
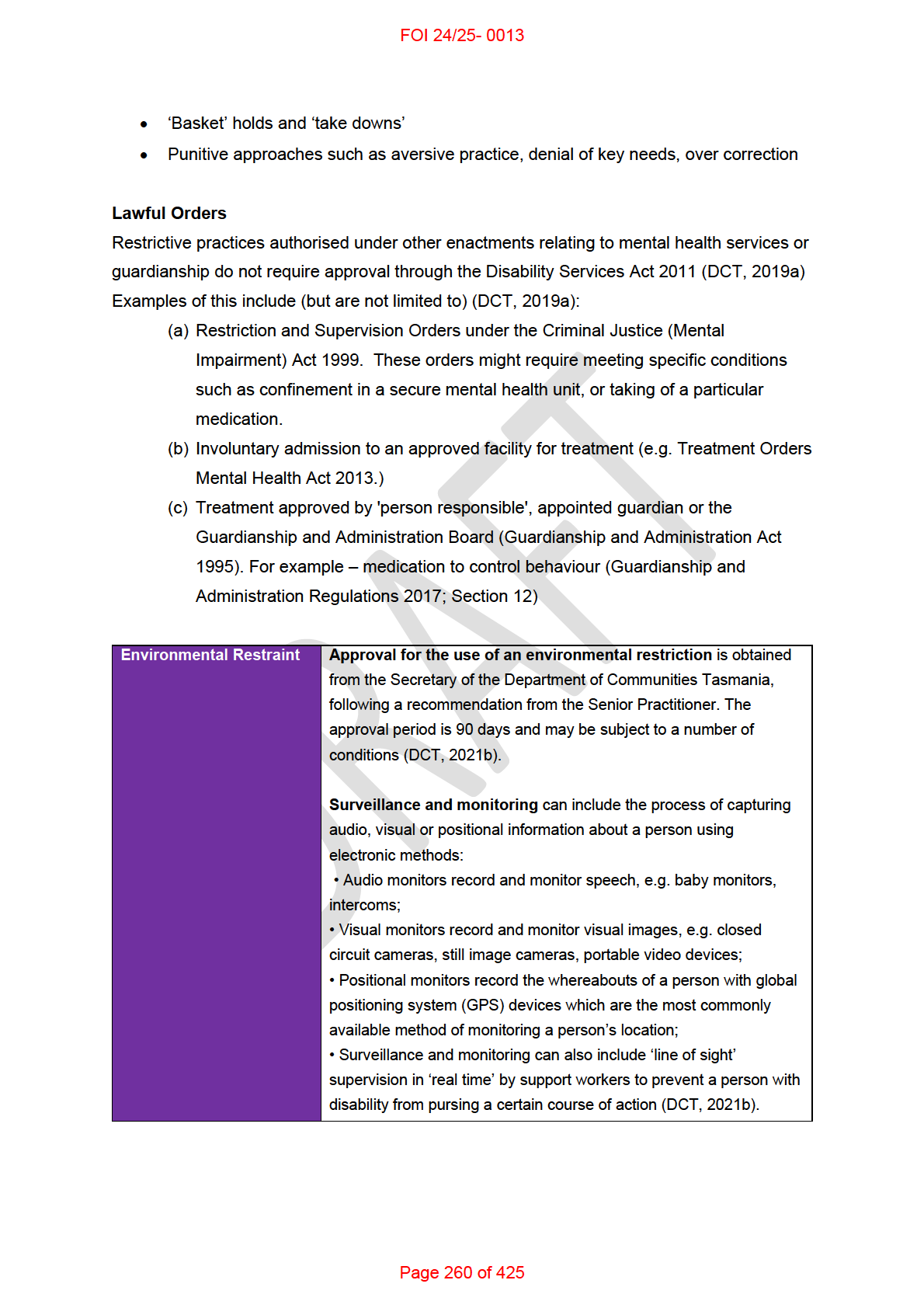
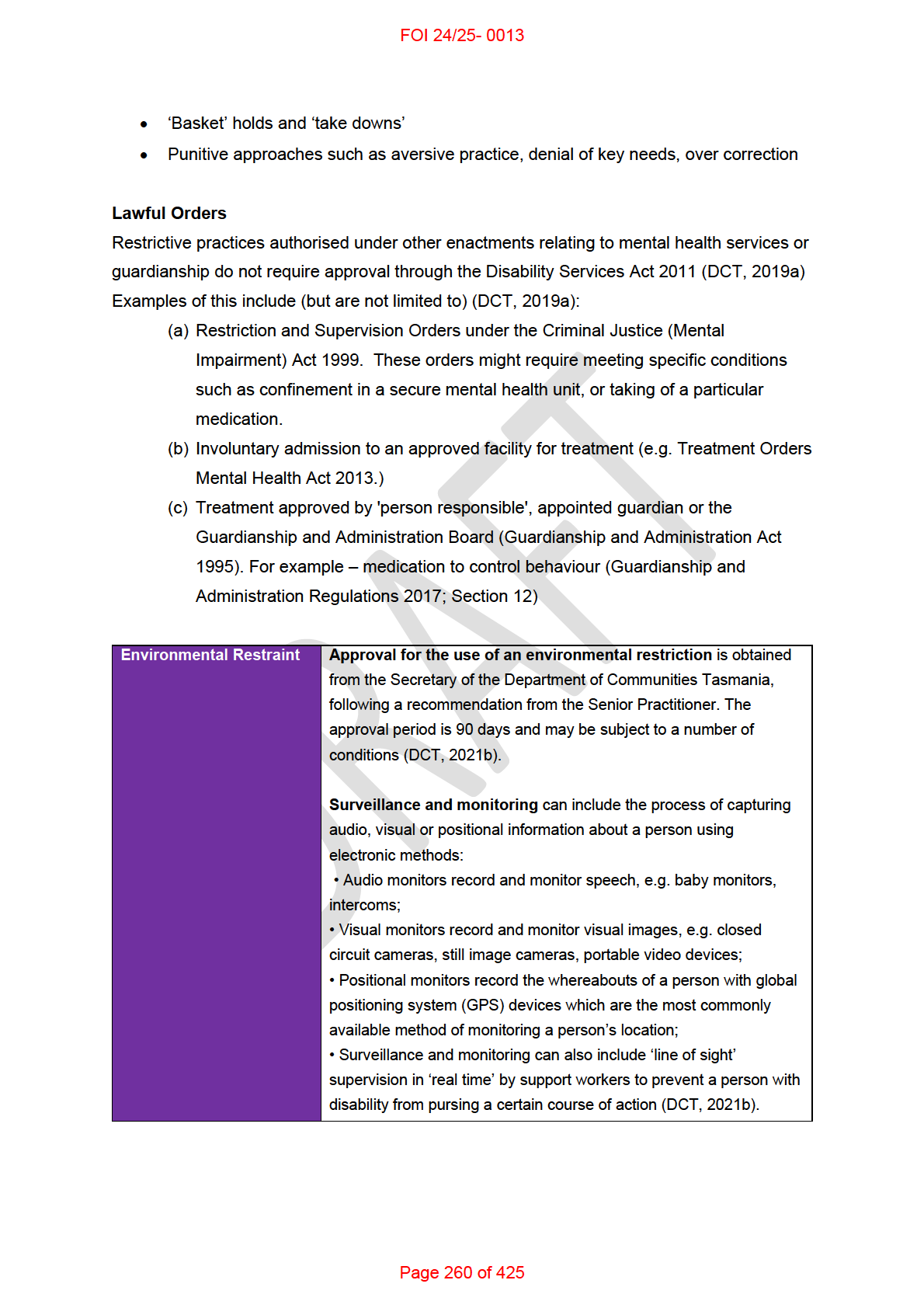
not explicitly mentioned. However, the estimates do appeal to the following scale:
[8]
As reasoned in 3. Assessment Tools, it may be possible to interpret this scale as implying
something about support ratios, however this would need to be done carefully and with
individual clinical justification.
I have not found any professional or governmental guidelines that could assist with
determining appropriate ratios of support for community access or group social activities. I
reached out to 13 professional Occupational Therapy organisations. I received replies from 6.
All 6 of the groups (s22(1)(a)(ii) - irrelevant material
) confirmed that there were no overall guidelines and
that determination of support ratios occurs at a local or individual level [7. Appendix –
Correspondence].
Members of the s22(1)(a)(ii) - irrelevant material reference group have advised:
Guidelines could be useful. However, information must be triangulated including
person’s own statement of performance, with observation, other clinical and care
information, client environment, and other relevant contextual factors. Any
inconsistencies need to be sorted out. Each client’s social and community participation
levels are different. What is reasonable and ordinary for their age, relationships, skil set
and social needs should be considered [s22(1)(a)(ii) - irrelevant material].
s22(1)(a)(ii) - irrelevant material , the Professional Practice Advisor from s22(1)(a)(ii) - i, als o referred me to a member of
their NDIS Reference group for further advice. s22(1)(a)(ii) - irrelevant material, OT and founder/director of
s22(1)(a)(ii) - irrelevant material , is in the process of developing and trialling a support measure aimed
Page 224 of 425
FOI 24/25- 0013
at informing NDIS planning decisions.
Discussions regarding this project are pending
s22(1)(a)(ii)
].
5. Factors that can influence ratios of support
s22(1)(a)(ii) - i me mbers advised the following factors can influence decisions about determining support
ratio:
• level of risk to self, others and property damage
• past incident reports
• manual handling risk plans
• self-report around comfort, confidence
• cognition
• safety risks
• vulnerability within the community
• public transport confidence/ability/ability to be trained
• level of supervision required
• maximum benefit – do they participate/benefit with number of people around
• compatibility with others, e.g. issues participating with other genders precluding
group ratios
• opportunities/abilities to learn from others and form natural relationships
• unpredictable or ad hoc support needs such as behavioural support or toileting
support [s22(1)(a)(ii) - irrelevant material].
Relevant considerations can include personal, environmental and institutional factors.
Personal factors can include:
• goals and lifestyle
• physical features of the person (height, weight etc.)
• functional capacity of the person (e.g. capacity to assist with transfers or to self-
mobilise)
• the behaviour and personality of the person (e.g. presence of behaviours of concern,
how well they get on with the staff)
• the person’s capacity to engage in social activities (need for prompting, active
inclusion etc.)
• need for assistive technology / availability of assistive technology
Page 225 of 425
FOI 24/25- 0013
Environmental factors can include:
• risk of the activity (e.g. swimming, operating tools/equipment)
• complexity of the activity (e.g. complex employment tasks, navigating crowded
event)
• duration of the activity (e.g. travel time, short trip to the shops, day trip out of town)
• risk in the environment (e.g. beach, busy urban streets, crowded events)
Institutional factors can include:
• consideration of the needs of all individuals in a group
• manual handling policy of the organisation
• availability of assistive technology, accessible vehicles etc.
• availability of trained staff
• other staffing needs (e.g. scheduled breaks, support for staff with a disability)
• legislative requirements, codes of practice, professional guidelines
This list is not exhaustive. The complexity and interdisciplinarity of determining support ratios
may provide a clue as to why there is very little research directly focussing on the topic.
5.1 Manual Handling
Safe Work Australia and state-based work safety organisations have codes of practice relating
to manual handling tasks [9,10,11]. The Safe Work Australia
Code of Practice for Hazardous
Manual Tasks suggests that, to maximise worker safety, transfer equipment should be
preferred to team handling. In other words, where possible a single person should assist a
patient or client using suitable assistive technology rather than two or more people assisting a
patient or client manual y. There are of course exceptions for equipment that is designed to be
operated by two people [9]. A 2011 Work Safe Victoria guideline suggests that two people may
be required to operate an electric hoist where the patient or client is not able to assist [10]. A
2006 manual handling guideline from the NSW Department of Ageing, Disability and Home
Care (now the Department of Community and Justice) states that clients with uncontrolled
movement may require two carers for personal care tasks. The guideline also recommends the
development of a Client Manual Handling plan for risk management and support planning [12].
Phil ips, Mellson and Richards emphasise the importance of individual risk assessments rather
than just assuming that one or two carers are appropriate for transfers [13]. Thornton observes
that two carers are often required for floor hoists, while a single carer is required for ceiling
hoists. The latter is safer and generally more cost effective [14]. Determining whether 1:1 or
2:1 is required for transfers depends on the suitability of available equipment with implications
for funding of ceiling hoists or floor hoists.
Page 226 of 425
FOI 24/25- 0013
5.2 Behaviours of concern
Behaviours of concern are a frequent reason for requesting higher staff ratios. I could not find
any research directly investigating the relationship between staff ratios and behaviours of
concern. A 2021 Cochrane review completed by researchers at the NDIS Quality and
Safeguard Commission investigated organisational interventions for reducing use of restrictive
practices. They listed 11 potential interventions but did not explicitly consider staffing numbers
or staff-client ratios as a factor in use of restrictive practices [15]. Correspondence with the
author of this review suggested other potential sources (refer to s22(1)(a)(ii) - irrelevant material
). A 2009 report from the Victorian government
summarises the relationship between staffing levels and restrictive practices:
Staffing factors have been identified as critical, though there is a lack of consensus in
the literature as to how best to determine optimum staffing numbers. Higher staffing
ratios have been suggested as a means of enabling early intervention and prevention of
escalation. However, the availability of higher levels of staff have also been associated
with a greater likelihood of staff using physical interventions, if for no other reason than
they have the person power available to do so. Similarly, while lower staffing ratios
make it practically more difficult to use restraint, lower staffing levels can also contribute
to staff feeling anxious and consequently more likely to deploy restrictive practices
earlier than they might otherwise do so had they the support (reassurance and security)
of other staff close by who could offer assistance if required. Further research into these
issues is necessary [16].
Relating specifically to staff-client ratios, the report refers to a study in which the researchers
found higher staff to patient ratios resulted in increased use of restrictive practice when the
staff in question were nursing assistants. However, there was a decreased use of restrictive
practices when the staff in question were registered nurses [16]. This finding could not be
corroborated as the reference appears to be incorrect, however it does coincide with other
research that suggests training has a greater effect than staff numbers. Singh et al found that
training staff with mindfulness techniques reduced staff interventions for aggression and this
was true at low, moderate and high staff-client ratios [17].
6. Social service analogues
I looked into the literature related to ratios of support in aged care and childcare. Unfortunately,
the literature did not add much to the considerations already raised above.
There is inconsistent evidence that ratios of support affect children’s learning and
developments in early learning environments. A 2016 study by Iluz, Adi-Japha and Klein found
some association between ratios of support and positive peer interactions [18]. A later
systematic review found “child-staff ratios for pre-school aged children classrooms have small,
if any, associations with concurrent or subsequent child outcomes” [19]. Though ultimately the
standard of evidence in the reviewed papers was low.
Page 227 of 425
FOI 24/25- 0013
In the context of aged care, a study by Baker et al found that abuse is more likely to occur in
situations where there is not sufficient staff to complete all the work [20]. A study by Karimi-
Shahanjarini et al found that insufficient staff in a hospital setting leads to lack of organisation
and ‘ad hoc’ shifting of tasks [21]. In both these cases, it is not clear what counts as
‘insufficient staff’. While the findings might be relevant to determining the importance of proper
ratios, they do not support planning for what those ratios might be.
7. Appendix – Correspondence
I sent an initial inquiry to 13 professional occupational therapy organisations via email on 30th
September 2021 (refer to table below). With minor variations for individual organisations, the
message read:
I am completing some research for the National Disability Insurance Agency, the
organisation that administers Australia’s National Disability Insurance Scheme (NDIS).
The NDIS provides support to eligible people with intellectual, physical, sensory,
cognitive and psychosocial disability.
I am currently compiling existing research on how occupational therapists determine
ratios of support for community access and group social activities. I am interested in
how this is achieved internationally.
It is common practice for Occupational Therapists to recommend support ratios required
by their clients. For example, while one person may require 2:1 direct assistance for
certain tasks, another person might thrive with 1:7 supervision for the same task. My
questions are:
• What considerations go into determining the appropriate ratio of individual support
(i.e. 1:1 or 2:1)?
• What considerations go into determining a safe and effective ratio of group support
(i.e. 1:3 versus 1:7)?
I’m hoping you might be able to provide some information on how your members
determine the appropriate ratio of support. If possible can you please provide any:
• recommendations you make to your members regarding ratios of support
• best practice guidelines you may have developed or refer to in order to determine
appropriate ratios of support
• existing research you appeal to in making recommendations / developing guidelines
for ratios of support
• contacts you believe may be able to assist with my inquiry.
Thank you very much for your time and all the best
Page 228 of 425
FOI 24/25- 0013
s22(1)(a)(ii) - irrelevant material
Page 231 of 425
FOI 24/25- 0013
s22(1)(a)(ii) - irrelevant material
Page 232 of 425
FOI 24/25- 0013
s22(1)(a)(ii) - irrelevant material
Page 233 of 425
FOI 24/25- 0013
s22(1)(a)(ii) - irrelevant material
Page 234 of 425
FOI 24/25- 0013
s22(1)(a)(ii) - irrelevant material
Page 235 of 425
FOI 24/25- 0013
s22(1)(a)(ii) - irrelevant material
Page 236 of 425
FOI 24/25- 0013
s22(1)(a)(ii) - irrelevant material
Page 237 of 425
FOI 24/25- 0013
s22(1)(a)(ii) - irrelevant material
8. References
[1] s22(1)(a)(ii)
J.
- irrelevant m
Resource to Assist with Determining Personal Care Hours. TAB Research Team
paper 2021.
[2] Verdugo MA, Aguayo V, Arias VB, García-Domínguez L. A systematic review of the
assessment of support needs in people with intellectual and developmental disabilities. Int J
Environ Res Public Health. 2020;17(24):9494.
[3] Giné C, Font J, Guàrdia-Olmos J, Balcells-Balcells A, Valls J, Carbó-Carreté M. Using the
SIS to better align the funding of residential services to assessed support needs. Res Dev
Disabil. 2014;35(5):1144–51.
[4] Arnold SRC, Riches VC, Stancliffe RJ. I-CAN: the classification and prediction of support
needs. J Appl Res Intel ect Disabil. 2014;27(2):97–111.
[5] International SIS Use [Internet]. American Association on Intellectual and Developmental
Disabilities. [cited 2021 Oct 6]. Available from: https://www.aaidd.org/sis/international.
[6] Profile Form. Supports Intensity Scale [Internet]. American Association on Intellectual and
Developmental Disabilities. [cited 2021 Oct 6]. Available from:
https://www.aaidd.org/docs/default-source/sis-docs/sis form do not copy.pdf?sfvrsn=2.
[7] I-CAN [Internet]. Centre for Disability Studies. [cited 2021 Oct 6]. Available from:
https://www.i-can.org.au/.
[8] Lukersmith S (ed.) ICARE (Insurance and Care NSW). Guidance on the support needs for
adults with spinal cord injury. 2017. Sydney, Australia.
[9] Code of Practice for Hazardous Manual Tasks [Internet]. Safe Work Australia. [cited 2021
Oct 6]. Available from:
https://www.safeworkaustralia.gov.au/system/files/documents/1905/model-cop-hazardous-
manual-tasks.pdf.
[10] A health and safety solution – assisting people who have fallen [Internet].
WorkSafeVictoria. [cited 2021 Oct 6]. Available from:
https://content.api.worksafe.vic.gov.au/sites/default/files/2018-06/ISBN-A-health-and-safety-
solution-assisting-people-who-have-fallen-2011-05.pdf.
[11] Code of Practice for Hazardous Manual Tasks [Internet]. Safe Work NSW. [cited 2021 Oct
6]. Available from:
https://www.safework.nsw.gov.au/ data/assets/pdf file/0020/50078/Hazardous-manual-
tasks-COP.pdf.
Page 238 of 425
FOI 24/25- 0013
[12] Best Practice Guidelines for Manual Handling [Internet]. Department of Ageing, Disability
and Home Care. [cited 2021 Oct 6]. Available from:
http://disabilitysafe.org.au/sites/default/files/DADHC Best Practice Guidelines MH.pdf.
[13] Phil ips J, Mellson J and Richardson N. It takes two? exploring the manual handling myth.
2014. University of Salford. Available from: http://usir.salford.ac.uk/id/eprint/43619/.
[14] Thornton S. An ergonomics approach to managing transfers from two handed to single
handed care [Thesis]. Loughborough University. [cited 2021 Oct 6]. Available from:
https://iosh.com/media/4403/sarah-thornton.pdf.
[15] Iffland M, Xu J, Gil ies D. Organisational interventions for decreasing the use of restrictive
practices with children or adults who have an intellectual or developmental disability. Cochrane
Libr [Internet]. 2021; Available from: http://dx.doi.org/10.1002/14651858.cd013840.
[16] McVilly K. Physical restraint in disability services: Current practices, contemporary
concerns, and future directions [Report]. State Government of Victoria 2009.
[17] Singh NN, Lancioni GE, Winton ASW, Curtis WJ, Wahler RG, Sabaawi M, et al. Mindful
staff increase learning and reduce aggression in adults with developmental disabilities. Res
Dev Disabil [Internet]. 2006;27(5):545–58. Available from:
http://dx.doi.org/10.1016/j.ridd.2005.07.002.
[18] Iluz R, Adi-Japha E, Klein PS. Identifying child–staff ratios that promote peer skil s in
childcare. Early Educ Dev [Internet]. 2016;27(7):1077–98. Available from:
http://dx.doi.org/10.1080/10409289.2016.1175240.
[19] Perlman M, Fletcher B, Falenchuk O, Brunsek A, McMullen E, Shah PS. Child-staff ratios
in early childhood education and care settings and child outcomes: A systematic review and
meta-analysis. PLoS One [Internet]. 2017;12(1):e0170256. Available from:
http://dx.doi.org/10.1371/journal.pone.0170256.
[20] Baker PRA, Francis DP, Hairi NN, Othman S, Choo WY. Interventions for preventing
abuse in the elderly. Cochrane Database Syst Rev [Internet]; 2016(8):CD010321. Available
from: http://dx.doi.org/10.1002/14651858.CD010321.pub2.
[21] Karimi-Shahanjarini A, Shakibazadeh E, Rashidian A, Hajimiri K, Glenton C, Noyes J, et
al. Barriers and facilitators to the implementation of doctor-nurse substitution strategies in
primary care: a qualitative evidence synthesis. Cochrane Database Syst Rev [Internet].
2019;4:CD010412. Available from: http://dx.doi.org/10.1002/14651858.CD010412.pub2.
Page 239 of 425

FOI 24/25- 0013
DOCUMENT 25
Home automation as an everyday living cost
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be
shared external to the Branch. These are for internal TAB use only and are intended to
assist our advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If
Delegates require further information on access or planning matters, they are to call the
TAPS line for advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: How common is home automation/”smart homes” in Australia?
What is the typical ‘scope of works’ for a standard ‘smart home’ vs disability-specific home
automation features?
What is the typical cost or price range to setup a ‘smart home’?
Are existing homes able to accommodate home automation without needing to upgrade
electrical features (e.g. switchboard, wiring)?
Is there a significant dif erence in outcomes between low cost solutions (e.g. Google Home)
and high cost solutions (e.g. Control 4)?
What is the current evidence base regarding home automation and people with disability? Is
there evidence home automation is linked to increased independence, or other positive
outcomes (e.g. improved quality of life, wellbeing)? Are there any best practice guidelines?
What is the Agency’s risk appetite for home automation requests? Do mitigation strategies
need to be put in place (e.g. TAB mandatory referral for requests above $20,000)?
Date: 09/05/2022
Requestor: Claire s22(1)(a)(ii)
- irrele
Endorsed by (EL1 or above): Sandi s22(1)(a)(ii) - irrelevant material
Researcher: Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Stephanie s22(1)(a)(ii)
- irrelevant mate
Page 278 of 425
FOI 24/25- 0013
1. Contents
Home automation as an everyday living cost ............................................................................. 1
1.
Contents ....................................................................................................................... 2
2.
Summary ...................................................................................................................... 2
3.
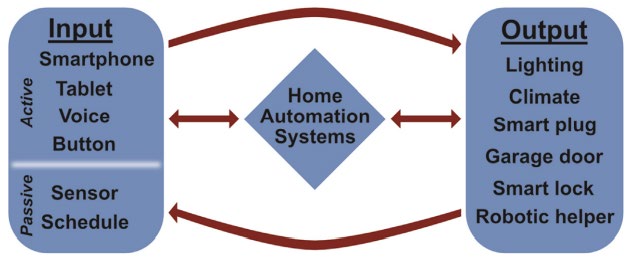
What is home automation? ........................................................................................... 3
4.
Home automation in Australia ....................................................................................... 4
5.
Home automation as a disability support ...................................................................... 4
5.1 Benefits ...................................................................................................................... 5
6.
Risk ............................................................................................................................... 7
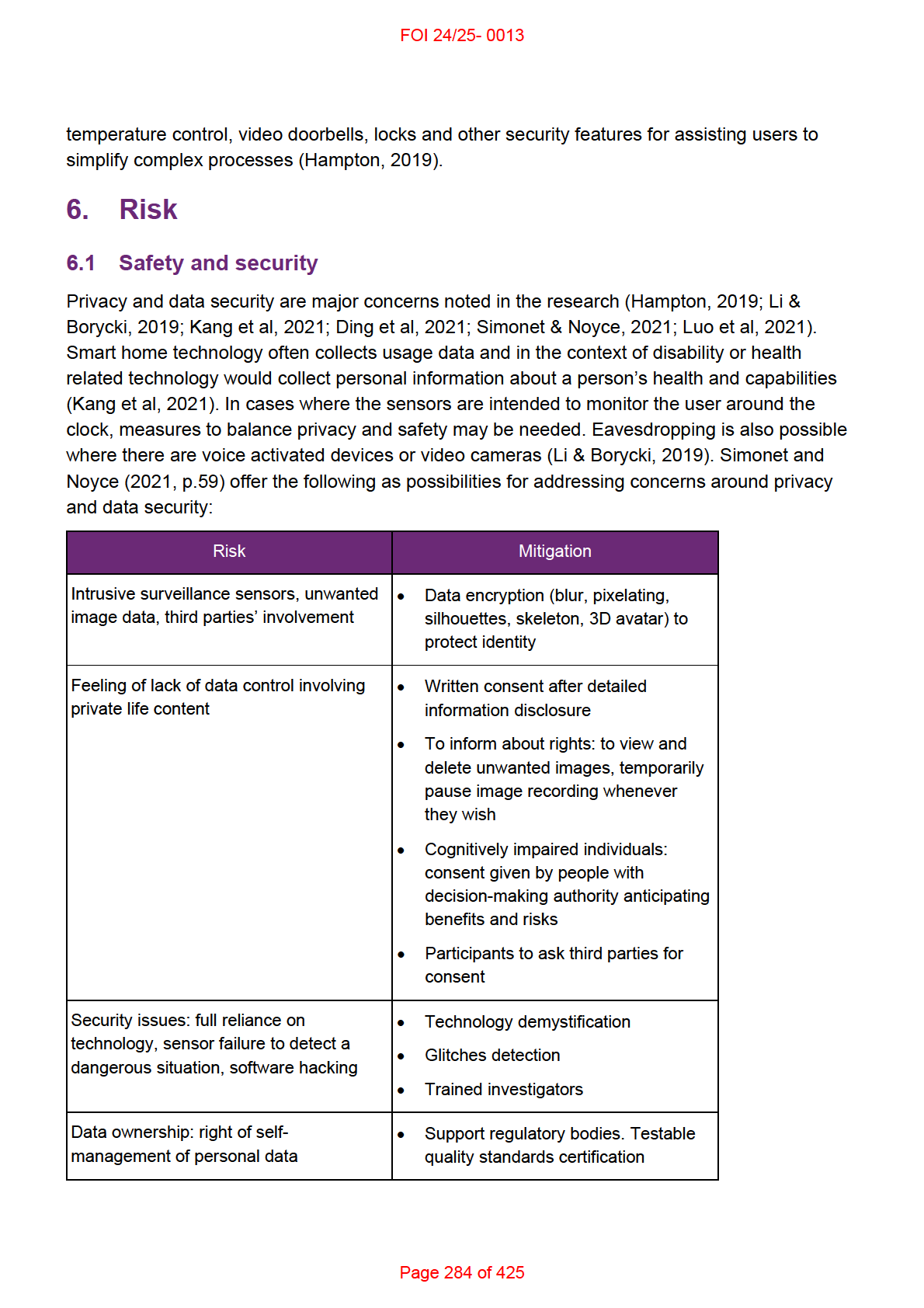
6.1 Safety and security .................................................................................................... 7
6.2 Cost effectiveness ..................................................................................................... 8
7.
References ................................................................................................................. 10
8.
Version control ............................................................................................................ 12
2. Summary
Smart home technology is growing in popularity in Australia. Most people having at least one
smart home device in their home. While common, only certain types of automations (eg.
entertainment) are ubiquitous in Australian homes. Whether a particular home automation
support is more likely an everyday living cost wil depend on the type and function of the
technology.
With the technology growing and changing, there is inconsistent and outdated information
online. Much of the research is still in very early stages and so the evidence base is minimal.
There is more research focussing on maintaining independence of older people compared to
other disability cohorts.
There is a body of research focussed on using sensors and the Internet of Things (IoT) in the
home to monitor and assess people at risk of various harms (for example, trips or falls, burns
when cooking etc.). Although home automations are often integrated with IoT, this paper will
only discuss IoT technology when it relates to automating processes in the home. Similarly,
there is a strong research focus on use of robotics to automate processes in the home (for
example, a robot vacuum to clean the floor). There may not be distinct boundaries between
home automations and robotics, but this paper will focus on the automation of processes
related to structure or fixtures of the house and environment (for example, automated lights,
doors or heating/cooling systems).
Page 279 of 425
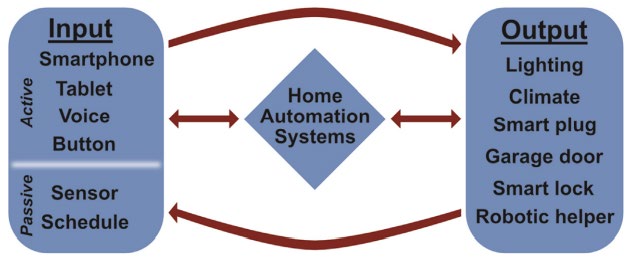
FOI 24/25- 0013
From the available information it appears that for most common home automations, off-the-
shelf control units like Google Home, Apple Home kit or Amazon dot may be sufficient with
installation of automated appliances or fixtures. If these mainstream options are not accessible
for a user, or if they require a more customised solution, then specialised home automation
systems may be required.
Currently, we do not have accurate information about how often home automations are funded
and what the average costs that quotes are implemented for. Without this information we
cannot accurately determine financial risk to the scheme.
3. What is home automation?
Anything that moves or turns on and off can be automated. In a house, this can include lights,
electricity outlets, doors, windows, drawers, blinds, locks, showers, baths, sinks, toilets, air-
conditioning, ceiling fans, platform or stair lifts, cameras, intercoms, alarms or other security
features, watering or reticulation systems. Any home appliance can be automated including
TVs, sound systems, vacuums, fridges, kettles and coffee makers etc.
Home automations, sometimes called domotics, can be linked or integrated via home internet
or wireless technology and operated via phones, tablets, computers or dedicated control
interfaces, allowing users to control structural or environmental features of their home. A home
in which automation is integrated with the Internet of Things is often called a smart home (Choi
et al, 2021; Katre & Rojatkar, 2017). The Internet of Things refers to a network of computing
devices which can communicate with each other via a system of sensors (Choi et al, 2021).
For example, a bedroom light turns on when the bedroom door is opened thanks to a sensor in
the door, or a wearable temperature sensor can send information to an air-conditioner to
regulate the room temperature. This is an example of an automated system with a passive
input. It’s called passive because the user does not have to intentionally turn the light on, it is
turned on by doing another activity the user would have done anyway (opening the door). This
contrasts with active input, in which the user speaks or operates controls on a tablet or phone
(Hampton, 2019). Figure 1 illustrates the relationship between inputs and outputs in a home
automation system.
Figure 1: Home automation systems. Source: Hampton, 2019.
Page 280 of 425
FOI 24/25- 0013
4. Home automation in Australia
There is little reliable data on the prevalence of home automations in Australian households.
The information that is available was gathered for commercial purposes and may have
inherent bias. Data from the Statista Global Consumer survey of 2049 people found 85% had
some smart home device in their house. Entertainment devices are the most common (79%),
followed by:
• devices for monitoring and automating electricity and lighting (30%)
• safety and security (29%)
• smart appliances (26%)
• smart speakers with virtual assistant (22%)
• energy management (22%) (Statista 2022).
A 2022 Savvy survey of 1000 people found 48% aged over 55 have at least one smart home
device and 41% have 5-10 devices. 58% of people 18-44 have at least one smart home device
in their home (Chavda, 2022). Due to barriers accessing the ful datasets or reports for these
surveys, the definitions of ‘smart device’ or ‘smart home device’ are not clear. They may
include devices as common as Bluetooth speakers or motion sensor lights. Also, information
substantiating the representativeness of the survey group is not available.
5. Home automation as a disability support
There is no standard home automation scope of works in either a mainstream or disability
support context. However, based on a review of 20 TAB advice requests from 2021/2022,
common automation requests include:
• doors and locks
• windows and blinds
• lighting (ceiling lights or lamps)
• heating/cooling (air-conditioner, ceiling fans)
• intercom / video doorbell
• entertainment (TV, sound systems).
In a mainstream context, the goals of home automation include safety and security, comfort,
convenience and energy efficiency (Statista, 2022). Features designed for comfort or
convenience in a mainstream context can have significant implications for independent living
for people who live with a disability (Hampton, 2019). A 2021 survey of allied health
practitioners found commercially available home automation technology has been used to
assist people with traumatic brain injury, spinal cord injury, cerebral palsy, amyotrophic lateral
sclerosis, multiple sclerosis, stroke, dementia, Alzheimer’s, mild cognitive impairments, autism,
Page 281 of 425
FOI 24/25- 0013
Parkinson’s disease, low vision or blindness, and Down syndrome (Ding et al, 2021). Home
automation can be useful to:
• remove physical barriers to the use of fixtures or appliances
For example, the automation of doors, windows, and blinds can be used to change the
usual physical input (pushing, lifting, reaching, pulling) which a user might have difficulty
with to a different input within the user’s ability (speaking a voice command, using a
touch screen).
• prompt a user to complete daily activities
For example, a user might require prompting to brush their teeth in the morning, so they
install a sensor on the bedroom door which triggers a voice prompt when the user first
leaves their bedroom in the morning.
• simplify complex process
For example, if a user has difficulty remembering everything they need to do to secure
their house when they leave, multiple processes (lock doors, close windows and blinds,
turn off all lights and appliances), could be activated via a single input (press a single
button on their smartphone).
5.1 Benefits
Research focussing on the use of home automation in a disability, health or ageing context is
only a smal portion of the research literature on home automation (Li et al, 2022; Choi et al,
2021). Despite this, healthcare was one of the first applications of smart home research
represented in the literature. This body of research looks at technology for monitoring health of
patients, improving service delivery and promoting ageing in place.
Much of the literature on the effectiveness of home automation or Smart home technology
focusses on home care for older people (Lee & Kim, 2020; Tural et al, 2021; Astasio-Picado et
al, 2022). This literature has shown that smart home technology including sensors, automated
lighting, locks and fire detection devices can reduce hospitalisation among older adults,
improve feelings of safety and security and promote ageing in place. However, since the focus
is on older people, the results may not generalise across disability cohorts.
Research into the use of home automation in a disability context is still developing. As late as
2008, a Cochrane review found no randomised controlled trials, quasi‐experimental studies,
controlled before and after studies or interrupted time series analyses looking into home
automation as a treatment for people with physical disability, cognitive impairment or learning
disability. Noting that these technologies are in use, the authors recognise that technology
often finds its way into the healthcare industry “without comprehensive evaluation of the health
impact or a true understanding of the added value of ICT to health services” (Martin et al,
Page 282 of 425
FOI 24/25- 0013
2008, p.5). Research also often develops slower than technology, so that by the time research
is completed, a technology may be obsolete (TAC, n.d).
The evidence base is still minimal though preliminary studies show a positive effect of home
automation. A 2021 review into the use of home automation and smart home technology for
people with Parkinson’s found benefit in improving autonomy and safety, but this is primarily
using sensors and data-collection to inform health care providers of risks (Simonet & Noyce,
2021). Two pilot studies into the use of home automation found improvements in social
adaptation, activities of daily living and quality of life for people with Parkinson’s disease
(Latella et al, 2021) and improvements in social and cognitive functioning and autonomy in
people with chronic stroke (Maggio et al, 2020). However, both pilot studies measure use of
home automation in short sessions rather than as a ubiquitous living environment.
Victoria’s Transport Accident Commission has funded a research project looking at smart
home technology for supporting memory, planning and organisation. The research is
scheduled to be completed in 2022 (TAC, n.d.).
Removing physical barriers. There is some evidence on the usability and accessibility of
control systems for operating common home automations (Masina et al, 2020; Conado et al,
2022). For example, Masina et al (2020) found accessibility issues in the use of voice
assistants (Siri, Alexa, Cortana etc) for people with cognitive and linguistic impairments. I have
found no evidence relating to the effectiveness of common home automations to remove
physical barriers. This may be due to the early stages of the evidence base or the typical
heterogeneity of new technologies. It may also relate to the fact that home automations
straight-forwardly allow people to perform these basic activities (turn lights on and off, open
doors and windows) provided the controls are accessible.
Prompting. A 2015 study into prompting technology found an effective prompting system:
can improve the efficacy of cognitive interventions, minimize the necessity for human
assistance, and allow users to feel more independent. Research has shown that
prompting technologies can enhance medication adherence, improve the use of
external compensatory strategies, reduce caregiver burden, and increase functional
independence in those with cognitive impairment (Robertson et al, 2015, p.9).
The authors note prompting is most ef ective during points of transition (when finishing or
starting a different activity) and less effective when the prompt occurs at a specific time of day
regardless of what the user is doing (for example, a reminder set for 8:30am every day). Smart
home technology can facilitate prompting triggered by certain activities (leaving or entering a
room, getting out of bed, turning an appliance on or off) and so may be more targeted than
simple time-of-day prompts.
Simplifying complex processes. In a 2019 introduction to home automation, Hampton
suggested there was no significant evidence base for the effectiveness of home automation for
people with disability. However, he does acknowledge the usefulness of automated lights,
Page 283 of 425
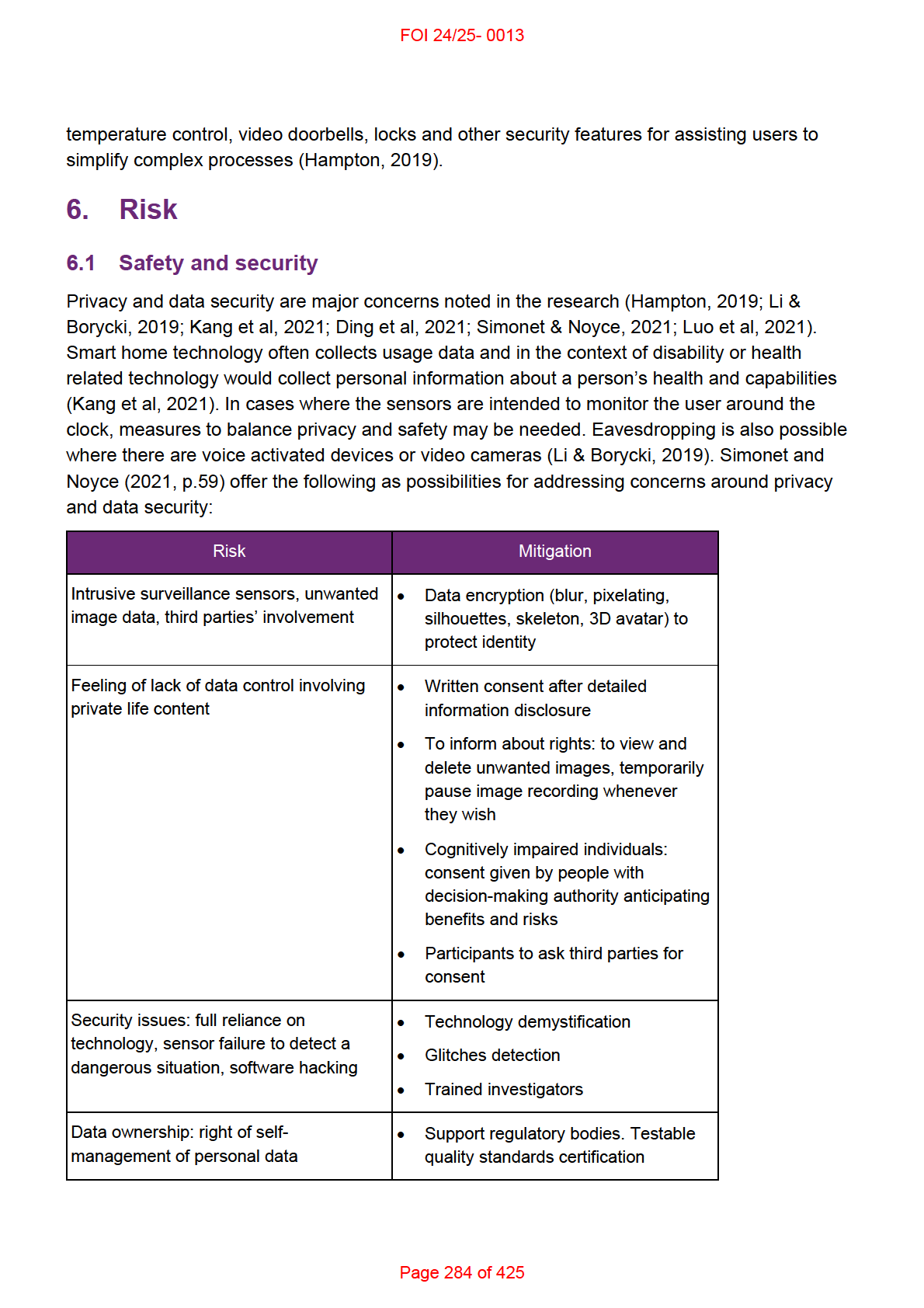
FOI 24/25- 0013
Other risks relate to networking and remote operation of basic household processes. If a
device is connected to a user’s Wi-Fi and there is a network failure this may cause be safety
issues such as the inability to open or unlock doors. This might be mitigated by systems which
connect via Bluetooth or Z-Wave and do not depend on Wi-Fi network. If a smart home system
is hacked, all the automated systems may be vulnerable to remote operation. This may be
mitigated by appropriate digital security measures. In addition, remote operation of doors and
locks raises concerns of restrictive practice. This risk could be mitigated by limiting number of
users with access to the systems and identifying if a behaviour support plan involving
restrictive practice is required.
6.2 Cost effectiveness
I have not found any research on the cost effectiveness of home automations compared to
personal assistance. There is a suggestion in the literature that home automation can increase
independence and reduce carer burden, but this is not quantified into reduced hours of
support. In theory, a person who only requires monitoring over the day could reduce the
amount of on-site care they require. However, for both on and off-site care, reduced hours
would depend on the support arrangement in place. There is some evidence that a person
only requiring prompting to complete daily activities could rely less on personal assistants and
therefore reduce care hours (5.1 Benefits). However, I have not seen any evidence showing
that home automations designed for prompting do reduce support hours.
As such, we cannot say that home automations have a track record of reducing support hours
and we cannot say in general that home automations are likely to be value for money.
Individual requests for funding may be able to demonstrate a likely reduction in support hours
or some comparable benefit that would make the request value for money. For example, if a
participant can sometimes navigate the community independently and an automated door will
enable them to enter or exit their home independently, then the request may increase their
independence to an extent that funding would be justified, even if it does not reduce support
hours.
There is inconsistent information available when comparing mainstream smart home hubs
(Google Home, Amazon Dot, Samsung SmartThings, Apple HomeKit etc) with more
specialised control units (C-Bus, Crestron, Mobotix, Control 4). This may be due to the
commercial nature of the reviews and the rapid progress of the technology. Most online
reviews compare mainstream hubs with each other or specialised control units with each
other, but do not compare mainstream with specialised.
Specialised units require more set-up and are more costly but allow for greater customisation.
Mainstream hubs are cheaper, fulfill most basic automation needs but their interface is less
customisable and may be less accessible. I have not found a home automation technology
designed specifically for people with disabilities, though with some specification both
mainstream hubs and specialised units can accommodate some accessibility measures. The
most cost-ef ective system will depend on the needs of the individual.
Page 285 of 425
FOI 24/25- 0013
For example, Apple Home is a free app which works with various accessories. It advertises the
ability to automate or work with air conditioners, air purifiers, bridges, cameras, doorbells, fans,
garage doors, humidifiers, lights, locks, power points, receivers, routers, security, sensors,
speakers, sprinklers, switches, taps, thermostats, TVs, and windows. It is compatible with
hundreds of products of various brands (Apple Home).
Google Home setups are currently selling for $99 and can automate several processes
independently (email, phone, entertain systems) and can link to additional modules (for
example, Samsung’s SmartThings) to:
lock and unlock doors, regulate air-con settings, open and close windows blinds, water
plants, start robotic vacuum cleaners, and arm and disarm alarm systems, [operate]
plug and power outlet, motion sensor, security camera, Honeywell thermostat, garage
door opener, washing machine, door bell and garden irrigation controller (Noda, 2018,
p.675).
Mainstream smart home hubs are inexpensive but require compatibility with devices or fixtures
in the home. This can involve buying new appliances or separately automating household
processes, which can sometimes involve substantial costs.
An additional consideration is re-wiring of a home. Mainstream accessories (lights and
appliances) and accessories or systems that run on batteries will often not need re-wiring.
Many home automation systems or devices need neutral wires and so some older homes may
require re-wiring. Some people choose to install deep junction boxes, wiring closets or higher
grade ethernet cables (Fritz, 2021; SmartHome, n.d., Tholen, 2021).
6.2.1 Reducing financial risk
When a request for home automation is determined to be reasonable and necessary a plan
developer includes the line item:
Environmental Control (ECU)/ Safety-Related Products 05_241303121_0123_1_2.
This is a quotable item in the Assistive Technology category with a benchmark of $17,474. The
line item for repair and maintenance is:
Repairs and Maintenance - Communication Cognitive or ECU AT
05_502200312_0124_1_2
and has a notional value of $500. Home automations are not a mandatory referral to TAB and
do not have any mandatory referral rules associated with them.
We do not currently have data on how frequently this line item is included in the plan and
whether the benchmark represents to average cost quotes are implemented for. However, this
information may be obtained from the Office of the Scheme Actuary. Without this information
we don’t have a good idea of the financial risk associated with these requests and we don’t
know if further risk mitigation strategies are required.
Page 286 of 425
FOI 24/25- 0013
However, without an idea of scale, some concerns and strategies are stil apparent. It is also
possible home automations are being included in plans without the line item or with a different
line item, contributing to the lack of clarity about how often this support is being funded. There
could be a few reasons for this. Home automations are funded through the Assistive
Technology category, though they sometimes blur the line between AT and Home
Modifications, requiring rewiring efforts or installation of built-in features like doors and
cabinetry. Plan developers may be looking to fund the support through the Home Modifications
budget. Environmental control unit is a technical term which may not be widely known. This
term may or may not be used in the request, assessment or quote and may not signal to the
plan developer to include the correct line item.
Either changing the name of the line-item to include a reference to home automation or
publicising the current line item and what it’s for could reduce the potential for home
automation funding being included via a different route.
Some risk reduction measures are introduced for supports costing above $15,000 such as a
full assessments and quotes. Risk of supports being funded that are not value for money could
be further reduced by creating a mandatory TAB referral rule (eg. mandatory referral to home
automations over $20,000).
Further support for decision makers might include adding a home automation example to the
Would We Fund It guide or adding a home automation advice request to the TAB digest.
7. References
Astasio-Picado, Á., Cobos-Moreno, P., Gómez-Martín, B., Verdú-Garcés, L., & Zabala-Baños,
M. (2022). Efficacy of Interventions Based on the Use of Information and
Communication Technologies for the Promotion of Active Aging.
International journal of
environmental research and public health,
19(3), 1534.
https://doi.org/10.3390/ijerph19031534
Condado, P. A., Lobo, F. G., & Carita, T. (2022). Towards Richer Assisted Living
Environments.
SN computer science,
3(1), 96. https://doi.org/10.1007/s42979-021-
00983-0
Chavda, S. (2022).
Smart home technology adoption rises with more Australians over 60
buying tech devices. Savvy. Retrieve May 6 2022, from
https://www.savvy.com.au/smart-home-technology-adoption-rises-with-more-
australians-over-60-buying-tech-devices/
Choi W, Kim J, Lee S, Park E. (2021) Smart home and internet of things: A bibliometric study.
Journal of Cleaner Production. 301, 126908
Ding, D., Morris, L., Messina, K., & Fairman, A. (2021). Providing mainstream smart home
technology as assistive technology for persons with disabilities: a qualitative study with
Page 287 of 425
FOI 24/25- 0013
professionals.
Disability and rehabilitation. Assistive technology, 1–8. Advance online
publication. https://doi.org/10.1080/17483107.2021.1998673
Fritz, R. (2021). How to wire your New House for home automation. Lifewire. Retrieved May 6,
2022, from https://www.lifewire.com/preparing-new-house-for-home-automation-817661
Hampton S. (2019). Internet-Connected Technology in the Home for Adaptive Living.
Physical
medicine and rehabilitation clinics of North America,
30(2), 451–457.
https://doi.org/10.1016/j.pmr.2018.12.004
Katre S and Sojatkar D. (2017). Home automation: past, present and future.
International
Research Journal of Engineering and Technology,
4(10), 343-346.
Kang, H. J., Han, J., & Kwon, G. H. (2021). Determining the Intellectual Structure and
Academic Trends of Smart Home Health Care Research: Coword and Topic Analyses.
Journal of medical Internet research,
23(1), e19625. https://doi.org/10.2196/19625
Latella, D., Maggio, M. G., Maresca, G., Andaloro, A., Anchesi, S., Pajno, V., De Luca, R., Di
Lorenzo, G., Manuli, A., & Calabrò, R. S. (2021). Effects of domotics on cognitive, social
and personal functioning in patients with Parkinson's disease: A pilot study.
Assistive
technology : the official journal of RESNA, 1–6. Advance online publication.
https://doi.org/10.1080/10400435.2020.1846095
Lee LN and Kim MJ (2020) A Critical Review of Smart Residential Environments for Older
Adults With a Focus on Pleasurable Experience.
Front. Psychol. 10:3080. doi:
10.3389/fpsyg.2019.03080
Li, C. Z., & Borycki, E. M. (2019). Smart Homes for Healthcare.
Studies in health technology
and informatics,
257, 283–287.
Li, W., Yigitcanlar, T., Liu, A., & Erol, I. (2022). Mapping two decades of smart home research:
A systematic scientometric analysis.
Technological Forecasting and Social Change,
179(121676), 121676. https://doi.org/10.1016/j.techfore.2022.121676
Luo, H., Liu, X., & Wang, P. (2021). Safety risk analysis of Home Automation products.
Journal
of Physics. Conference Series,
1986(1), 012103. https://doi.org/10.1088/1742-
6596/1986/1/012103
Maggio, M. G., Maresca, G., Russo, M., Stagnitti, M. C., Anchesi, S., Casella, C., Zichitella, C.,
Manuli, A., De Cola, M. C., De Luca, R., & Calabrò, R. S. (2020). Effects of domotics on
cognitive, social and personal functioning in patients with chronic stroke: A pilot study.
Disability and health journal,
13(1), 100838. https://doi.org/10.1016/j.dhjo.2019.100838
Martin S, Kelly G, Kernohan WG, McCreight B, Nugent C. Smart home technologies for health
and social care support. Cochrane Database of Systematic Reviews 2008, Issue 4. Art.
No.: CD006412. DOI: 10.1002/14651858.CD006412.pub2.
Masina, F., Orso, V., Pluchino, P., Dainese, G., Volpato, S., Nelini, C., Mapelli, D., Spagnolli,
A., & Gamberini, L. (2020). Investigating the Accessibility of Voice Assistants With
Page 288 of 425
FOI 24/25- 0013
DOCUMENT 26
Gym membership in Australia
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: How many Australians have gym memberships? What are their ages?
How many Australians with disabilities have gym memberships?
Date: 11/08/2022
Requestor: Andrea s22(1)(a)(ii) - ir
Endorsed by: n/a
Researcher: Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Aaron s22(1)(a)(ii)
- irrelevant ma
Review date:
1. Contents
Gym membership in Australia .................................................................................................... 1
1.
Contents ....................................................................................................................... 1
2.
Summary ...................................................................................................................... 2
3.
Gym membership in Australia ....................................................................................... 2
4.
Age and gym membership ............................................................................................ 3
5.
Disability and gym membership .................................................................................... 3
6.
References ................................................................................................................... 3
Page 290 of 425
FOI 24/25- 0013
2. Summary
Methodologically reliable but dated information from ABS indicates 17% of Australians had
gym memberships in 2015. Lower quality sources indicate 2020-2021 membership rates are
around 14%-15%. Very low quality sources indicate current gym membership in 2021 was
between 32% and 39%.
Very low quality sources indicate gym membership is most common in the 25 – 45 year age
bracket.
I was unable to find data on the number of gym members with disability. However, Australian
government sources show people with disability are more likely to have chronic health
conditions, more likely to be under financial stress and less likely to get enough exercise. This
suggests gym membership rates would be lower for Australians with disability.
3. Gym membership in Australia
Two sources from 2015 found less than one in five Australian’s have gym memberships. The
Australian Bureau of Statistics Participation in Sport and Physical Recreation, Australia survey
found 17% of Australians exercised at the gym (ABS, 2015). SunCorp Bank’s Cost of Being Fit
report finds 18% of Australians have gym memberships (Elsworth, 2015).
While this survey data is significantly dated, more recent information corroborates this rough
estimate. IHRSA, an international health and fitness industry peak body, published Australian
gym membership data in their 2020 global report. They found 15.3% of Australians have gym
memberships (Rizzo, 2021).
Another rough estimate is found in Rothwell’s account of the impact of COVID-19 on the
fitness industry. He states that COVID-19 related restrictions affected 3.7 mil ion consumers of
gym and fitness centres in Australia (Rothwell, 2023). This is roughly 14.4% of the Australian
population. While not necessarily an accurate estimate of gym memberships, it is corresponds
to the ABS, SunCorp and IHRSA estimates.
In contrast, the subscription data website Statista found 47% of Australians used gyms,
fitness, sports or leisure centres in 2020 (Share of people visiting gyms, fitness clubs, sports
centers Australia 2020, by age, n.d.). Their 2021 survey found 39.6% of Australians
participated in fitness and gym activities (Gym membership in Australia by age 2021, n.d.).
This may indicate a drop in memberships or may indicate ambiguity in the survey questions.
Also, the for-profit consumer advice website Finder determined 32% of Australians have a gym
membership (Lloyd, 2021).
Methodology of research from SunCorp, IHRSA, Statista and Finder are unclear and the
quality cannot be determined.
Page 291 of 425
FOI 24/25- 0013
4. Age and gym membership
Statista report:
In 2021, Australians aged between 25 and 34 years dominated the fitness and gym
industry in Australia, with over 1.7 mil ion Australians from the age group participating in
fitness or gym activities during the year. That year, gym and fitness participation was
least popular among survey respondents aged 15 to 17 and 55 to 64 years (Gym
membership in Australia by age 2021, n.d.).
Fitness Australia (2016) states that while 18-34 year olds are more likely to engage in
exercise, gym goers are more likely to be in the 26-45 age range.
5. Disability and gym membership
I was unable to find data on gym membership among people with disability.
The following is relevant contextual information. People experiencing socio-economic
disadvantage and people with long term health conditions are less likely to get enough
exercise (ABS, 2022). Australians with disability are six times more likely to have chronic
health problems and twice as likely to be under financial stress compared with the general
population. Three quarters of Australians with disability do not get enough exercise compared
to half of the general population (AIHW, 2022).
6. References
Australian Bureau of Statistics. (2015). Participation in Sport and Physical Recreation,
Australia, 2013-14 (No.4177.0). https://www.abs.gov.au/statistics/people/people-and-
communities/participation-sport-and-physical-recreation-australia/latest-release
Australian Bureau of Statistics. (2022). Physical Activity, 2021 (No.4364.0).
https://www.abs.gov.au/statistics/health/health-conditions-and-risks/physical-
activity/2020-21
Australian Institute of Health and Welfare. (2022). People with Disability in Australia, 2022 (No.
DIS 72). https://www.aihw.gov.au/getmedia/5f322ec4-ef63-4c43-a854-
64f7a2f55a04/aihw-dis-72-people-with-disability-in-australia-2022.pdf.aspx?inline=true
Elsworth, S. (2015). Australians spend $8.5 bil ion a year on gym memberships, sports
equipment, fitness fads. NewCORP Australia.
https://www.news.com.au/lifestyle/fitness/australians-spend-85-billion-a-year-on-gym-
memberships-sports-equipment-fitness-fads/news-
story/d0092769eaea24b59aa1b32d86999c98
Fitness Australia. (2016).
Profile of the Fitness Industry in Australia. https://bp-fitnessaustralia-
production.s3.amazonaws.com/uploads/uploaded file/file/173496/FAUS843-Industry-
Report-2016-Section-3-Digital.pdf
Page 292 of 425
FOI 24/25- 0013
Gym membership in Australia by age 2021. (n.d.). Statista. Retrieved August 11, 2022, from
https://www.statista.com/statistics/884599/australia-fitness-and-gym-participation-by-
age/
Lloyd, A. (2021).
Financial treadmil : Aussies wasting $2.4 bil ion on unused gym
memberships. Finder.com.au; Finder. https://www.finder.com.au/unused-gym-
memberships
Rizzo, N. (2021).
200+ gym industry statistics 2021. Athletic Shoe Reviews; RunRepeat.
https://runrepeat.com/gym-industry-statistics
Rothwell, L. (2022). COVID-19 and the Fitness Industry. In Frawley, S., & Schulenkorf, N.
(Eds.). (2022).
Routledge Handbook of Sport and COVID-19. Taylor & Francis. pp.235-
241
Share of people visiting gyms, fitness clubs, sports centers Australia 2020, by age. (n.d.).
Statista. Retrieved August 11, 2022, from
https://www.statista.com/statistics/884706/australia-gym-or-fitness-club-usage-share-
by-age/
Page 293 of 425
FOI 24/25- 0013
DOCUMENT 27
Eating out habits of Australians
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: How many meals on average Australians eat out or get take away per
week or month?
Date: 23/8/2022
Requestor: Kim s22(1)(a)(ii)
- irr
Endorsed by: Andrea s22(1)(a)(ii) - ir
Researcher: Stephanie s22(1)(a)(ii)
- irrelevant mate
Cleared by: Stephanie s22(1)(a)(ii) - irrelevant mat
Review date: n/a
1. Contents
Eating out habits of Australians .................................................................................................. 1
1.
Contents ....................................................................................................................... 1
2.
Habits of Australians consuming food prepared outside the home ............................... 2
3.
References ................................................................................................................... 5
Page 294 of 425
FOI 24/25- 0013
2. Eating habits of Australians for food prepared outside
the home
There is limited quality, peer reviewed literature addressing the question of how often
Australians eat food prepared outside the home and the method of procurement. One peer
reviewed paper was sourced, Cameron et al (2022), which reports data from the Australian
arm of the 2018 International Food Policy Study. This study is conducted annually in five
countries: Australia, Canada, Mexico, the United Kingdom and the United States. In 2018
there were 3963 Australian participants; data is collected through self-report methods.
Table 1 shows the source and frequency over one week of meals prepared outside the home.
Highlights from this table:
• An average of 2.73 (95% CI 2.61 – 2.86) meals per week were prepared outside the
home, this included fast food/take away an average of 1.35 times, sit down restaurant
or pub meal 0.73 times, sandwich or prepared food from supermarket 0.2 times.
• On average, males tend to source more food prepared outside the home at 3.08 times
per week (fast food 1.49 times per week; restaurant meals 0.78 times) than females at
2.40 times per week (fast food 1.21 times; restaurant 0.68 times).
• By age group, 18-29 year-olds source more prepared food from outside the home,
averaging 4.29 times per week (fast food most frequently 2.00 times per week, followed
by restaurants or pubs 0.95 times per week), with 30-44 year-olds second highest (fast
food 1.71 times per week, restaurants or pubs 0.76 times per week)
Table 2 reports how meals prepared outside the home were procured. Highlights from this
table:
• Food sourced from an outlet more than 5 minutes from home was procured most often
(1.13 times per week), followed by a food outlet less than 5 minutes from home (0.77
times), food delivery service (0.35 times) and restaurant delivery (0.33 times)
Page 295 of 425
FOI 24/25- 0013
Table 1
Source and frequency (over one week) of meals prepared outside the home, Australian data
Mean number of meals from each source (95% CI)
Fast
Sit-down
Work,
Sandwich
Food truck,
Petrol
Leisure
Vending
Other
Total
food/take
restaurant
School,
from
market
station,
centre,
machine
average of
away
or pub
University
sup’market
milk bar
entertainment
all sources
venue
Total
1.35
0.73
0.15
0.20
0.10
0.10
0.07
0.05
0.11
2.73
average
(1.29-1.41) (0.67-0.78) (0.12-0.18) (0.17-0.24) (0.08-0.13) (0.08-0.13)
(0.05-0.08)
(0.04-0.07) (0.08-0.13) (2.61-2.86)
Sex M
1.49
0.78
0.20
0.26
0.14
0.14
0.08
0.08
0.11
3.08
F
1.21
0.68
0.10
0.15
0.07
0.07
0.05
0.03
0.11
2.40
Age 18-
2.00
0.95
0.34
0.43
0.26
0.22
0.16
0.16
0.13
4.29
29
30-
1.71
0.76
0.20
0.30
0.13
0.16
0.10
0.07
0.07
3.28
44
45-
1.22
0.55
0.06
0.09
0.01
0.04
0.01
0.01
0.14
2.20
59
≥60
0.61
0.67
0.02
0.04
0.02
0.02
0.03
0
0.10
1.47
Cameron et al (2022)
Page 296 of 425
FOI 24/25- 0013
Table 2
Procurement of meals prepared outside the home, Australian data
Mean number of meals from each procurement method per week (95% CI)
Food delivery service
Restaurant delivery service
Food outlet < 5 mins from
Food outlet > 5 mins from
home
home
Total
0.35
0.33
0.77
1.13
(0.31-0.40)
(0.29-0.38)
(0.71-0.82)
(1.06-1.19)
Sex
M
0.46
0.42
0.84
1.19
F
0.25
0.25
0.69
1.07
Age
18-29
0.79
0.65
1.22
1.36
30-44
0.53
0.48
0.87
1.26
45-59
0.12
0.16
0.68
1.08
≥ 60
0.04
0.09
0.39
0.86
Cameron et al (2022)
Page 297 of 425
FOI 24/25- 0013
3. References
Cameron, A. J., Oostenbach, L. H., Dean, S., Robinson, E., White, C. M., Vanderlee, L.,
Hammond, D., & Sacks, G. (2022). Consumption frequency and purchase locations of
foods prepared outside the home in Australia: 2018 International food policy study.
Journal of Nutrition, 152, 76S-84S. doi: https:/ doi.org/10.1093/jn/nxab437
Page 298 of 425
FOI 24/25- 0013
DOCUMENT 28
Efficacy of Equine Therapy
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: What is the efficacy of equine therapy?
Date: 13/9/22
Requestor: Adam s22(1)(a)(ii) - irre
Endorsed by: Andrea s22(1)(a)(ii) - ir
Researcher: Stephanie s22(1)(a)(ii)
- irrelevant mate
Cleared by: Stephanie s22(1)(a)(ii) - irrelevant mat
Recommended review date: September 2023
1. Contents
Equine Therapy .......................................................................................................................... 1
1.
Contents ....................................................................................................................... 1
2.
Summary ...................................................................................................................... 2
3.
Equine Therapy............................................................................................................. 2
3.1 Background ............................................................................................................... 2
3.2 State of the literature ................................................................................................. 3
4.
Specific findings by disability ........................................................................................ 3
4.1 Autism Spectrum Disorder ......................................................................................... 3
4.2 Cerebral palsy ........................................................................................................... 4
Page 299 of 425
FOI 24/25- 0013
4.3 Multiple Sclerosis ....................................................................................................... 5
4.4 Stroke ........................................................................................................................ 5
4.5 Down Syndrome ........................................................................................................ 5
5.
References ................................................................................................................... 7
2. Summary
Equine therapy is defined as therapy completed in the presence of a horse, horse trainer and health
professional/therapist, and includes hippotherapy, therapeutic riding, and riding for rehabilitation, as
well as non-mounted tasks such as grooming and caring for the horse (Srinivasan et al, 2018).
It is proposed that hippotherapy and therapeutic horse riding promote neuromuscular and sensory
system development through rhythmic movements of the horse that mimic natural pelvis movement
during walking, and stimulate proprioceptive and balance reactions (Guindos-Sanchez et al, 2020;
Koca and Ataseven, 2015; Portaro et al, 2020; Zhao et al, 2021).
Improvement in social communication for children with ASD is the most commonly reported finding in
studies of equine therapy, postulated to be a response to verbal and non-verbal communication skil s
developed during equine therapy. However an umbrella review by Stern and Chur-Hansen (2019)
found that out of positive effects described in the literature for the social communication, behavioural
and motor domains, only effects in the behavioural domain were statistical y significant.
In general, findings for equine therapy across a range of conditions is equivocal due to methodological
weaknesses in the current literature (Stern and Chur-Hansen, 2019).
3. Equine Therapy
3.1 Background
Examination of the literature shows a range of terminology for the use of horses for therapeutic
purposes. Equine therapy is an overarching term for activities that are completed in the presence of a
horse, horse trainer and health professional/therapist, and includes hippotherapy, therapeutic riding,
and riding for rehabilitation, as well as non-mounted tasks such as grooming and caring for the horse
(Srinivasan et al, 2018). Health professionals involved in equine therapy may include a physiotherapist,
occupational therapist, speech therapist and/or psychotherapist depending on the patient’s goals and
therapeutic needs (Koca and Ataseven, 2015; McDaniel Peters and Wood, 2017). Equine assisted
activities may involve the same tasks however are not implemented by a health care professional (Tan
and Simmonds, 2018). This current paper only considers research involving equine therapy programs
that are implemented by a therapist with has specific goals and objectives for the participants.
Hippotherapy is defined as equine assisted therapy that uses the gait and movement of a horse to
provide motor and sensory input for physical, occupational or speech therapy goals (Koca and
Ataseven, 2015). This may involve a mechanical device mimicking horse motion or actual horse riding
(Silva et al, 2020). During hippotherapy, the horse or device lead the rider to stimulate anterior and
posterior swinging movements that mimic normal movements of the pelvis while walking. It is
Page 300 of 425
FOI 24/25- 0013
suggested that horse riding provides up to 110 postural deviations in one minute (Portaro et al, 2020),
which may stimulate proprioceptive and balance reactions (De Guindos-Sanchez et al, 2020).
Additionally, it is proposed the warmth and feel of the horse, along with rhythmic movements, provides
the rider with motor and sensory input to develop neuromuscular and sensory systems (Guindos-
Sanchez et al, 2020; Koca and Ataseven, 2015; Zhao et al, 2021).
Therapeutic riding builds on hippotherapy and may encompass additional functional domains, to
include cognitive, physical, emotional and social wellbeing goals (Lee et al, 2016). Importantly, during
therapeutic riding the rider has active control of the horse which may foster further development of
functional domains (Stern and Chur-Hansen, 2019). Other therapeutic options described in the
literature are equine assisted psychotherapy, which is implemented in conjunction with a mental health
practitioner, to focus on emotional growth and learning (Lee et al, 2016), and therapeutic carriage
driving, which may be a suitable option for individuals who cannot mount a horse (Stern and Chur-
Hansen, 2019).
3.2 State of the literature
There are many individual studies and reviews in the literature describing favourable effects of equine
therapy, despite heterogeneity in the data, on communication and language skil s, motor coordination,
muscle tone, postural balance, flexibility, gait and strength for a diverse range of conditions such as
cerebral palsy, Down syndrome, autistic spectrum disorder, stroke and multiple sclerosis (Koca and
Ataseven, 2015). Interestingly, an umbrella review (review of previous systematic reviews) published in
the Australian Journal of Psychology, found that evidence for equine assisted therapy for many
conditions is equivocal due to methodological weaknesses in the research (Stern and Chur-Hansen,
2019). In their opinion, this makes interpretation of the efficacy of equine therapy dif icult to determine
for some conditions based on the current state of the literature (Stern and Chur-Hansen, 2019). It is
important to note, however, that despite weaknesses in methodology limiting interpretation of group
effects of the intervention, there may stil be benefit to some individuals who undergo equine therapy,
therefore findings from the literature wil be discussed with respect to dif erent disabilities below.
4. Specific findings for different disabilities
4.1 Autism Spectrum Disorder
There is a large body of research evaluating the efficacy of equine therapy for minors with autism
spectrum disorder. Improvement in social functioning, including interaction, engagement and
communication, is the most commonly reported finding in the research (Srinivasan et al, 2018; Tzmiel
et al, 2019).
In a review by Srinivasan et al (2018) it was found 9 out of 11 studies reported improvement in social
skil s following equine intervention, 5 out of 7 studies demonstrated improvement in behavioural skil s
(e.g., stereotypical behaviours, affective responses, irritability, hyperactivity and self-regulation),
promising evidence for improvement in sensory skil s and only weak evidence for a positive effect on
motor skil s post equine therapy. This review was examined statistically by Stern and Chur-Hansen
(2019), who found there was only evidence of a positive significant effect for the behavioural domain
and the remainder were statistically non-significant.
Another review, undertaken by Tzmiel et al (2019), collated findings from 15 studies and found that
equine therapy may support psychosocial functioning for children and adolescents with ASD, however
they stated further research was warranted due to methodological differences between studies. In
particular, this review highlighted studies that found there was a decrease in maladaptive behaviour,
reduced hyperactivity and irritability, and lower levels of aggression and violent behaviour after
Page 301 of 425
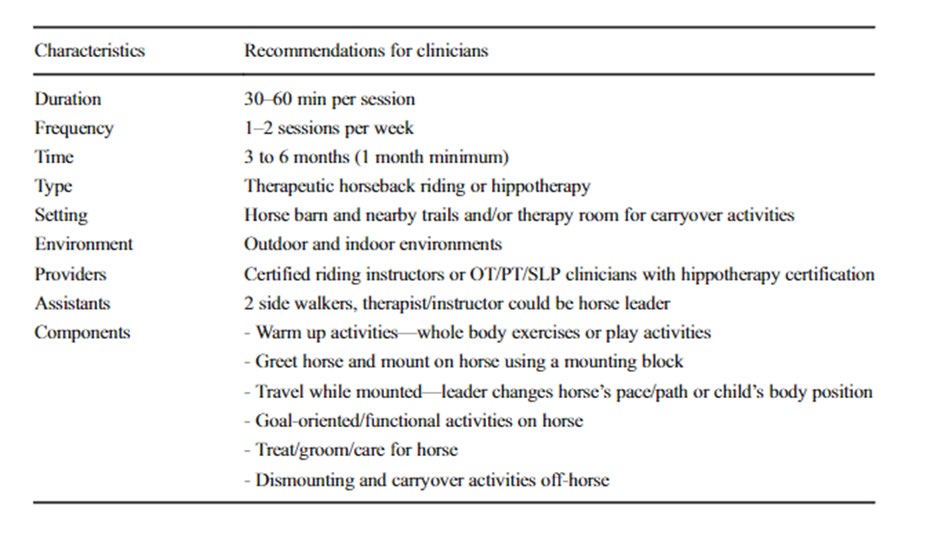
FOI 24/25- 0013
completing a therapeutic riding program (Anderson and Meints, 2016; Gabriels et al, 2012; Gomez et
al, 2017).
Individual findings by Holm et al (2014) suggested, after equine psychotherapy, that some challenging
or stereotypical behaviours may worsen during equine therapy sessions but demonstrated positive
effects afterwards in the home and community. They also found there was an increase in verbalisation
after equine therapy and an increased ability to follow directions, potentially as a result of needing to
follow directions successfully during equine therapy.
Only one study appeared to directly examine improvement in cognitive function. Borgi et al (2015)
demonstrated improved reaction time during problem solving activities after a therapeutic riding
program, and concluded this may reflect improved executive function abilities. Tan and Simmonds
(2018) also argued improvement in self-regulatory skil s may be linked to improved executive
functioning, sensory processing and emotional regulation, with these resulting in increased alertness,
focus, compliance and reduced emotional reactivity.
Srinivasan et al (2018) determined there was conflicting evidence regarding the long-term maintenance
of functional gains made after equine therapy had ceased, and Ward et al (2013) noted that consistent
therapeutic riding lessons were important to sustain functional gains. Despite this, Srinivasan et al
(2018) developed a protocol for equine therapy treatment based on the data from their review that they
proposed would generate the most positive outcomes (see Table 1).
Table 1
Proposed program for equine therapy for children with ASD (Srinivasan et al, 2018)
4.2 Cerebral palsy
Page 302 of 425
FOI 24/25- 0013
Literature describing equine therapy outcomes for children with cerebral palsy show a variety
of outcome measures and many dif erent measurement tools used (Stern and Chur-Hansen,
2019). The most frequently used tools to measure gross movement function – GMFM-88 and GMFM-
66 – show mixed results. Guindos-Sanchez et al (2020) undertook systematic review and meta-
analysis of 10 studies evaluating the efficacy of equine therapy on improvement in gross motor function
for children with cerebral palsy. Findings showed a favourable effect size for the subscales of ‘laying
and rolling’, ‘sitting’, and ‘walking, running and jumping’ (Guindos-Sanchez et al, 2020). Studies that
were included typically had equine therapy programs of 30-45mins; it was proposed that longer
durations may be associated with fatigue that counter the development of functional gains. Results of
the Guindos-Sanchez et al (2020) review concurred with Whalen and Case-Smith (2012) that also
found equine therapy was associated with improvements in gross motor function for children with
cerebral palsy. On the other hand, Stern and Chur-Hansen (2019) cite meta-analysis conducted by
Stergiou et al (2017) and Tseng et al (2013) that found no significant dif erences in gross motor
function after equine therapy for children with cerebral palsy.
4.3 Multiple Sclerosis
A small study conducted by Munoz-Lasa et al (2011) compared therapeutic riding with
traditional physiotherapy for adults with multiple sclerosis found that therapeutic riding group
experienced improvement in balance, decreased stride time and increased gait speed and
cadence. The control group did not demonstrate increased balance, and did not undergo gait
analysis for comparison.
The umbrella review by Stern and Chur-Hansen (2019) identified three systematic reviews
comprised of a total of 8 studies investigating the role of therapeutic riding for people with
multiple sclerosis. Al but one study that measured gait showed improvement following equine
therapy. Results were the same for balance. Of the other outcomes measured, including global
severity, health status, depression, speed/stride, postural stability/control, spasticity, mobility,
muscle tension, ground reaction force, fatigue, pain, disability, somatisation, quality of life, and
sway did not show improvement (Stern and Chur-Hansen, 2019).
4.4 Stroke
Stern and Chur-Hansen (2019) identified three systematic reviews (Stergiou et al, 2017;
White-Lewis et al, 2017; Wonsetler & Bowen, 2017) investigating the effect of therapeutic
riding for adults post-stroke, however this only included three unique studies. Analysis of these
reviews showed that after an equine therapy program, motor impairment in the lower limbs,
gait velocity, step length asymmetry and quality of life measures improved, while balance,
ambulance and cadence showed no change.
4.5 Down Syndrome
Two individual studies examining the efficacy of equine therapy for individuals with Down
Syndrome were sourced. Espindula et al (2016) used photogrammetry to demonstrate that
after hippotherapy, there was evidence of improvement in static posture, better alignment of
Page 303 of 425
FOI 24/25- 0013
shoulders, head, hip, lower limbs, decreased kyphosis and head protrusion, reflecting
improvement in motor behaviour. Additionally, Portaro et al (2020) found that after 6 months of
equine therapy, participants had better bilateral forefoot to hindfoot pressure distribution,
meaning greater stability during stance. They also identified a decrease in centre of pressure
and lower centre of pressure sway, indicating improved neuromotor systems relating to
stabilisation. Finally, they also found an increase in step length, velocity and width, to conclude
overall that hippotherapy resulted in functional improvement and increased stability for
individuals with Down Syndrome.
Page 304 of 425
FOI 24/25- 0013
5. References
Anderson, S., & Meints, K. (2016). Brief Report: The Effects of Equine-Assisted Activities on
the Social Functioning in Children and Adolescents with Autism Spectrum Disorder.
Journal of autism and developmental disorders, 46(10), 3344–3352.
https://doi.org/10.1007/s10803-016-2869-3
Borgi, M., Loliva, D., Cerino, S., Chiarotti, F., Venerosi, A., Bramini, M., Nonnis, E., Marcel i,
M., Vinti, C., De Santis, C., Bisacco, F., Fagerlie, M., Frascarel i, M., & Cirul i, F. (2016).
Effectiveness of a Standardized Equine-Assisted Therapy Program for Children with
Autism Spectrum Disorder. Journal of autism and developmental disorders, 46(1), 1–9.
https://doi.org/10.1007/s10803-015-2530-6
Espindula, A. P., Ribeiro, M. F., Souza, L. A. P. S. de, Ferreira, A. A., Ferraz, M. L. da F., &
Teixeira, V. de P. A. (2016). Effects of hippotherapy on posture in individuals with Down
Syndrome.
Fisioterapia Em Movimento,
29(3), 497–506. https://doi.org/10.1590/1980-
5918.029.003.ao07
Gabriels, R.L., Agnew, J.A., Holt, K.D., Shoffner, A., Zhaoxing, P., Ruzzano, S., Clayton, G.H.,
& Mesibov, G.B. (2012). Pilot study measuring the effects of therapeutic horseback
riding on school-age children and adolescents with autism spectrum disorders.
Research in Autism Spectrum Disorders, 6, 578-588.
Gómez, A.G., López-Risco, M., Jiménez, J.R., Guerrero, E.B., & Garcia-Peña, I.M. (2014).
Effects of a Program of Adapted Therapeutic Horse-Riding in a Group of Autism
Spectrum Disorder Children. Electronic Journal of Research in Educational Psychology,
12, 107-128.
Guindos-Sanchez, L., Lucena-Anton, D., Moral-Munoz, J. A., Salazar, A., & Carmona-
Barrientos, I. (2020). The Ef ectiveness of Hippotherapy to Recover Gross Motor
Function in Children with Cerebral Palsy: A Systematic Review and Meta-Analysis.
Children (Basel, Switzerland), 7(9), 106. https://doi.org/10.3390/children7090106
Holm, M. B., Baird, J. M., Kim, Y. J., Rajora, K. B., D'Silva, D., Podolinsky, L., Mazefsky, C., &
Minshew, N. (2014). Therapeutic horseback riding outcomes of parent-identified goals
for children with autism spectrum disorder: an ABA' multiple case design examining
dosing and generalization to the home and community. Journal of autism and
developmental disorders, 44(4), 937–947. https://doi.org/10.1007/s10803-013-1949-x
Koca, T. T., & Ataseven, H. (2016). What is hippotherapy? The indications and effectiveness
of hippotherapy. Northern clinics of Istanbul, 2(3), 247–252.
https://doi.org/10.14744/nci.2016.71601
Lee, P. T., Dakin, E., & McLure, M. (2016). Narrative synthesis of equine-assisted
psychotherapy literature: Current knowledge and future research directions. Health &
social care in the community, 24(3), 225–246. https:/ doi.org/10.1111/hsc.12201
Page 305 of 425
FOI 24/25- 0013
McDaniel Peters, B. C., & Wood, W. (2017). Autism and Equine-Assisted Interventions: A
Systematic Mapping Review. Journal of autism and developmental disorders, 47(10),
3220–3242. https:/ doi.org/10.1007/s10803-017-3219-9
Muñoz-Lasa, S., Ferriero, G., Valero, R., Gomez-Muñiz, F., Rabini, A., & Varela, E. (2011).
Effect of therapeutic horseback riding on balance and gait of people with multiple
sclerosis.
Giornale italiano di medicina del lavoro ed ergonomia,
33(4), 462–467.
Portaro, S., Cacciola, A., Naro, A., Caval aro, F., Gemel i, G., Aliberti, B., De Luca, R.,
Calabrò, R. S., & Milardi, D. (2020). Can Individuals with Down Syndrome Benefit from
Hippotherapy? An Exploratory Study on Gait and Balance. Developmental
neurorehabilitation, 23(6), 337–342. https://doi.org/10.1080/17518423.2019.1646830
Silva, S. B. C. Azevedo., Hruschka, A. C. C. B., Moraes, A. G., Leal, J. C., da Silva, M. L., &
Paz, L. (2021). Effectiveness of hippotherapy and therapeutic horseback riding on
balance in hemiparetic patients after stroke. Fisioterapia em Movimento, 34.
doi.org/10.1590/fm.2021.34201
Srinivasan, S. M., Cavagnino, D. T., & Bhat, A. N. (2018). Effects of Equine Therapy on
Individuals with Autism Spectrum Disorder: A Systematic Review. Review journal of
autism and developmental disorders, 5(2), 156–175. https://doi.org/10.1007/s40489-
018-0130-z
Stergiou, A., Tzoufi, M., Ntzani, E., Varvarousis, D., Beris, A., & Ploumis, A. (2017).
Therapeutic effects of horseback riding interventions: A systematic review and meta-
analysis. American Journal of Physical Medicine & Rehabilitation, 96(10), 717–725.
https://doi.org/10.1111/j.1469-8749.2007. 0175a.x
Stern, C., and Chur-Hansen, A. (2019). An umbrella review of the evidence for equine-assisted
interventions. Aust J Psychol, 71, 361– 374. https://doi.org/10.1111/ajpy.12246
Tan, V. X., & Simmonds, J. G. (2018). Parent Perceptions of Psychosocial Outcomes of
Equine-Assisted Interventions for Children with Autism Spectrum Disorder. Journal of
autism and developmental disorders, 48(3), 759–769. https:/ doi.org/10.1007/s10803-
017-3399-3
Trzmiel, T., Purandare, B., Michalak, M., Zasadzka, E., & Pawlaczyk, M. (2019). Equine
assisted activities and therapies in children with autism spectrum disorder: A systematic
review and a meta-analysis. Complementary therapies in medicine, 42, 104–113.
https://doi.org/10.1016/j.ctim.2018.11.004
Tseng, S. H., Chen, H. C., & Tam, K. W. (2013). Systematic review and metaanalysis of the
effect of equine assisted activities and therapies on gross motor outcome in children
with cerebral palsy. Disability and Rehabilitation, 35(2), 89–99.
https://doi.org/10.3109/09638288.2012.687033
Ward, S. C., Whalon, K., Rusnak, K., Wendel , K., & Paschall, N. (2013). The association
between therapeutic horseback riding and the social communication and sensory
Page 306 of 425
FOI 24/25- 0013
reactions of children with autism. Journal of autism and developmental disorders, 43(9),
2190–2198. https:/ doi.org/10.1007/s10803-013-1773-3
Whalen, C. N., & Case-Smith, J. (2012). Therapeutic effects of horseback riding therapy on
gross motor function in children with cerebral palsy: A systematic review. Physical &
Occupational Therapy in Pediatrics, 32(3), 229–242.
White-Lewis, S., Russell, C., Johnson, R., Cheng, A. L., & McClain, N. (2017). Equine-assisted
therapy intervention studies targeting physical symptoms in adults: A systematic review.
Applied Nursing Research, 38, 9–21. https:// doi.org/10.1016/j.apnr.2017.08.002
Wonsetler, E. C., & Bowden, M. G. (2017). A systematic review of mechanisms of gait speed
change post-stroke. Part 1: Spatiotemporal parameters and asymmetry ratios. Topics in
Stroke Rehabilitation, 24(6), 435–446. https:/ doi.org/10.1080/10749357.2017.1285746
Zhao, M., Chen, S., You, Y., Wang, Y., & Zhang, Y. (2021). Effects of a Therapeutic
Horseback Riding Program on Social Interaction and Communication in Children with
Autism. International journal of environmental research and public health, 18(5), 2656.
https://doi.org/10.3390/ijerph18052656
Page 307 of 425
FOI 24/25- 0013
DOCUMENT 29
Sensory-based therapy
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: Is sensory integration, modulation, processing all talking about the
same thing? Any other important terms to define?
Who might benefit from sensory support?
What is the evidence sensory support reduces the need for RRP?
What is the evidence for other more general outcomes?
Who might implement/qualifications for sensory support?
Date: 29/09/2022
Requestor: Karyn s22(1)(a)(ii)
- irrelevant
Endorsed by: Researcher: Stephanie s22(1)(a)(ii)
an
- irrelevant mate
d Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Stephanie s22(1)(a)(ii) - irrelevant mat
Review date:
Page 308 of 425
FOI 24/25- 0013
1. Contents
Sensory based interventions ...................................................................................................... 1
1.
Contents ....................................................................................................................... 2
2.
Summary ...................................................................................................................... 2
3.
Terminology .................................................................................................................. 3
3.1 Theoretical terminology ............................................................................................. 3
3.2 Types of sensory based interventions ....................................................................... 4
4.
Efficacy ......................................................................................................................... 7
4.1 Autism Spectrum Disorder ......................................................................................... 7
4.2 Mental Health ............................................................................................................ 9
4.3 Other conditions ...................................................................................................... 10
5.
References ................................................................................................................. 10
2. Summary
The terminology used in the literature on sensory disorder and sensory-based interventions
(SBIs) is inconsistent. The terms sensory integration, sensory processing and sensory
modulation are sometimes used interchangeably in the literature and sometimes given distinct
definitions. General features of these key terms can be described.
Researchers and clinicians have employed SBIs for a variety of conditions. Most of the
research available relates to interventions for Autism Spectrum Disorder (ASD) or other
neurodevelopmental disorders such as intellectual disabilities or attention deficit/hyperactivity
disorder, schizophrenia or other mental health conditions such a bipolar, depression or
obsessive-compulsive disorder. There is also research relating to interventions for cerebral
palsy, Huntington’s disease and dementia.
There is some evidence that SBIs can contribute to a reduction in restrictive practice. The
evidence is predominantly in the domain of mental health and is predominantly related to
restrictive practice in a clinical or institutional setting. However, systematic reviews show
inconsistent results. Based on the evidence collected it is not possible to say with confidence
that SBIs reduce the use of restrictive practice. There are many factors which contribute to an
institution’s use of restrictive practice that are not addressed by the introduction of SBIs.
SBIs do likely have some positive effects. There is consistent evidence that SBIs reduce
distress of people with mental health conditions and lower quality evidence that distress is
reduced for people with Huntington’s disease and dementia. There is low to moderate quality
evidence of positive effect for young people with ASD relating to some core autistic
characteristics, life outcomes and cognitive, motor and social-emotional skills. There is weak
Page 309 of 425
FOI 24/25- 0013
evidence showing improvement in functional outcomes for children with intellectual disability
and development delay.
SBIs are usually implemented by an occupational therapist. However, other professionals can
be trained to implement SBIs including nurses, psychologists and speech therapists.
3. Terminology
The literature on sensory therapies is not well organised and key terminology is not used
consistently (Ouellet et al, 2021). However, rough definitions of the major concepts are
possible.
3.1 Theoretical terminology
Underlying theoretical terms are often used in different ways. Brown et al (2019) provide an
overview of the use of the terms
sensory integration,
sensory processing, sensory
modulation and
sensory perception, showing that despite considerable variation, these
terms
have also been used interchangeably in the literature. Based on their review, the
authors propose the following definition of sensory modulation:
Sensory modulation is considered a twofold process. It originates in the central nervous
system as the neurological ability to regulate and process sensory stimuli; this
subsequently offers the individual an opportunity to respond behaviourally to the
stimulus (Brown et al, 2019, p.521).
They characterise sensory modulation as a combined neurophysiological and behavioural
process within the larger category of sensory processing. Sensory processing also includes:
receiving, organisation, perception, interpretation, registration and discrimination. They
suggest sensory integration is the framework which encompasses the sensory processing sub-
processes and the disorders associated with those subtypes (Brown et al, 2019).
However, we should also recognise that the process of proposing consistent definitions of
these terms is largely revisionary considering the disagreement in the literature. For instance,
sensory integration can refer to a neurological process, a theory or a practice depending on
the researcher. Sensory processing might be used interchangeably with sensory integration
(Camarat et al, 2020; Brown et al, 2019). Sensory processing is more often used in the
literature related to autism, but sensory modulation is often used in the literature on mental
health to refer to the same types of interventions (Brown et al, 2019; Hitch et al, 2020).
There is inconsistency in the definitions of sensory disorders as well. Diagnosis is made based
on the presence of i) difficulties translating sensory information into appropriate behavioural
responses and; ii) a demonstrable effect on activities of daily living (Ouellet, 2021). There is
some controversy about whether sensory disorders are genuinely separate conditions or
whether they are collections of symptoms associated with other conditions. The category of
sensory disorders is not included in either the DSM-5 or the ICD-11 (American Psychiatric
Association, 2013; World Health Organisation, 2019).
Page 310 of 425
FOI 24/25- 0013
3.2 Types of sensory based interventions
Terms for therapeutic practices are also used in incompatible ways (Ouellet et al, 2021). In
particular, there is an ambiguity in the use of the term
sensory based interventions.
SBI can refer to a category of therapeutic techniques that include sensory integration therapy
(SIT), auditory integration therapy (AIT), use of multi-sensory environments (MSE) and other
techniques that target sensory processing difficulties. Preis and McKenna (2014) and
Whitehouse et al (2020) use SBI in this way.
However, SBI can also refer to specific practices that are distinguished from SIT, AIT or MSE.
Ouellet et al (2021), Basic et al (2021) and Wans Yunus et al (2015) draw the distinction
between SIT and SBI based on the number of therapeutic modalities or stimuli. SBI is used to
refer to techniques that use singular discrete stimuli to achieve the desired result (e.g.,
massage, a weighted vest). SIT on the other hand, uses multiple integrated stimuli and must
include more than one sensory modality (Parham et al, 2007).
McGil and Breen (2019) note a further complication: SBI-type strategies are emerging in the
context of positive behaviour support and multi-element behavioural interventions without
being labelled as SBIs.
There does seem to be agreement that SBIs are based on the theoretical premise that sensory
processing differences affect skil acquisition and behavioural development. By targeting
sensory processing, the interventions aim to improve behavioural problems, emotional
regulation, cognitive, language and social skil s (Whitehouse et al, 2020).
Discrete SBIs, SIT, MSE and AIT are considered in further detail below. There are other
therapeutic practices that can be included under the label SBI. Whitehouse et al also consider
environmental enrichment, sensory diet and the following:
alternative seating; blanket or “body sock”; brushing with a bristle or a feather; chewing
on a rubber tube; developmental speech and language training through music; family-
centered music therapy; joint compression or stretching; jumping or bouncing; music
therapy; playing with a water and sand sensory table; playing with specially textured
toys; Qigong Sensory Treatment (QST); Rhythm Intervention Sensorimotor Enrichment;
sensory enrichment; swinging or rocking stimulation; Thai traditional massage; Tomatis
Sound Therapy; and weighted vests (Whitehouse et al, 2020, p.70).
SBIs are usually implemented by occupational therapists, although speech therapists, nurses,
psychologists and other professionals can be trained to implement programs (McGil & Breen,
2019).
3.2.1 Sensory-based interventions
SBI provides sensory stimuli that are specific or discrete to address behavioural problems
causes by dif iculties in sensory processing (Wan Yunus, 2015; Ouellet et al, 2021). The
distinction between sensory-based and sensorimotor-based approaches is drawn differently in
the literature. Ouellet et al (2021) says that sensory-based approaches involve a stimulus of
Page 311 of 425
FOI 24/25- 0013
constant intensity, such as a weighted vest, whereas sensorimotor-based approaches include
the use of movements, allowing the person to control the quantity and intensity of stimulation.
In contrast, Wan Yunus et al (2015) distinguish between tactile (eg. massage, touch therapy,
brushing), proprioceptive (eg. weighted vests) and vestibular (eg. therapy ball, cushions, horse
riding) based interventions. Vestibular interventions involve patient movements and variation in
the constancy of intensity of stimulus was not noted as a distinguishing feature of different
techniques.
3.2.2 Sensory integration therapy
Sensory integration therapy (sometimes sensory processing therapy) is defined as any
intervention that targets someone’s “ability to integrate sensory information (visual, auditory,
tactile, proprioceptive, and vestibular) from their body and environment in order to respond
using organized and adaptive behaviour” (Steinbrenner et al, 2020, p.29). Steinbrenner et al
(2020) regard SIT as synonymous with Ayers Sensory Integration (Ayers). Whereas Omairi et
al (2022) treat Ayers as just one frequently used type of SIT.
Ayers can include equipment such as mats, swings, scooter boards and bolsters in
“individually tailored sensorimotor activities that are contextualized in play at the just-right
challenge to facilitate adaptive behaviours for participation in tasks and activities” (Omairi et al,
2022, p.4; Whitehouse et al, 2020). There are 10 core elements of Ayers:
• Provide sensory opportunities – intervention includes various sensory experiences
(tactile, proprioceptive, vestibular) involving more than one sensory modality.
• Provide just-right challenges – sensory challenges are neither too dif icult nor too
easy for the individual
• Collaborate on activity choice – the participant is an active contributor to the
intervention including choice of activity
• Guide self-organisation – participant is encouraged to initiate, plan and organise
their own activities
• Support optimal arousal – the context should allow the child to maintain their optimal
level of arousal
• Create play context – the context builds on the participants intrinsic motivation and
enjoyment of activities
• Maximise child’s success – activities are tailored so that the child can experience
success
• Ensure physical safety – activities are tailored so that the child is safe and properly
supervised
Page 312 of 425

FOI 24/25- 0013
• Arrange room for engagement – the environment is organised to motivate the
participant to participate in activities
• Foster therapeutic alliance – the participant is treated with respect and allowed to
have their own emotional reactions to experiences (Parham et al, 2007; Wans
Yunus et al, 2015; Whitehouse et al, 2020).
3.2.3 Multi-sensory environment
MSEs (also called comfort rooms, sensory rooms or Snoezelen rooms) are rooms that contain
equipment used to modify the environment primarily with the aim to create sensory
experiences. This includes equipment used to create lights, sounds, smells or proprioceptive
and tactile sensations. The goal of an MSE is to soothe or stimulate a person with sensory
needs (Unwin et al, 2022; Cameron et al, 2020).
Figure 1 Multi-sensory room
MSEs are often windowless or have covered walls. They commonly include:
(1) projection equipment to provide changing light colours and patterns, (2) sound
(music) equipment, (3) bubble tubes offering visual, audible and tactile stimulation, (4)
waterbed, (5) fibre optic lighting, (6) tactile objects, (7) user-controlled switching for
changing lighting and other equipment, (8) weighted blankets, (9) self-massagers, (10)
rocking chair(s), (11) exercise balls, and (12) squeeze balls (Cameron et al, 2020,
p.631).
Rooms might also include essential oils, scented candles, sweet or salty foods (Cameron et al,
2020). Participants can control aspects of the environment thereby reducing the
unpredictability or the environment and allowing the participant to regulate their own sensory
stimulation (Unwin et al, 2022).
Page 313 of 425
FOI 24/25- 0013
3.2.4 Auditory integration training
AIT aims to ‘re-educate’ the auditory processing system of the patient’s brain with 2 half hour
electronic music listening sessions over 10 days. This re-education process is intended to
target behaviour and learning problems in people with autism (Sinha et al, 2011).
Wans Yunus et al (2015) suggest auditory integration training (AIT) is a based on the same
theory of sensory integration as SIT. However, because SIT involves multiple sensory
modalities (Parham et al, 2007), AIT can only be considered a related therapy rather than a
kind of SIT. Other related techniques include Tomatis sound therapy and Samonas sound
therapy (Sinha et al, 2011).
3.2.5 Music therapy
Music therapy is considered a type of SBI by some (Whitehouse et al, 2020; Cheung et al,
2022) and not others (Steinbrenner et al, 2020). The mechanism by which music therapy is
supposed to work does involve active listening and auditory sensory experiences, though it
also includes social and cognitive processes (Geretsegger et al, 2014).
4. Efficacy
Researchers and clinicians have suggested that sensory based interventions could benefit
people with autism spectrum disorder, ADHD, developmental coordination disorder, cerebral
palsy, down syndrome, intellectual disability, dementia, depression, schizophrenia, mood
disorders, obsessive compulsive disorder (Wan Yunus et al, 2015; Sinha et al, 2011; Hitch et
al, 2020; Ouellet et al, 2021).
4.1 Autism Spectrum Disorder
Steinbrenner et al (2020) and Whitehouse et al (2020) consider sensory-based interventions in
their reviews of evidence-based treatments for young people with ASD.
Steinbrenner et al added Ayers to their 2020 review of evidence-based practices for children
and young people with autism spectrum disorder. They note evidence of effect on
communication, social skil s, cognitive and academic outcomes, adaptive coping skil s,
challenging behaviour, and motor skil s (Steinbrenner et al, 2020). However, Steinbrenner et al
did not assess the evidence for ef icacy in detail, but only show that Ayers meet their criteria
for being considered an evidence-based practice:
To be identified as evidence-based, a category of practice had to contain (a) two high
quality group design studies conducted by two different research groups, or (b) five high
quality single case design studies conducted by three different research groups and
involving a total of 20 participants across studies, or (c) a combination of one high
quality group design study and three high quality single case design studies with the
combination being conducted by two independent research groups (Steinbrenner et al,
2020, p.24).
Page 314 of 425
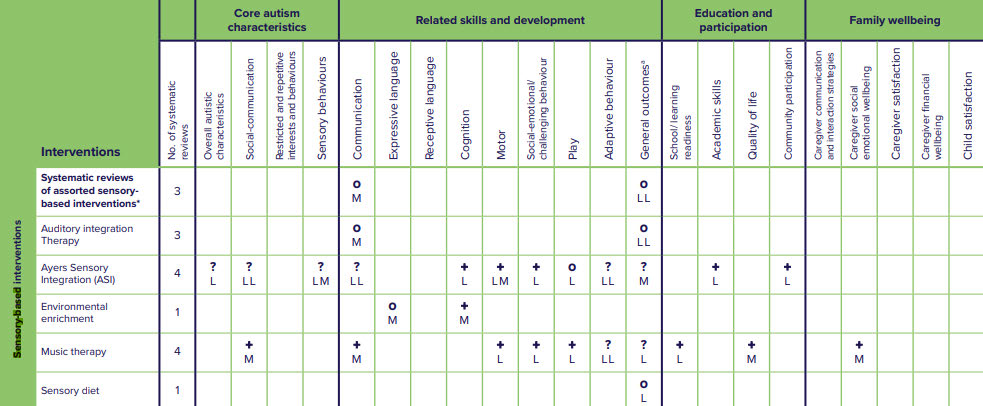
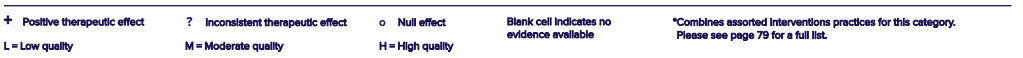
FOI 24/25- 0013
Whitehouse et al (2020) considered 9 systematic reviews. No evidence was found of a positive
effect for assorted SBIs, AIT or sensory diet. Environmental enrichment showed a positive
effect on motor skil s based on moderate quality evidence.
Ayers was considered in 4 reviews which showed low quality evidence of improvement to
cognition, motor skil s, challenging behaviours, academic skil s and community participation.
Reviewers also found moderate quality evidence of a benefit to motor skil s. Low or moderate
quality evidence showed inconsistent or null effect on autistic characteristics such as social-
communication and sensory behaviours, communication skil s, play, adaptive behaviour skil s,
and general outcomes. 1 review found evidence that SIT may contribute to increase in
stereotypical and problem behaviours (Whitehouse et al, 2020).
Music therapy demonstrated the most consistent positive effect. Reviewers found moderate
quality evidence showing positive effect on social-communication symptoms, communication
skills, and quality of life. Reviewers found low quality evidence showing positive effect on play,
motor skil s, challenging behaviours, and school readiness (Whitehouse et al, 2020).
Figure 2 Summary of evidence for sensory-based interventions. From Whitehouse et al, 2020, p.75
Wan Yunus et al (2015) argue that there is sufficient evidence that tactile stimulation (such as
massage therapy) positively affects challenging behaviours such that it can be included in
clinical practice. This contrasts with both Whitehouse et al (2020) and Steinbrenner et al
(2020) who note evidence that Ayers and music therapy can improve challenging behaviours,
but who do not recognise evidence that discrete tactile stimulation can improve challenging
behaviours.
Page 315 of 425
FOI 24/25- 0013
4.2 Mental Health
Sensory profiles of people with mental health conditions differ from the norm. Brown et al
(2020) found a general pattern of greater sensory sensitivity, sensation avoiding, and low
registration and less sensation seeking in a group of patients with either schizophrenia, high
risk for psychosis, bipolar disorder, major depressive disorder, posttraumatic stress and
obsessive-compulsive. Machingura et al (2022) confirmed higher rates of low registration and
sensory avoiding in a group of 41 people with schizophrenia.
SBIs are currently in use in mental health settings in Australia, including discrete SBIs and
MSEs. While the evidence base is stil emerging, existing studies consistently find an effect of
SBIs on distress. Multiple systematic reviews over the past 10 years have concluded that SBIs
are likely to contribute to a reduction in distress for patients with mental health issues in clinical
settings (Scanlon & Novak, 2015; Hitch et al, 2020; McGreevy & Boland, 2020; Ma et al, 2021;
Hain & Hallet, 2022). In a recent controlled trial, Machingura et al (2022) found a reduction in
distress for patients with schizophrenia when comparing pre- and post-test scores. However,
the effect was no longer statistically significant when compared with the control group.
SBIs are hypothesised to reduce the use of restrictive practice. State and national policies
aiming to reduce the use of restrictive practice are driving adoption of and research into SBIs
(Machingura et al, 2022; Baker et al, 2022; Baker et al, 2021; Hitch et al, 2020). The
suggestion is that if SBIs can reduce distress and level of arousal, then fewer episodes
requiring restrictive practice would occur. However, this assumption is questionable
considering the effect of workplace culture and institutional/state policy on rates of restrictive
practices (Scanlon & Novak, 2015). The evidence for an actual reduction in use of restrictive
practice is mixed.
Scanlon and Novak (2015) reviewed 17 papers and found that of the 9 studies reporting only
rates of restrictive practice use, all were using MSE type interventions. Of those studies 5
reported a reduction in rates of restraint or seclusion, 3 reported no change and 1 reported an
increase.
Other systematic reviews also show inconsistent evidence that MSEs used in clinical or
institutional settings can reduce restrictive practice. Haig and Hallett (2022) reviewed 6 studies
which reported rates or seclusion, restraint or violence. 4 of the 6 reported any positive results:
one out 6 studies found a reduction in seclusion episodes, 2 out of 6 found reductions in
restraint and 1 out of 6 found a reduction in aggression. One study also found an increase in
rates of seclusion. Haig and Hallett also note that all the studies reviewed had moderate to
high risk of bias.
Oostermeijer et al (2021) completed a rapid review including 14 studies on the effect of MSEs
on restrictive practices and found more positive results: 6 of the 14 studies found reduction in
restraint; 10 of the 14 found reduction in seclusion; 3 of the 14 reported no statistically
significant results; and 3 of the 14 reported an increase in restraint or seclusion.
Page 316 of 425
FOI 24/25- 0013
None of the systematic reviews were able to complete a meta-analysis. The inconsistency of
the evidence regarding MSEs effect on restrictive practice may relate to the unstructured and
heterogeneous nature of the intervention. There may be effective MSE-based practices or
protocols but existing studies have not identified them (Oostermeijer et al, 2021; Haig &
Hallett, 2022).
Most research on SBIs for people with mental health conditions occurs in a clinical or
institutional setting. Lack of research in community use of SBIs is a significant limitation of the
existing research (Hitch et al, 2020).
Hitch et al (2020) argue that despite minimal evidence, there is at least sufficient evidence to
support wider use in clinical settings due to minimal cost of implementation of many sensory
based interventions (for example, the discrete SBIs described in 3.2.1 Sensory-based
interventions).
4.3 Other conditions
There is some evidence that SBIs (especially MSEs, massage and music therapy) can
contribute to reduction in distress and agitation for people with dementia (Livingston et al,
2014; Pinto et al, 2020; Cheung et al, 2022).
Fisher et al (2014; 2017) show minimal evidence that SBI can reduce aggression in people
with Huntington’s disease.
Kantor et al (2022) found positive effects of Ayers on motor skil s of children with cerebral
palsy. However, better quality evidence is required to draw reliable conclusions.
A 2015 meta-analysis found only weak evidence for the efficacy of SIT in improving functional
outcomes for children with intellectual disability and development delay (Leong et al, 2015).
Subsequent studies have shown that SIT can assist children with developmental delay when
combined with a more comprehensive early intervention program (Wang et al, 2020).
5. References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental
disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Baker, J., Berzins, K., Canvin, K., Benson, I., Kel ar, I., Wright, J., Lopez, R. R., Duxbury, J.,
Kendall, T., & Stewart, D. (2021). Non-pharmacological interventions to reduce
restrictive practices in adult mental health inpatient settings: the COMPARE systematic
mapping review.
Health Services and Delivery Research,
9(5), 1–184.
https://doi.org/10.3310/hsdr09050
Baker, J., Berzins, K., Canvin, K., Kendal, S., Branthonne-Foster, S., Wright, J., McDougal , T.,
Goldson, B., Kellar, I., & Duxbury, J. (2022). Components of interventions to reduce
restrictive practices with children and young people in institutional settings: the Contrast
Page 317 of 425
FOI 24/25- 0013
systematic mapping review.
Health and Social Care Delivery Research,
10(8), 1–180.
https://doi.org/10.3310/yvkt5692
Basic, A., Macesic Petrovic, D., Pantovic, L., Zdravkovic Parezanovic, R., Gajic, A., Arsic, B.,
Nikolic, J. (2021). Sensory integration and activities that promote sensory integration in
children with autism spectrum disorders.
Journal Human Research in Rehabilitation,
11(1), 28–38. https://doi.org/10.21554/hrr.042104
Brown, A., Tse, T., & Fortune, T. (2019). Defining sensory modulation: A review of the concept
and a contemporary definition for application by occupational therapists.
Scandinavian
Journal of Occupational Therapy,
26(7), 515–523.
https://doi.org/10.1080/11038128.2018.1509370
Brown, C., Karim, R., & Steuter, M. (2020). Retrospective analysis of studies examining
sensory processing preferences in people with a psychiatric condition.
The American
Journal of Occupational Therapy: Official Publication of the American Occupational
Therapy Association,
74(4), 7404205130p1-7404205130p11.
https://doi.org/10.5014/ajot.2020.038463
Cameron, A., Burns, P., Garner, A., Lau, S., Dixon, R., Pascoe, C., & Szafraniec, M. (2020).
Making sense of multi-sensory environments: A scoping review.
International Journal of
Disability, Development, and Education,
67(6), 630–656.
https://doi.org/10.1080/1034912x.2019.1634247
Cheung, D. S. K., Wang, S. S., Li, Y., Ho, K. H. M., Kwok, R. K. H., Mo, S. H., & Bressington,
D. (2022). Sensory-based interventions for the immediate de-escalation of agitation in
people with dementia: A systematic review.
Aging & Mental Health, 1–12.
https://doi.org/10.1080/13607863.2022.2116404
Fisher, C. A., Sewell, K., Brown, A., & Churchyard, A. (2014). Aggression in Huntington’s
disease: a systematic review of rates of aggression and treatment methods.
Journal of
Huntington’s Disease,
3(4), 319–332. https:/ doi.org/10.3233/JHD-140127
Fisher, C. A., & Brown, A. (2017). Sensory modulation intervention and behaviour support
modification for the treatment of severe aggression in Huntington’s disease. A single
case experimental design.
Neuropsychological Rehabilitation,
27(6), 891–903.
https://doi.org/10.1080/09602011.2015.1091779
Geretsegger, M., Elefant, C., Mössler, K. A., & Gold, C. (2014). Music therapy for people with
autism spectrum disorder.
Cochrane Database of Systematic Reviews,
2016(6),
CD004381. https://doi.org/10.1002/14651858.CD004381.pub3
Haig, S., & Hallett, N. (2022). Use of sensory rooms in adult psychiatric inpatient settings: A
systematic review and narrative synthesis.
International Journal of Mental Health
Nursing. https:/ doi.org/10.1111/inm.13065
Hitch D, Wilson C, Hillman A. (2020) Sensory modulation in mental health practice. Mental
Health Practice. https:/ doi.org/10.7748/mhp.2020.e1422
Page 318 of 425
FOI 24/25- 0013
Kantor, J., Hlaváčková, L., Du, J., Dvořáková, P., Svobodová, Z., Karasová, K., & Kantorová,
L. (2022). The effects of Ayres sensory integration and related sensory based
interventions in children with cerebral palsy: A scoping review.
Children (Basel,
Switzerland),
9(4), 483. https://doi.org/10.3390/children9040483
Leong, H. M., Carter, M., & Stephenson, J. R. (2015). Meta-analysis of research on sensory
integration therapy for individuals with developmental and learning disabilities.
Journal
of Developmental and Physical Disabilities,
27(2), 183–206.
https://doi.org/10.1007/s10882-014-9408-y
Livingston, G., Kelly, L., Lewis-Holmes, E., Baio, G., Morris, S., Patel, N., Omar, R. Z., Katona,
C., & Cooper, C. (2014). A systematic review of the clinical effectiveness and cost-
effectiveness of sensory, psychological and behavioural interventions for managing
agitation in older adults with dementia.
Health Technology Assessment (Winchester,
England),
18(39), 1–226, v–vi. https://doi.org/10.3310/hta18390
Ma, D., Su, J., Wang, H., Zhao, Y., Li, H., Li, Y., Zhang, X., Qi, Y., & Sun, J. (2021). Sensory-
based approaches in psychiatric care: A systematic mixed-methods review.
Journal of
Advanced Nursing,
77(10), 3991–4004. https://doi.org/10.1111/jan.14884
Machingura, T., Shum, D., Lloyd, C., Murphy, K., Rathbone, E., & Green, H. (2022).
Effectiveness of sensory modulation for people with schizophrenia: A multisite
quantitative prospective cohort study.
Australian Occupational Therapy Journal,
69(4),
424–435. https://doi.org/10.1111/1440-1630.12803
McGil , C., & Breen, C. J. (2020). Can sensory integration have a role in multi‐element
behavioural intervention? An evaluation of factors associated with the management of
challenging behaviour in community adult learning disability services.
British Journal of
Learning Disabilities,
48(2), 142–153. https:/ doi.org/10.1111/bld.12308
McGreevy, S., & Boland, P. (2020). Sensory-based interventions with adult and adolescent
trauma survivors: An integrative review of the occupational therapy literature.
Irish
Journal of Occupational Therapy,
48(1), 31–54. https://doi.org/10.1108/ijot-10-2019-
0014
Omairi, C., Mail oux, Z., Antoniuk, S. A., & Schaaf, R. (2022). Occupational therapy using
Ayres Sensory Integration®: A randomized controlled trial in Brazil.
The American
Journal of Occupational Therapy: Official Publication of the American Occupational
Therapy Association,
76(4). https://doi.org/10.5014/ajot.2022.048249
Oostermeijer, S., Brasier, C., Harvey, C., Hamilton, B., Roper, C., Martel, A., Fletcher, J., &
Brophy, L. (2021). Design features that reduce the use of seclusion and restraint in
mental health facilities: a rapid systematic review.
BMJ Open,
11(7), e046647.
https://doi.org/10.1136/bmjopen-2020-046647
Ouellet, B., Carreau, E., Dion, V., Rouat, A., Tremblay, E., & Voisin, J. I. A. (2021). Efficacy of
sensory interventions on school participation of children with sensory disorders: A
Page 319 of 425
FOI 24/25- 0013
systematic review.
American Journal of Lifestyle Medicine,
15(1), 75–83.
https://doi.org/10.1177/1559827618784274
Parham, L. D., Cohn, E. S., Spitzer, S., Koomar, J. A., Mil er, L. J., Burke, J. P., Brett-Green,
B., Mail oux, Z., May-Benson, T. A., Roley, S. S., Schaaf, R. C., Schoen, S. A., &
Summers, C. A. (2007). Fidelity in sensory integration intervention research.
The
American Journal of Occupational Therapy: Official Publication of the American
Occupational Therapy Association,
61(2), 216–227.
https://doi.org/10.5014/ajot.61.2.216
Pinto, J. O., Dores, A. R., Geraldo, A., Peixoto, B., & Barbosa, F. (2020). Sensory stimulation
programs in dementia: a systematic review of methods and effectiveness.
Expert
Review of Neurotherapeutics,
20(12), 1229–1247.
https://doi.org/10.1080/14737175.2020.1825942
Preis, J., & McKenna, M. (2014). The effects of sensory integration therapy on verbal
expression and engagement in children with autism.
International Journal of Therapy
and Rehabilitation,
21(10), 476–486. https://doi.org/10.12968/ijtr.2014.21.10.476
Scanlan, J. N., & Novak, T. (2015). Sensory approaches in mental health: A scoping review.
Australian Occupational Therapy Journal,
62(5), 277–285. https://doi.org/10.1111/1440-
1630.12224
Sinha, Y., Silove, N., Hayen, A., & Wil iams, K. (2011). Auditory integration training and other
sound therapies for autism spectrum disorders (ASD).
Cochrane Database of
Systematic Reviews,
12, CD003681. https://doi.org/10.1002/14651858.CD003681.pub3
Steinbrenner, J. R., Hume, K., Odom, S. L., Morin, K. L., Nowel , S. W., Tomaszewski, B.,
Szendrey, S., McIntyre, N. S., Yücesoy-Özkan, S., & Savage, M. N. (2020). Evidence-
based practices for children, youth, and young adults with Autism. The University of
North Carolina at Chapel Hil , Frank Porter Graham Child Development Institute,
National Clearinghouse on Autism Evidence and Practice Review Team.
Unwin, K. L., Powell, G., & Jones, C. R. (2022). The use of Multi-Sensory Environments with
autistic children: Exploring the effect of having control of sensory changes.
Autism: The
International Journal of Research and Practice,
26(6), 1379–1394.
https://doi.org/10.1177/13623613211050176
Wan Yunus, F., Liu, K. P. Y., Bissett, M., & Penkala, S. (2015). Sensory-based intervention for
children with behavioral problems: A systematic review.
Journal of Autism and
Developmental Disorders,
45(11), 3565–3579. https:/ doi.org/10.1007/s10803-015-
2503-9
Wang, L.-J., Hsieh, H.-Y., Chen, L.-Y., Ko, K.-L., Liu, H.-H., Chou, W.-J., Chou, M.-C., & Tsai,
C.-S. (2020). Adjunctive sensory integration therapy for children with developmental
disabilities in a family-based early intervention program.
Taiwanese Journal of
Psychiatry,
34(3), 121. https://doi.org/10.4103/tpsy.tpsy 26 20
Page 320 of 425
FOI 24/25- 0013
Whitehouse, A., Varcin, K., Waddington, H., Sulek, R., Bent, C., Ashburner, J., Eapen, V.,
Goodall, E., Hudry, K., Roberts, J., Silove, N., Trembath, D. (2020). Interventions for
children on the autism spectrum: A synthesis of research evidence. Autism CRC,
Brisbane
World Health Organization. (2019). ICD-11: International classification of diseases (11th
revision). https://icd.who.int/
Page 321 of 425
FOI 24/25- 0013
DOCUMENT 30
Pet ownership and mental health
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: What evidence is there that pet ownership can support mental health
and wellbeing of people with psychosocial disability diagnoses or symptoms of anxiety,
depression or trauma?
Date: 28/10/2022
Requestor: Olivia s22(1)(a)(ii) - irrele
Endorsed by: n/a
Researcher: Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Stephanie s22(1)(a)(ii) - irrelevant mat
1. Contents
Pet ownership and mental health ............................................................................................... 1
1.
Contents ....................................................................................................................... 1
2.
Summary ...................................................................................................................... 2
3.
Definitions ..................................................................................................................... 2
4.
Pet ownership ............................................................................................................... 4
5.
Health and well-being of pet owners ............................................................................. 6
5.1 Perception of benefit .................................................................................................. 6
5.2 Social interaction ....................................................................................................... 6
5.3 Mental health ............................................................................................................. 7
Page 322 of 425
FOI 24/25- 0013
5.4 Physical health .......................................................................................................... 8
6.
References ................................................................................................................... 9
2. Summary
Physiological, demographic and personality characteristics of both the human and the pet, as
well as the duration and quality of the hauuman-pet relationship, may affect how pet ownership
influences the health and well-being of the human. Currently, the evidence-base for human-pet
interaction is not sufficient to determine how these different variables affect the health and
well-being of the human.
Researchers consistently point out limitations with the current literature on human-pet
interaction, including problems with study design such as low sample sizes and failure to
control for confounding variables. The heterogeneity of study designs, inconsistent or vague
definitions of key concepts and outcome measures also prevents the establishment of a
reliable evidence base.
For these reasons it is not possible to say whether, when or how a pet will benefit someone
with mental health challenges.
Note: This paper has focussed on the literature describing mental health benefits of pets or
companion animals, rather than literature regarding emotional support animals. Emotional
support animals are recognised by a health professional to provide a benefit to a person with
mental health difficulties. It is possible that different results may be obtained by studies looking
at confirmed emotional support animals. As emotional support animals don’t require special
training, they may ultimately be a family pet with whom the owner has the right kind of positive
relationship. This area wil need to be researched further before any conclusions can be
drawn.
This paper relates primarily to pet or companion animal ownership. The TAB Tactical
Research team has completed three other papers related more specifically to assistance
animals:
• RES 183 Therapy Animals: Models of practice for ending involvement in therapy
programs
• RES 238 Accreditation of assistance animals
• RES 239 Animal assisted therapy.
3. Definitions
There is no widely agreed upon definition of ‘pet’ or ‘companion animal’. Explicit definitions are
rarely provided in the literature (Miklosi et al, 2021; Rodriguez et al, 2021; Barroso et al, 2021).
None of the four available Animal Medicines Australia reports define a pet (refer to 4. Pet
Page 323 of 425
FOI 24/25- 0013
ownership). Where the terms companion animal and pet are defined, the definitions can be
idiosyncratic. Kretzler et al use the Oxford English Dictionary definition, “an animal (typically
one which is domestic or tame) kept for pleasure or companionship” (Kretzler et al, 2022,
p.1935). RSPCA uses the terms pet and companion animal interchangeably and distinguishes
the companion animal from an animal used for farming, research, sport or entertainment
(RSPCA, 2018). Sandoe et al (2015) consider pets to be domesticated non-human animals
living inside the home, while they consider companion animals to be a specific kind of pet.
Companionship is said to involve reciprocal social interaction between human and pet. Miklosi
et al (2021) take this further, removing any other consideration (domestication, living inside the
home) and arguing that any animal can be a companion animal so long as the right kind of
relationship exists between it and a human. In contrast, the NSW state legislation treats all
dogs and cats as companion animals, regardless of the relationship with their owner:
The fact that an animal is not strictly a “companion” does not prevent it being a
companion animal for the purposes of this Act. Al dogs are treated as companion
animals, even working dogs on rural properties, guard dogs, police dogs and corrective
services dogs (
Companion Animals Act 1988 (NSW), s. 5.1).
Farrell and Crowley (2021) provide a discussion in the US context. Their focus is emotional
support animals, but their discussion is instructive for our purposes as well. Emotional support
animals, they say, are a kind of assistance animal, a category that includes service animals
and therapy animals. An emotional support animal is distinguished from the other two as it
does not have any special training and is not used in any specific therapy. An animal is an
emotional support animal when it is needed by a person with a mental health condition to
alleviate a symptom or effect of disability. This means a pet could be an emotional support
animal if it is needed to provide this function.
These differences can be important, especially since researchers generally don’t make their
definition explicit. For example, for Sandoe et al (2015) horses can’t be pets if they live in a
stable and spiders, insects and fish can be pets but not companion animals because they are
unlikely to meet the threshold for a significant degree of social interaction. The NSW state
legislation includes all dogs regardless of their relationship to the owner. However, as noted in
5. Health and well-being of pet owners, it is likely exactly this relationship which mediates
effects of human-animal interaction on mental health and well-being.
Throughout this paper I wil use the terms ‘pet’ and ‘pet owner’ and specify where results
pertain to one species or another.
For further discussion of the definition of Assistance Animal in the Australian context, please
refer to RES 238 Accreditation of Assistance Animals.
Page 324 of 425
FOI 24/25- 0013
4. Pet ownership
The Australian Bureau of Statistics (ABS) collected pet ownership data in 1994. At this time,
59.2% of Australian households owned pets, with dogs comprising 37.5%. There is no
indication the ABS have tracked pet ownership since this 1994 survey (ABS, 1995).
The Household, Income and Labour Dynamics in Australia (HILDA) Survey, funded by the
Department of Social Services, is a yearly survey of 17,000 Australians that collects
information on “household and family relationships, child-care, employment, education,
income, expenditure, health and wellbeing, attitudes and values on a variety of subjects, and
various life events and experiences” (Wilkins et al, 2020, p.4). This survey collected data on
pet ownership for their 2018 survey, published in their 2020 report. However, they do not
appear to have collected pet ownership data for any other years. The HILDA survey shows for
2018, 62% of Australians had at least one pet. Of these pet owners, 72% (or 48% of the
population) reported having at least one dog (Wilkins et al, 2020).
The most current and comprehensive Australian pet ownership statistics are drawn from a
series of reports from the Animal Medicines Association (AMA). Every 3 years since 2013,
AMA has published pet ownership rates through the following reports:
• Pet ownership in Australia 2013
• Pet ownership in Australia 2016
• Pets in Australia: a national survey of pets and people (2019)
• Pets and the Pandemic: a social research snapshot of pets and people in the
COVID-19 era (2021 supplement).
Between 2013 and 2019, pet ownership was slowly declining. In 2013, 63% of households had
at least one pet (Animal Health Al iance, 2013). In 2016 this decreased to 62% (AMA, 2016)
and in 2019 to 61% (AMA, 2019). During the pandemic, this estimate increased considerably
to 69% in 2021 (AMA, 2021). USA experienced a similar jump in ownership during the
pandemic (Kretzler et al, 2022).
AMA’s 2021 supplement report estimated that almost half (47%) of all Australian households,
approximately 4.6 mil ion households, had at least one dog. This was an increase from the
2019 report where approximately 40% of households reported having at least one dog. This
represents the largest increase of any animal category between the 2019 and 2021 surveys.
Cat ownership also increased over this time – 27% of households in 2019 compared to 30% in
2021. Half of all dogs and cats acquired during the pandemic were acquired by existing pet
owners (AMA, 2021; refer to Table 1 – Pet ownership in Australia).
In giving reasons for acquiring a dog, 54% of households reported companionship and 23%
reported mental health reasons. When examining living arrangements, 37% of dog owners
living alone said they got their dog to improve their mental health compared to 22% for other
households (AMA, 2021). The 2019 report did not appear to ask survey participants if mental
Page 325 of 425
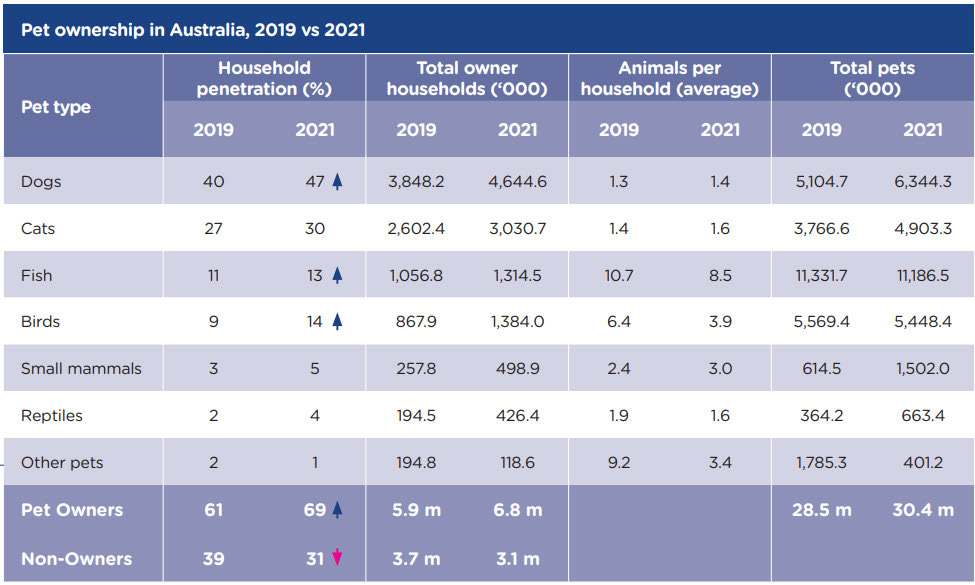
FOI 24/25- 0013
health was a contributing reason for acquiring their animal. However, the report does note that
18% of pet owners say that the animals has had a positive impact on their mental health
(AMA, 2019).
While the AMA reports are widely cited for their ownership estimates, there are some
methodological issues to consider. Firstly, although steps were taken to make the surveys
representative, small sample sizes mean some results may not be statistically reliable. The
overall increase in ownership percentage between 2019 and 2021 was statistically significant,
however data on reasons for acquiring a pet and perceived benefits of animal ownership do
not appear to have been tested for statistical significance.
Additionally, there is risk of bias considering the role of the AMA in preparing the report due to
their position as a peak body for animal health companies in Australia. The AMA funded the
research from social research companies Galaxy Research (for the 2013 report) and Newgate
Research (for the 2016, 2019 and 2021 reports). The role of AMA in preparing the publication
(for example, summarising data or drawing conclusions) is not clear from the report itself. This
lack of clarity about authorship is of concern as emphasising beneficial aspects of the human-
pet bond is a marketing tool used by the pet industry (Scoresby et al, 2021).
Table 1 – Pet ownership in Australia
Page 326 of 425
FOI 24/25- 0013
5. Health and well-being of pet owners
The literature connecting pet ownership with health and well-being is largely inconsistent. The
systematic reviews considered below support the assessment of many researchers that issues
with methodology and quality in the literature prevent reliable meta-analysis and therefore
prevent the building of a consistent evidence base for judging the effects of animal interaction
on human health (Rodriguez et al, 2021; Barroso et al, 2021; Clements et al, 2019). Almost all
reviews considered below mention the following problems:
• small sample sizes
• variability in study design including lack of controls or masking
• inconsistent use of standardised measures
• lack of standardised definitions.
There is also a need for researchers to control for confounding variables and to better describe
characteristics of the pet owner, the pet and the quality and duration of their relationship.
Several features can potentially mediate the benefits or harms of pet ownership, such as:
• gender, attachment style, ethnicity and cultural or religious dif erences of the owner
• temperament, training, breed of the pet
• living arrangements, family dynamics, type of dwelling
• activities that pet and owner usually do together
• duration of the relationship
• strength of attachment bond (Rodriguez et al, 2021; Scoresby et al, 2021; Brooks et
al, 2018; Carlisle et al, 2018;).
If awareness of these features is included in the study design it may allow researchers to
establish a more reliable association between pet ownership and health and well-being.
5.1 Perception of benefit
There is evidence of a public perception that pet ownership improves health and well-being
(Scoresby et al, 2021; Carlisle et al, 2020). Surveys indicate that improvements to health and
well-being can be a reason people acquire a pet (AMA 2021; AMA 2019).
5.2 Social interaction
Christian et al (2020) found more positive social interactions in young children with a pet at
home compared to those without. The correlation was strongest for single-child families.
A 2022 systematic review into the relationship between pet ownership, loneliness and social
isolation found most studies reported insignificant results relating to loneliness. Of the studies
that showed significant results, some reflected increased loneliness and others decreased
Page 327 of 425
FOI 24/25- 0013
loneliness. Only 2 of the 24 studies reviewed considered social isolation but both found pet
ownership correlates with lower social isolation. Some studies show a decrease in loneliness
with pet ownership, some show no significant relationship and some show an increase in
loneliness (Kretzler et al, 2022).
Wil iams et al (2021) investigated interventions that might reduce loneliness during the COVID-
19 pandemic. They reviewed 3 animal studies. One study involving a pet budgie showed no
significant results. The other two studies included both living and robotic dogs and showed a
positive reduction in loneliness. However, the study quality of both was poor/fair.
Clements et al (2019) found no evidence that keeping fish is associated with a reduction in
loneliness. One studied they reviewed showed very few participants acquire fish for the
purpose of companionship.
5.3 Mental health
Carlisle et al (2020) found parents of children with autism spectrum disorder (ASD) who owned
both a dog and a cat reported less stress and more benefit compared with parents who owned
only a dog or a cat. Christian et al (2020) found having a household pet was associated with
fewer social-emotional problems in young children. These findings contrast with the HILDA
survey. Wilkins et al (2020) compare their pet ownership data with participant’s answers to the
SF-36, a measure of general health and mental health, to determine if there is a correlation
between pet ownership and health or well-being. They found a slight reduction in mental health
scores for pet owners. In addition, people who own a cat are more likely to report lower life
satisfaction compared to dog owners. People who have both a dog and a cat are more likely to
report worse general and mental health compared to people with only a dog. Importantly, none
of these 3 studies found consistent evidence supporting a relationship between pet ownership
and positive wel -being.
Clements et al (2019) found inconsistent evidence for the relationship between interaction with
fish and psychological outcomes. Of the 24 studies reviewed, 4 found positive outcomes, 6
found partial support for positive outcomes and 5 found no support for positive outcomes.
Of the 54 articles reviewed in Scoresby et al (2021), 17 showed a positive impact of pet
ownership on mental health. However, 19 studies showed a mixed impact, 13 showed no
impact and 5 showed a negative impact. These inconsistent results are similar in other studies
(Rodriguez et al, 2021; Brooks et al, 2018). Little weight can be placed on the positive results
due to the quality and methodological issues identified in other studies. Some studies reviewed
in Scoresby et al (2021) showed that dog or cat ownership can reduce depression and anxiety
in children and adolescents. However, these studies did not control for confounding variables
such as family dynamics, which may contribute to children’s mental health. Also, the authors
note that the 54 studies reviewed used 75 different outcome measures, making comparison
between studies difficult.
Page 328 of 425
FOI 24/25- 0013
Overall, these studies show the relationship between pet ownership and mental health is
complex and requires more nuanced studies to demonstrate where the benefits of pet
ownership lie. Scoresby et al (2021, p.7) argue:
Developing clear guidelines about the benefits and liabilities of pet ownership and
mental health is important to mitigate the public halo effect that suggests that simply
acquiring a pet wil improve your mental health.
5.4 Physical health
Clements et al (2019) found some evidence that interaction with fish could reduce pain and
benefit nutritional intake and body mass. However, study designs were not sufficient to
attribute this effect to the animal interaction rather than to a confounding variable.
In their systematic review, Barroso et al (2021) found 6 out of 10 studies showed some
positive effect of pet ownership on cardiovascular disease. Of the remaining 4 studies, 2 found
mixed results, 1 found no effect and 1 found a negative effect. Of 4 studies that investigated
pet ownership and obesity, no effect was found. Considering the inconsistent results, quality
and design issues, no conclusions were possible regarding effects of pet ownership on
cardiovascular disease or obesity.
Page 329 of 425
FOI 24/25- 0013
6. References
Animal Health Al iance. (2013).
Pet ownership in Australia 2013.
https://animalmedicinesaustralia.org.au/wp-content/uploads/2019/10/AMA-Pet-
Ownership-in-Australia-5-AUGUST-2013.pdf
Animal Medicines Australia. (2016).
Pet ownership in Australia 2016.
https://animalmedicinesaustralia.org.au/report/pet-ownership-in-australia-2016/
Animal Medicines Australia. (2019).
Pets in Australia: a national survey of pets and people.
https://animalmedicinesaustralia.org.au/report/pets-in-australia-a-national-survey-of-
pets-and-people/
Animal Medicines Australia. (2021).
Pets and the Pandemic: a social research snapshot of
pets and people in the COVID-19 era.
https://animalmedicinesaustralia.org.au/report/pets-and-the-pandemic-a-social-
research-snapshot-of-pets-and-people-in-the-covid-19-era-2/
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental
disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Australian Bureau of Statistics. (1995). Australian Social Trends, 1995: Special Feature:
Household pets (No.4102.0).
https://www.abs.gov.au/AUSSTATS/abs@.nsf/2f762f95845417aeca25706c00834efa/5
ef8016f420622a3ca2570ec00753524!OpenDocument
Barroso, C. S., Brown, K. C., Laubach, D., Souza, M., Daugherty, L. M., & Dixson, M. (2021).
Cat and/or dog ownership, cardiovascular disease, and obesity: A systematic review.
Veterinary Sciences,
8(12), 333. https://doi.org/10.3390/vetsci8120333
Brooks, H. L., Rushton, K., Lovell, K., Bee, P., Walker, L., Grant, L., & Rogers, A. (2018). The
power of support from companion animals for people living with mental health problems:
a systematic review and narrative synthesis of the evidence.
BMC Psychiatry,
18(1).
https://doi.org/10.1186/s12888-018-1613-2
Carlisle, G. K., Johnson, R. A., Mazurek, M., Bibbo, J. L., Tocco, F., & Cameron, G. T. (2018).
Companion animals in families of children with autism spectrum disorder: Lessons
learned from caregivers.
Journal of Family Social Work,
21(4–5), 294–312.
https://doi.org/10.1080/10522158.2017.1394413
Carlisle, G. K., Johnson, R. A., Wang, Z., Brosi, T. C., Rife, E. M., & Hutchison, A. (2020).
Exploring human-companion animal interaction in families of children with autism.
Journal of Autism and Developmental Disorders,
50(8), 2793–2805.
https://doi.org/10.1007/s10803-020-04390-x
Christian, H., Mitrou, F., Cunneen, R., & Zubrick, S. R. (2020). Pets are associated with fewer
peer problems and emotional symptoms, and better prosocial behavior: Findings from
Page 330 of 425
FOI 24/25- 0013
the Longitudinal Study of Australian Children.
The Journal of Pediatrics,
220, 200-
206.e2. https://doi.org/10.1016/j.jpeds.2020.01.012
Clements, H., Valentin, S., Jenkins, N., Rankin, J., Baker, J. S., Gee, N., Snel grove, D., &
Sloman, K. (2019). The effects of interacting with fish in aquariums on human health
and well-being: A systematic review.
PloS One,
14(7), e0220524.
https://doi.org/10.1371/journal.pone.0220524
Companion Animals Act 1998 (NSW).
https://legislation.nsw.gov.au/view/whole/html/inforce/current/act-1998-087
Ferrell, J., & Crowley, S. L. (2021). Emotional support animals: A framework for clinical
decision-making.
Professional Psychology, Research and Practice,
52(6), 560–568.
https://doi.org/10.1037/pro0000391
Kretzler, B., König, H.-H., & Hajek, A. (2022). Pet ownership, loneliness, and social isolation: a
systematic review.
Social Psychiatry and Psychiatric Epidemiology,
57(10), 1935–1957.
https://doi.org/10.1007/s00127-022-02332-9
Miklósi, Á., Abdai, J., & Temesi, A. (2021). Searching where the treasure is: on the emergence
of human companion animal partnership (HCAP).
Animal Cognition,
24(2), 387–394.
https://doi.org/10.1007/s10071-020-01467-z
Rodriguez, K. E., Herzog, H., & Gee, N. R. (2020). Variability in human-Animal Interaction
research.
Frontiers in Veterinary Science,
7, 619600.
https://doi.org/10.3389/fvets.2020.619600
Royal Society for the Prevention of Cruelty to Animals. (2018).
RSPCA Policy A01
Responsible companion animal ownership. RSPCA Knowledge Base.
https://kb.rspca.org.au/knowledge-base/rspca-policy-a01-responsible-companion-
animal-ownership/
Scoresby, K. J., Strand, E. B., Ng, Z., Brown, K. C., Stilz, C. R., Strobel, K., Barroso, C. S., &
Souza, M. (2021). Pet ownership and quality of life: A systematic review of the
literature.
Veterinary Sciences,
8(12), 332. https://doi.org/10.3390/vetsci8120332
Sandoe, P., Corr, S., & Palmer, C. (2015).
Companion Animal Ethics. John Wiley & Sons
Wilkins, R., Botha, F., Vera-Toscano, E., Wooden, M. (2020).
The Household, Income and
Labour Dynamics in Australia Survey: Selected Findings from Waves 1 to 18.
Melbourne Institute: Applied Economic & Social Research, University of Melbourne.
https://melbourneinstitute.unimelb.edu.au/ data/assets/pdf file/0009/3537441/HILDA-
Statistical-report-2020.pdf
Wil iams, C. Y. K., Townson, A. T., Kapur, M., Ferreira, A. F., Nunn, R., Galante, J., Phil ips,
V., Gentry, S., & Usher-Smith, J. A. (2021). Interventions to reduce social isolation and
loneliness during COVID-19 physical distancing measures: A rapid systematic review.
PloS One,
16(2), e0247139. https://doi.org/10.1371/journal.pone.0247139
Page 331 of 425
FOI 24/25- 0013
DOCUMENT 31
Home Modifications and behaviours of concern
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Tactical Research Team (TRT) are
not to be shared external to the Branch. These are for internal TAB use only and are intended
to assist our advisors with their reasonable and necessary advice provision.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
TRT are unable to ensure that the information listed below provides an accurate & up-to-date
snapshot of these matters.
Research question: What is the research evidence to support the effectiveness of home
modifications for both adults and children with behaviours of concern?
Is there any research that relates to sensory processing/ leisure/interest activities to
decrease BoC / increase independence (e.g., bathtubs, playgrounds, secure backyards)?
Date: 10/03/2023
Requestor: Helen s22(1)(a)(ii) - irrelevant material
Endorsed by: Melinda s22(1)(a)(ii) - irrelevant ma
Researcher: Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Aaron s22(1)(a)(ii)
- irrelevant ma
Page 332 of 425
FOI 24/25- 0013
1. Contents
Home Modifications and behaviours of concern ........................................................................ 1
1.
Contents ....................................................................................................................... 2
2.
Summary ...................................................................................................................... 2
3.
Quality of research ........................................................................................................ 3
4.
Built environment and mental health ............................................................................. 3
5.
Built environment and behaviours of concern ............................................................... 4
5.1 Built environment and positive behaviour support ..................................................... 5
5.2 Autonomy and homeliness ........................................................................................ 7
5.3 Multi-sensory environments ....................................................................................... 8
6.
References ................................................................................................................... 9
2. Summary
Most reviews of the literature suggest some positive association between rates of behaviours
of concern and features of the built environment while acknowledging the low quality of the
evidence. There is low- to moderate- quality evidence of the association between fewer
behaviours and improved air quality, accessibility, access to nature, and homeliness of the
environment. Design features of a home may contribute to a reduction in stress and negative
emotions, and to a reduction in resulting behaviours. To the extent that a home modification
improves one of these design features, it is possible that a home modification may contribute
to a reduction in behaviours of concern. However, it is difficult to draw causal conclusions due
to the quality and study designs of the reviewed papers.
Guidelines regarding managing behaviours of concern generally recommend a personalised
approach. This should involve analysing an individual’s environment to isolate what factors are
contributing to behaviours of concern. This often depends on the resident’s preferences and
sensory needs. If certain features of the built environment are found to contribute to
behaviours of a particular person, removing or changing those features should be a part of the
relevant behaviour support plan. This is required by
National Disability Insurance Scheme
(Restrictive Practices and Behaviour Support) Rules 2018. In some cases, changing features
of a home which trigger behaviours of concern may involve home modifications.
Generalising about the effectiveness of particular modifications is not possible due to the
current quality of the evidence and to the essentially individual nature of causes of behaviours
of concern.
Page 333 of 425
FOI 24/25- 0013
3. Quality of research
Features of the physical environment can affect our health and functioning in daily activities.
Poor classroom acoustics can interrupt learning and academic performance (Murgia et al,
2023). Optimal temperature and ventilation can improve patient’s health outcomes in hospitals
(Shajaran et al, 2019). Researchers have tried to establish the link between built environment
and mood. For example, neighbourhoods which encourage walkability may lead to improved
health and mood of residents due to higher rates of physical activity (Han et al, 2022; Nuñez-
Gonzalez et al, 2020). There is some evidence that heat and humidity increase arousal, while
natural and green spaces decrease arousal (Baird et al, 2023).
It has been difficult to establish high quality evidence for direct association between specific
features of the built environment and incidence of behaviours of concern. Of particular note,
poor quality living environments are associated with low socio-economic conditions, which are
independently associated with poor mental health (Tibber et al, 2022). Background economic
conditions may often be the causal factor when studies do show a link between the built
environment and poor mental health outcomes or high rates of behaviours of concern.
The available evidence is often of low quality and there are several gaps in the literature. Nine
of the 11 systematic reviews reviewed by Nuñez-Gonzalez et al (2020) were found to be of
critically low quality. Bridge and Vasilacopolou (2019) noted expert opinion was the highest
frequency type of study appearing in the literature. Also, much of their evidence based is over
20 years old.
Baird et al (2023) note there is a particular lack of research on the impact of the physical
environment on children with developmental disabilities. This is echoed by Roos et al (2022)
who reviewed 276 studies but found little research on the effect of the built environment on
people with intellectual disabilities in long-term care. They identified 26 components of the built
environment that may affect health, behaviour and quality of life of people with intellectual
disability but found research on only seven components. Two studies from Bridge and
Vasilacopolou (2019) and Aljunaidy et al (2021) both note that there is an over-representation
of research focussed on people with dementia and Alzheimer’s disease compared to other
developmental or psychiatric diagnoses. Almost 60% of the studies reviewed by Bridge and
Vasilacopolou (2019) concerned dementia or Alzheimer’s disease. The next most prevalent
cohort in their study was intellectual disability at 18%.
4. Built environment and mental health
Qualitative studies show people associate features of the built environment with fluctuations in
their mental health, including location, personal space, homeliness and security (Tekin et al,
2023; Rollings & Bollo, 2021):
Behaviours of concern can be the result of interaction between a person and the
environment, wherein factors such as noise levels, stimulation or lack of stimulation,
Page 334 of 425
FOI 24/25- 0013
unmet needs, or unpredictable environments can increase the risk of, and can be the
motivation behind, such behaviours (Iffland et al, 2021, p.4).
There is a consensus that environmental features affect behaviours even if experimental and
quantitative evidence cannot establish a direct causal link between particular environmental
features and the rate of behaviours of concern in general.
Nuñez-Gonzalez et al (2020) found two high quality systematic reviews investigating the
effects of the built environment on mental health. Neither study found sufficient evidence to
draw conclusions on the association between the built environment and mental health and
neither discussed the presence of behaviours of concern (Moore et al, 2018; Turley et al,
2013). The only low risk of bias randomised controlled trial identified by Moore et al (2018)
showed no effect between the built environment changes and mental health.
Some large-scale primary studies have showed an association between indoor environment
and mental health. However, due to their study designs it is not possible to establish a causal
link between indoor environments and mental health. A 2020 cohort study of 2290 children
found poor indoor air quality caused by smoking leads to increased stress in younger
adolescents (Franklin et al, 2020). The higher stress levels may be partially reduced by
availability of green spaces. Exposure to second-hand smoke is also associated with more
stressful living conditions for children and so it is not clear whether poor indoor air quality is the
primary driver for increased stress levels. A survey of 8,177 people during COVID related
lockdowns found a strong association between self-reported symptoms of depression and
anxiety and lack of natural lighting, temperature control, air quality privacy, adequate space,
good views, access to nature, quality acoustics, and homeliness (Amerio et al, 2020). This
survey was based on self-reported measures and so it’s not clear whether poor environmental
features lead to poor mental health or whether people with poor mental health are more likely
to feel negatively towards their living environment.
5. Built environment and behaviours of concern
Murgia et al (2023) suggests that poor classroom acoustics can lead to increased negative
behaviours in children, including lack of attention and disruptive behaviour. However, the
evidence for this link is assumed rather than directly established.
In their rapid review, Oostermeijer et al (2021) found evidence that restrictive practices could
be reduced in psychiatric facilities with the introduction of access to private spaces, gardens,
pools, and other amenities. This is supported in a later study from Harpøth et al (2022). The
authors report reduction in restrictive practices after moving a psychiatric ward to a purpose-
built facility prioritising privacy, outdoor spaces, airflow and access to amenities and activities.
However, both studies note the difficulty of making causal inferences based on naturalistic
experiments.
Baird et al (2023) found evidence connecting interior design and architectural features to
aggressive behaviours and conduct problems in children. Low-moderate quality evidence
Page 335 of 425
FOI 24/25- 0013
showed higher rates of behaviours of concern in children are associated with red painted
rooms in the home, overcrowding and damp. In addition, they found inconsistent evidence that
environmental noise such as air and road traffic and construction noise contribute to an
increase in aggression. The authors hypothesis that noise may not cause aggressive
behaviours but may exacerbate behaviours in those more sensitive to noise. Five of the six
studies reviewed showed high or unclear risk of bias. The only study rated as low risk of bias
was also authored by Baird et al.
Baird et al (2023) found some low-quality evidence connecting design and architectural
features of playrooms with aggressive behaviours and conduct problems in children. An open
playroom reportedly reduced aggressive behaviours but there were inconsistent results
regarding the density of playrooms and no effect was observed for space per child or room
size.
There is some inconsistent evidence for the benefit of greenspace and access to nature for
young people, with the evidence broadly coalescing around positive effects on mood and
behaviour (Baird et al, 2023; Tekin et al, 2023; Han et al, 2022; McIntosh et al, 2022).
5.1 Built environment and positive behaviour support
Recent studies which address environmental antecedents of behaviours of concern from a
positive behaviour support perspective often focus on social and situational contexts (e.g.,
routine, activities, staff training, etc.) rather than physical features of the built environment
(Konstantinidou et al, 2023; Mahon et al, 2022; Deb et al, 2022; Beqiraj et al, 2022; Bruisma et
al, 2020). According to Caspar et al (2018), there is only minimal evidence that addressing
physical features of the environment alone is sufficient to reduce behaviours of concern. They
note that the evidence is more robust for interventions which treat physical and social
environments and other psychological factors. However, due to the combined nature of these
interventions it is often difficult to determine the causal factor.
Guidelines for developing individualised positive behaviour support plans suggest plans should
include an analysis of possible environmental triggers for behaviours of concern with the aim
of removing triggers to prevent behaviours. Significant environmental features related to the
built environment can include:
• location (room, own or other’s home, medical facility, school, new or unfamiliar
locations, recent changes to the house or care setting)
• dimensions of the room (crowded, cramped, open, empty etc.)
• furniture (size, texture, materials, colour, too much/too little)
• walls and surfaces (material, density, fragility, angle, texture, colour)
• air temperature and quality, airflow, smells
• nature, plants and outdoor spaces (accessible, open, healthy etc.)
• acoustics and noise (creaking doors, rapping pipes, flapping blinds)
Page 336 of 425
FOI 24/25- 0013
• light (brightness, colour, natural or artificial lighting)
• doors, windows, fences or other barriers (locks, latches, easily opened or closed)
• fixtures (access to taps, water temperature)
• homeliness or personalisation
• other features which may have specific associations for the person showing
behaviours of concern (Roos et al, 2022; Limbu et al, 2021; DHHS, 2020; DHHS,
2019; Bridge and Vasilacopolou, 2019; DHHS, 2018; NICE, 2015).
The Victorian State Government’s Department of Health and Human Services (now
Department of Families, Fairness and Housing) recommends behaviour support practitioners
consider the following questions about the physical environment:
• Does the physical environment allow the person to move around freely and gain
assistance from others when needed?
• Does the physical environment reflect the person’s likes and sensory preferences?
• Does the physical environment encourage independence and choice in daily
activities? (DHHS, 2019, p.6)
Positive behaviour support plans should also include recommendations for environmental
changes that may prevent behaviours of concern from developing. The
National Disability
Insurance Scheme (Restrictive Practices and Behaviour Support) Rules 2018 describe the
conditions under which a behaviour support plan containing restrictive practice must be
developed. Section 20.3(c) states that a specialised behaviour support practitioner must take
reasonable steps to, “make changes within the environment of the person with disability that
may reduce or remove the need for the use of regulated restrictive practices”.
In cases where restrictive practice is unavoidable, the practice can be made possible or
constituted by features of the home or physical environment. Time-outs, seclusion and secure
spaces for staff require adequate space, fixtures and security features to enact. Restrictive
practices can also include locks on doors or cupboards, surveil ance technology or other
structural features which prevent a person from accessing activities or areas in their home
(NDIS Quality and Safeguards Commission, 2022; NDIS Quality and Safeguards Commission,
2020; Bridge and Vasilacopolou, 2019).
Table 1 below shows some examples of housing design features which may help to prevent or
manage behaviours of concern. The list is adapted from Bridge and Vasilacopolou (2019).
These suggestions are derived from a smal sample of recommendations in the literature and
are not exhaustive.
Page 337 of 425
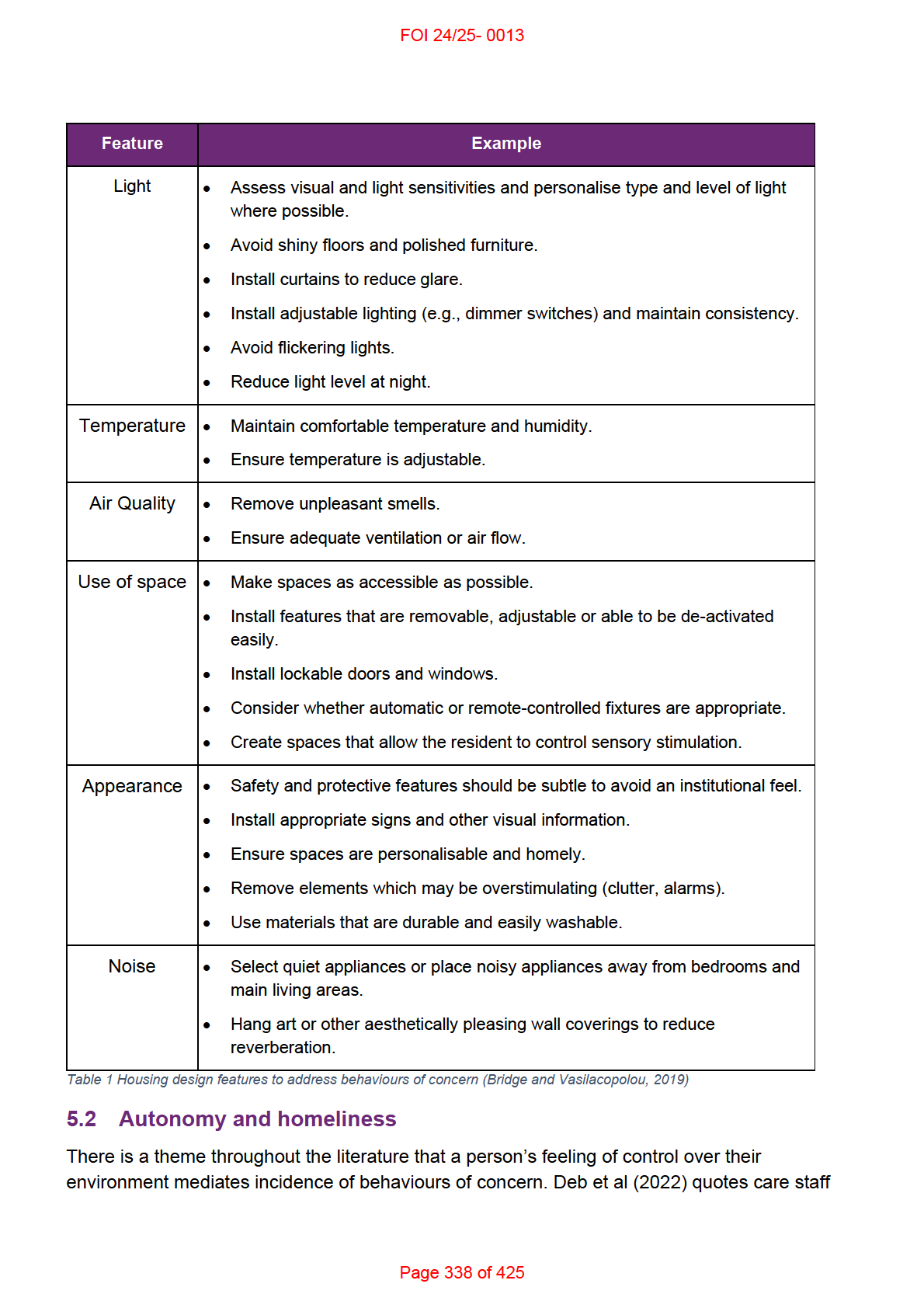
FOI 24/25- 0013
describing triggers in the physical environment such as the colour of a room or the position of
curtains. To address environmental triggers, many studies recommend strategies centred
around resident’s choice and control, such as access, privacy, predictability, personalisation,
adjustability, customisability and homeliness (Baird et al, 2023; Haig and Hallet, 2022;
Oostermeijer et al, 2021; Iffland et al, 2021; Bridge and Vasilacopolou, 2019).
Roos et al (2022) found evidence of association of behaviours of concern with the type of
residential facility, its size and homeliness, available views and sound quality/acoustics. The
authors suggest that most variables show effects based on their contribution to the homeliness
of the environment and access to appropriately stimulating activities and environments.
Homeliness has a positive association with behaviours including less lethargy, less
hyperactivity and less aggression, increased participation in social, domestic and individual
activities. Homeliness can be achieved in an institutional setting with:
smaller wards, rooms of different sizes with windows of different sizes and in different
places, public (common) spaces closer to the front door, unique bedrooms, wooden
doors, wallpaper, carpet, art, less reverberation, more light points in the living room, and
personal objects in the room (Roos et al, 2022, p.308).
These environments are likely to be more appropriately stimulating as well. In contrast, a place
is felt to be more institutional when it has:
more office, less public space, the same bedrooms, wide hallways, large rooms, high
ceilings, more passageways, rough (stone) walls, vinyl floors, little lighting, fixed ceiling
lights, more fire alarm systems, bare walls, different chairs, rows of toilets and sinks,
paper towel dispensers, grab bars, and more adaptations to disabilities … the roof is
less visible from the street, the driveway is longer, there are more windows in the
facade, and there is less greenery around the building (Roos et al, 2022, p.308).
However, as the authors did not perform a meta-analysis or investigate the quality, level of
evidence or risk of bias of the included studies, the evidence they present should be treated as
of very low quality.
5.3 Multi-sensory environments
Multi-sensory environments (MSEs; also called comfort rooms, sensory rooms or Snoezelen
rooms) are rooms designed to provide an ideal sensory environment with the aim of soothing
or stimulating a person with specific sensory needs (Unwin et al, 2022; Cameron et al, 2020).
MSEs have been used in nursing homes, schools, hospitals and psychiatric facilities. Little
research on MSEs have looked into their use in home environments (Unwin et al, 2022;
Backman et al, 2021; Cameron et al, 2020; Bridge and Vasilacopolou, 2019).
TRT’s RES 276 Sensory-based therapies provides more detail on MSEs and their effect on the
use of restrictive practice.
Evidence for the effectiveness of MSEs is generally of low quality due to study designs, risk of
bias, dif erences in how rooms are structured and used. Many studies also combine MSE use
Page 339 of 425
FOI 24/25- 0013
with other interventions such as staff training in behaviour support (Unwin et al, 2022; Haig
and Hallet, 2022; Oostermeijer et al, 2021).
In their 2022 review, Haig and Hallet did not find convincing evidence for a reduction in
aggressive behaviours of concern, though evidence does suggest that MSEs can provide
comfort to users in psychiatric facilities. The reviewed studies unanimously showed a reduction
in subjective measures of distress and a few studies also showed a reduction in arousal,
anxiety, irritability, hostility and withdrawal. Reduction in negative emotional states may lead to
a reduction in associated behaviours of concern, though the evidence for this connection is
less established (Oostermeijer et al, 2021; Cameron et al, 2020). Backman et al (2021)
reviewed three studies using MSEs in residential facilities for older people and found more
equivocal evidence for benefit to emotional wel -being and mental health.
There is some evidence that the way the room is used can mediate its effectiveness. Haig and
Halett (2022) note that distress increased for a smal number of patients, which may relate to
the different ways in which MSEs are set up and used and dif erent sensory needs of
individuals. Unwin et al (2022) found that children with autism who were able to control
features of the room’s equipment (active condition) showed increase in attention and reduction
in repetitive motor and sensory behaviours. It is important to note that these behaviours are
not necessarily concerning and a decrease in sensory and repetitive behaviours may not have
any relation to the person’s health or well-being. The authors also found no significant
difference in social behaviours, anxiety, positive affect or arousal between the active and
passive conditions.
6. References
Aljunaidy, M. M., & Adi, M. N. (2021). Architecture and Mental Disorders: A Systematic Study
of Peer-Reviewed Literature.
HERD,
14(3), 320–330.
https://doi.org/10.1177/1937586720973767
Amerio, A., Brambil a, A., Morganti, A., Aguglia, A., Bianchi, D., Santi, F., Costantini, L.,
Odone, A., Costanza, A., Signorelli, C., Serafini, G., Amore, M., & Capolongo, S.
(2020). COVID-19 Lockdown: Housing Built Environment's Effects on Mental Health.
International journal of environmental research and public health,
17(16), 5973.
https://doi.org/10.3390/ijerph17165973
Backman, C., Demery-Varin, M., Cho-Young, D., Crick, M., & Squires, J. (2021). Impact of
sensory interventions on the quality of life of long-term care residents: a scoping review.
BMJ open,
11(3), e042466. https://doi.org/10.1136/bmjopen-2020-042466
Baird, A., Candy, B., Flouri, E., Tyler, N., & Hassiotis, A. (2023). The Association between
Physical Environment and Externalising Problems in Typically Developing and
Neurodiverse Children and Young People: A Narrative Review.
International journal of
environmental research and public health,
20(3), 2549.
https://doi.org/10.3390/ijerph20032549
Page 340 of 425
FOI 24/25- 0013
Beqiraj, L., Denne, L. D., Hastings, R. P., & Paris, A. (2022). Positive behavioural support for
children and young people with developmental disabilities in special education settings:
A systematic review.
Journal of applied research in intellectual disabilities: JARID,
35(3), 719–735. https:/ doi.org/10.1111/jar.12989
Bridge, C. & Vasilakopoulou, K. (2019). Designing home environments for people with
problems with cognition who display aggressive or self-injurious behaviour, Ed. 2.
Home
Modification Information Clearinghouse. https://doi.org/10.26288/5DDDEAFDC0906
Bruinsma, E., van den Hoofdakker, B. J., Groenman, A. P., Hoekstra, P. J., de Kuijper, G. M.,
Klaver, M., & de Bildt, A. A. (2020). Non-pharmacological interventions for challenging
behaviours of adults with intellectual disabilities: A meta-analysis.
Journal of intellectual
disability research: JIDR,
64(8), 561–578. https://doi.org/10.1111/jir.12736
Cameron, A., Burns, P., Garner, A., Lau, S., Dixon, R., Pascoe, C., & Szafraniec, M. (2020).
Making sense of multi-sensory environments: A scoping review.
International Journal of
Disability, Development, and Education,
67(6), 630–656.
https://doi.org/10.1080/1034912x.2019.1634247
Carnemolla, P., & Bridge, C. (2019). Housing Design and Community Care: How Home
Modifications Reduce Care Needs of Older People and People with Disability.
International Journal of Environmental Research and Public Health,
16(11), 1951. MDPI
AG. http://dx.doi.org/10.3390/ijerph16111951
Caspar, S., Davis, E. D., Douziech, A., & Scott, D. R. (2018). Nonpharmacological
Management of Behavioral and Psychological Symptoms of Dementia: What Works, in
What Circumstances, and Why?.
Innovation in aging,
2(1), igy001.
https://doi.org/10.1093/geroni/igy001
Deb, S. S., Limbu, B., Unwin, G. L., & Weaver, T. (2022). Causes of and Alternatives to
Medication for Behaviours That Challenge in People with Intellectual Disabilities: Direct
Care Providers' Perspectives.
International journal of environmental research and public
health,
19(16), 9988. https://doi.org/10.3390/ijerph19169988
Department of Health and Human Services. (2018).
Positive practice framework: a guide for
behaviour support practitioners. https://www.dffh.vic.gov.au/positive-practice-
framework-word
Department of Health and Human Services. (2019).
Recognising and reducing mechanical
restraint: practice guide. https:/ www.dffh.vic.gov.au/recognising-and-reducing-
mechanical-restraint-practice-guide-word
Department of Health and Human Services. (2020).
Senior Practitioner report 2018–19.
https://www.dffh.vic.gov.au/sites/default/files/documents/202110/Senior%20Practitioner
%20Report%202018-2019.pdf
Page 341 of 425
FOI 24/25- 0013
Franklin, M., Yin, X., McConnell, R., & Fruin, S. (2020). Association of the Built Environment
With Childhood Psychosocial Stress.
JAMA network open,
3(10), e2017634.
https://doi.org/10.1001/jamanetworkopen.2020.17634
Haig, S., & Hallett, N. (2022). Use of sensory rooms in adult psychiatric inpatient settings: A
systematic review and narrative synthesis.
International Journal of Mental Health
Nursing. https:/ doi.org/10.1111/inm.13065
Iffland M, Xu J, Gil ies D. Organisational interventions for decreasing the use of restrictive
practices with children or adults who have an intellectual or developmental disability.
Cochrane Database of Systematic Reviews 2021, Issue 1. Art. No.: CD013840. DOI:
10.1002/14651858.CD013840.
Konstantinidou, I., Dil enburger, K., & Ramey, D. (2023). Positive behaviour support: a
systematic literature review of the effect of staff training and organisational behaviour
management.
International journal of developmental disabilities,
69(1), 29–44.
https://doi.org/10.1080/20473869.2022.2123199
Limbu, B., Unwin, G., & Deb, S. S. (2021). Comprehensive Assessment of Triggers for
Behaviours of Concern Scale (CATS): Initial Development.
International journal of
environmental research and public health,
18(20), 10674.
https://doi.org/10.3390/ijerph182010674
Mahon, D., Walsh, E., Holloway, J., & Lydon, H. (2022). A systematic review of training
methods to increase staff's knowledge and implementation of positive behaviour
support in residential and day settings for individuals with intellectual and
developmental disabilities.
Journal of intellectual disabilities: JOID,
26(3), 732–757.
https://doi.org/10.1177/17446295211022124
McIntosh, J., Marques, B., & Jenkin, G. (2022). The Role of Courtyards within Acute Mental
Health Wards: Designing with Recovery in Mind.
International journal of environmental
research and public health,
19(18), 11414. https://doi.org/10.3390/ijerph191811414
Moore, T. H. M., Kesten, J. M., López-López, J. A., Ijaz, S., McAleenan, A., Richards, A., Gray,
S., Savović, J., & Audrey, S. (2018). The effects of changes to the built environment on
the mental health and well-being of adults: Systematic review.
Health & Place,
53, 237–
257. https://doi.org/10.1016/j.healthplace.2018.07.012
Murgia, S., Webster, J., Cutiva, L. C. C., & Bottalico, P. (2023). Systematic Review of
Literature on Speech Intelligibility and Classroom Acoustics in Elementary Schools.
Language, speech, and hearing services in schools,
54(1), 322–335.
https://doi.org/10.1044/2022_LSHSS-21-00181
National Disability Insurance Scheme (Restrictive Practices and Behaviour Support) Rules
2018 (Cth). https://www.legislation.gov.au/Details/F2020C01087
National Institute for Health and Care Excellence. (2015).
Challenging behaviour and learning
disabilities (NICE guideline NG11). https:/ www.nice.org.uk/guidance/ng11
Page 342 of 425
FOI 24/25- 0013
NDIS Quality and Safeguards Commission. (2020).
Regulated Restrictive Practices Guide.
Penrith, Australia: NDIS Quality and Safeguards Commission.
https://www.ndiscommission.gov.au/sites/default/files/2022-02/regulated-restrictive-
practice-guide-rrp-20200 0.pdf
NDIS Quality and Safeguards Commission. (2022).
Surveil ance Technology Practice Guide.
Penrith, Australia: NDIS Quality and Safeguards Commission.
https://www.ndiscommission.gov.au/sites/default/files/2022-
08/SurveiIlance%20Technology%20Guide%20August%202022.pdf
Núñez-González, S., Delgado-Ron, J. A., Gault, C., Lara-Vinueza, A., Calle-Celi, D., Porreca,
R., & Simancas-Racines, D. (2020). Overview of Systematic Reviews of the Built
Environment's Effects on Mental Health.
Journal of environmental and public health,
2020, 9523127. https://doi.org/10.1155/2020/9523127
Oostermeijer, S., Brasier, C., Harvey, C., Hamilton, B., Roper, C., Martel, A., Fletcher, J., &
Brophy, L. (2021). Design features that reduce the use of seclusion and restraint in
mental health facilities: a rapid systematic review.
BMJ Open,
11(7), e046647.
https://doi.org/10.1136/bmjopen-2020-046647
Roos, J., Koppen, G., Vollmer, T. C., Van Schijndel-Speet, M., & Dijkxhoorn, Y. (2022).
Unlimited surrounding: A scoping review on the impact of the built environment on
health, behavior, and quality of life of individuals with intellectual disabilities in long-term
care.
HERD,
15(3), 295–314. https://doi.org/10.1177/19375867221085040
Rollings, K. A., & Bollo, C. S. (2021). Permanent supportive housing design characteristics
associated with the mental health of formerly homeless adults in the U.S. and Canada:
An integrative review.
International Journal of Environmental Research and Public
Health,
18(18), 9588. https://doi.org/10.3390/ijerph18189588
Shajahan, A., Culp, C. H., & Wil iamson, B. (2019). Effects of indoor environmental parameters
related to building heating, ventilation, and air conditioning systems on patients' medical
outcomes: A review of scientific research on hospital buildings.
Indoor air,
29(2), 161–
176. https://doi.org/10.1111/ina.12531
Tekin, B. H., Corcoran, R., & Gutiérrez, R. U. (2023). A Systematic Review and Conceptual
Framework of Biophilic Design Parameters in Clinical Environments.
HERD,
16(1),
233–250. https://doi.org/10.1177/19375867221118675
Tibber, M. S., Walji, F., Kirkbride, J. B., & Huddy, V. (2022). The association between income
inequality and adult mental health at the subnational level-a systematic review. Social
psychiatry and psychiatric epidemiology, 57(1), 1–24. https://doi.org/10.1007/s00127-
021-02159-w
Turley R, Saith R, Bhan N, Rehfuess E, Carter B. (2013). Slum upgrading strategies involving
physical environment and infrastructure interventions and their effects on health and
Page 343 of 425
FOI 24/25- 0013
socio‐economic outcomes.
Cochrane Database of Systematic Reviews, (1), Art. No.:
CD010067. DOI: 10.1002/14651858.CD010067.pub2
Unwin, K. L., Powell, G., & Jones, C. R. (2022). The use of Multi-Sensory Environments with
autistic children: Exploring the effect of having control of sensory changes.
Autism: The
International Journal of Research and Practice,
26(6), 1379–1394.
https://doi.org/10.1177/13623613211050176
Page 344 of 425