FOI 24/25- 0013
DOCUMENT 32
Summary of evidence quality of 6 cooking skills
related articles
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: Please evaluate the study quality of the following references provided
to TAB as support for a Thermomix for an individual with autism:
Nicollet, C., Zale, R., & Urbanowicz, A. (2016). Spectrum cooking. Evaluation of cooking classes
for young adults on the autism spectrum – executive summary.
Gustin, L., Funk, H. E., Reibolt, W., Parker, Em., Smith, N., & Blaine, R. (2020). Gaining
independence: cooking classes tailored for college students with autism (practice brief).
Journal of Postsecondary Education and Disability, 33(4), 395-403.
Bal, V. H., Kim, S-H., Cheong, D., Lord, C. (2015). Daily living skills in individuals with autism
spectrum disorder from 2 to 21 years of age. Autism, 19(7), 774-784.
Goldschmidt, J., & Song, H-J. (2017). Development of cooking skills as nutrition intervention
for adults with autism and other developmental disabilities. Journal of the Academy of
Nutrition and Dietetics, 117(5), 671-679.
Smith, K. A., Ayres, K. A., Alexander, J., Ledford, J. R., Shepley, C., & Shepley, S. B. (2016).
Initiation and generalisation of self-instructional skills in adolescents with autism and
intellectual disability. Journal of Autism and Developmental Disorders, 46, 1196-1209.
Ayres, K., & Cihak, D. (2010). Computer- and Video-based instruction of food-preparation
skills: acquisition, generalisation, and maintenance. Intellectual and Developmental
Disabilities, 48(3), 195-208.
Date: 23/2/2023
Requestor: Shannon s22(1)(a)(ii)
- irr
Endorsed by:
Page 345 of 425
FOI 24/25- 0013
Researcher: Stephanie s22(1)(a)(ii)
- irrelevant mate and Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Stephanie s22(1)(a)(ii) - irrelevant mat
1. Contents
Summary of evidence quality of 6 cooking skil s related articles ................................................ 1
1.
Contents ....................................................................................................................... 2
2.
Summary ...................................................................................................................... 2
3.
Articles .......................................................................................................................... 2
2. Summary
Six articles are examined below. Five of the articles describe an intervention aiming to improve
cooking skil s of people with developmental disabilities. The other article is an observational
study examining predictors of daily living skills in people with autism. Five of the included
studies describe people with autism and three describe people with intellectual or other
developmental disabilities.
These studies provide low quality evidence that people with autism or intellectual disability can
be assisted to develop cooking skil s. The main limitations of the studies are high risk of bias,
low sample sizes, uncontrolled study designs and unsystematised review methods. No
randomised controlled trials or systematic reviews were included, which are considered the
highest quality of evidence due to a lower risk of bias.
None of the included studies discuss the Thermomix or any other thermal cookers available on
the market. In fact, while acknowledging the limitations of the articles included, they all support
the possibility of assisting people with autism or intellectual disability to learn traditional
cooking skil s.
3. Articles
Nicollet, C., Zale, R., & Urbanowicz, A. (2016). Spectrum cooking. Evaluation of cooking
classes for young adults on the autism spectrum – executive summary.
This study does not mention the Thermomix or any other thermal cookers available on the
market.
This reference is an executive summary of the research, even so the evidence quality is low:
only 4 individuals provided data about the cooking program and data was collected 12 months
after the program ceased which may introduce biased/distorted recol ections. There was no
control group as it related to feedback/lived-experience of a specific cooking class program.
Page 346 of 425
FOI 24/25- 0013
The research evaluated cooking classes for individuals with autism. The purpose of the
program was to practice cooking related skil s. Participants were assisted to practice skills
such as following recipes and kneading dough. The classes also provided an opportunity for
participants to try new foods, socialise and cooperate. There were four study participants
between the ages 18-22 years old (however the cooking classes involved 6 individuals).
Evaluation of the cooking classes was qualitative via structured interview with key questions.
This data was collected 12 months after the cooking class program finished. The research did
not discuss appliances used in the cooking program and whether study participants found
cooking appliances beneficial.
One of the feedback comments regarding the cooking program related to sensory
considerations, “…be mindful of the person’s needs, when it comes to Asperger’s they may not
like loud noises around you know, banging pots and everything, the smells might be too much
or something like that.”
Note: The following passage is taken from the Thermomix website acknowledging the volume:
How loud is the Thermomix ®? – Vorwerk International Help Center (2018)
The Thermomix ® works very quietly in almost all situations. As with all motorized
kitchen appliances, the Thermomix® may get noisier for a short time when starting to
chop hard foods such as grains, ice, or frozen fruits. The device produces a similar level
of noise to a grain mil , but it reduces after just a few seconds.
If the Thermomix is to loud. As using the Thermomix® to chop big pieces of vegetables, the device may start to
vibrate and produce a loud noise. If that happens, consider
cutting the vegetables
into smaller pieces that may fit between the cutting knife of the device.
Assure that
the device lays stable on an even surface and that
there is nothing under the
device like a power cord.
Considering the finishing sound of the device that informs you that the step is finished,
you may set up the volume of that sound in the device settings.
Gustin, L., Funk, H. E., Reibolt, W., Parker, Em., Smith, N., & Blaine, R. (2020). Gaining
independence: cooking classes tailored for col ege students with autism (practice
brief). Journal of Postsecondary Education and Disability, 33(4), 395-403.
This study does not mention the Thermomix or any other thermal cookers available on the
market.
Evidence quality is low: it is a pre-test post-test design without a control group, the participant
number is small, the outcome measures were based on a questionnaire completed by the
participants which is vulnerable to bias.
The article reviews the effectiveness of a six week cooking course designed to teach cooking
skil s to college students with autism. The cooking program was part of a broader ‘Learning
Independence for Empowerment (LIFE) Project’ for students with disabilities. The paper states
that recipes in the cooking class were intended to teach basic skil s without becoming
Page 347 of 425
FOI 24/25- 0013
overwhelming for the students, such as knife skil s, baking, cooking on a stove top and using a
blender.
The literature review conducted by the authors acknowledged the link between autism traits
and feeding behaviour that may impact health and daily living skil s. Out of 16 cooking class
participants, full data-sets (pre- and post-tests) were collected from 11; study participants were
aged between 19-26 years old. The outcomes for the research were to determine if the
cooking classes increased cooking confidence, increased frequency of cooking at home, and
increased wil ingness to try new foods. It was found the students increased their home cooking
by an average of one meal per week, confidence in cooking increased, and acceptance of new
foods increased. The research does not describe how much of each specific cooking skil was
practiced and if one cooking method was preferred by participants over another. The research
mentions appliances such as stove and blender bit does not describe whether or how often
participants used appliances.
Bal, V. H., Kim, S-H., Cheong, D., Lord, C. (2015). Daily living skills in individuals with
autism spectrum disorder from 2 to 21 years of age. Autism, 19(7), 774-784.
This study does not mention the Thermomix or any other thermal cookers available on the
market.
Evidence quality is low-to-moderate due to the study design and potential lack of
generalisability. This study is a longitudinal observational study with no control group. While
the study starts with a good sized sample, attrition over time reduced the representativeness of
the group and therefore limits generalisability.
The study purpose was to investigate predictors of attainment of daily living skil s for
individuals with autism. Daily living skills were measured by the Vinelands scale for adaptive
functioning and was recorded at regular intervals (2, 3, 5, 9, 10, 13, 18 and 21 years old). This
data was used to predict the trajectory of daily living skil s for individuals with autism. Food
preparation skil s were assessed as part of the Vineland interview, though this aspect of daily
living skills received only minimal focus as part of the study.
Goldschmidt, J., & Song, H-J. (2017). Development of cooking skil s as nutrition
intervention for adults with autism and other developmental disabilities. Journal of the
Academy of Nutrition and Dietetics, 117(5), 671-679.
This study does not mention the Thermomix or any other thermal cookers available on the
market.
Evidence quality is low due to study design and risk of bias. This study is a narrative literature
review and opinion piece.
The authors argue that cooking skil s can change a person’s relationship with food as well as
contribute to improved nutritional status. The article is a promotion of a program called Active
Engagement, which is aims to increase generalised cooking skil s and independence in the
kitchen for adults with autism. In the first stage of the program, participants were required to
Page 348 of 425
FOI 24/25- 0013
prepare salads by learning learn how to chop, cut, grate and peel. Once participants
demonstrated these skil s, they could progress to the next stage of using small, low risk, low
appliances and eventually larger appliances. This article only focuses on the first salad-making
stage of the program and does not detail study participants’ experience with using cooking
appliances.
Smith, K. A., Ayres, K. A., Alexander, J., Ledford, J. R., Shepley, C., & Shepley, S. B.
(2016). Initiation and generalisation of self-instructional skil s in adolescents with
autism and intel ectual disability. Journal of Autism and Developmental Disorders, 46,
1196-1209.
This study does not mention the Thermomix or any other thermal cookers available on the
market.
Evidence quality is low due to study design. This is a pre-test/post-test study with no control
group and a small sample size of just 4 participants.
The study investigated whether video material can facilitate self-instructional learning for
adolescents with autism and intellectual disability. The content of the videos included kitchen,
office and other household skil s. Kitchen processes included putting popcorn in the
microwave, brushing zucchini with olive oil, and making lemonade.
Note: Although this research did not reference Thermomix or thermal cookers,
some
Thermomix (TM6) guided-cooking recipes now have video instructions which it could be
argued is a similar scenario to this research of teaching an individual to self-instruct.
Ayres, K., & Cihak, D. (2010). Computer- and Video-based instruction of food-
preparation skil s: acquisition, generalisation, and maintenance. Intel ectual and
Developmental Disabilities, 48(3), 195-208.
This study does not mention the Thermomix or any other thermal cookers available on the
market.
Evidence quality is low due to study design and age of paper. This is a pre-test/post-test study
with no control group and a small sample size of just 3 participants. The paper was published
13 years ago, which may affect the relevance of the technology-based interventions described.
This study evaluated the effect of computer-based video instruction on learning life skil s, such
as making a sandwich, microwaving soup or setting a table. Computer-based video instruction
was found to facilitate skil acquisition in the immediate term, however skil s were shown to
have declined at the 6- and 12-week assessments. On repeating the training, the skil was
reacquired.
Note: Although this research did not reference Thermomix or thermal cookers,
some
Thermomix (TM6) guided-cooking recipes now have video instructions which it could be
argued is a similar scenario to this research of teaching an individual to self-instruct.
Page 349 of 425
FOI 24/25- 0013
DOCUMENT 34
Transcranial magnetic stimulation for the
treatment of psychosocial conditions
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice. The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: What is the efficacy of Transcranial Magnetic Stimulation for adults
with Obsessive Compulsive Disorder, Bipolar Disorder and/or Depression? Is there evidence
of impact on functional outcomes such as social and economic participation?
Date: 23/06/2023
Requestor: Jil ian s22(1)(a)(ii)
- irrelevant mater
Endorsed by: Katrin s22(1)(a)(ii)
- irreleva
Researcher: Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Stephanie s22(1)(a)(ii) - irrelevant mat
1. Contents
Transcranial magnetic stimulation for the treatment of psychosocial conditions ........................ 1
1.
Contents ....................................................................................................................... 1
2.
Summary ...................................................................................................................... 2
3.
Transcranial Magnetic Stimulation ................................................................................ 2
4.
Guidelines ..................................................................................................................... 3
5.
Major Depressive Disorder ........................................................................................... 4
6.
Bipolar disorder ............................................................................................................. 5
7.
Obsessive-Compulsive Disorder ................................................................................... 5
8.
References ................................................................................................................... 6
Page 370 of 425
FOI 24/25- 0013
2. Summary
Transcranial Magnetic Stimulation (TMS) is a type of non-invasive brain stimulation. There is a
substantial body of literature relating to use of repetitive TMS (rTMS) to treat many psychiatric
and neurological disorders. This paper focusses on Major Depressive Disorder (MDD), bipolar
disorder and Obsessive-Compulsive Disorder (OCD).
Most clinical practice guidelines and systematic reviews agree that rTMS is an effective
treatment for symptoms of depression, especially treatment resistant Major Depressive
Disoder (MDD). There is stil some debate regarding treatment protocols and ef ect sizes.
While there is evidence that rTMS can be effective for bipolar disorder and OCD, it is more
tentative than in the case of MDD. The treatment may be offered in these cases where other
treatments have not been successful. There is wide agreement in the research that
heterogeneity of treatment protocols and small sample sizes in primary studies make it difficult
to draw more definite conclusions.
Evidence of improvements in functional outcomes for MDD, bipolar and OCD is minimal. Some
evidence exists around cognitive function. There is some evidence that rTMS can improve
cognitive function in healthy people as well as people with psychosocial conditions. However,
more evidence is required to establish this. No experimental evidence relating to efficacy of
rTMS to improve social or economic participation was found.
3. Transcranial Magnetic Stimulation
TMS is a type of non-invasive brain stimulation, which is a variety of neuromodulation or
neurostimulation. rTMS is generally safe and well-tolerated by patients and patients are
conscious during treatment. TMS involves the application of a wire coil to the patient’s head
which sends a pulsed magnetic field through the skull into the brain to alter brain function
(RANZCP, 2018a; RANZCP, 2018b; Hyde et al, 2022; Moses et al, 2023).
Single-pulse or paired-pulse TMS involves delivering one or two pulses to the patient’s brain
and is used primarily for exploratory or diagnostic purposes. Repetitive TMS is used for
therapeutic purposes and involves delivering recurring pulses to a specific brain region to
induce changes in brain activity. (Mann & Malhi, 2023; Klomjai et al, 2015).
Most research has focussed on rTMS for the treatment of depression but there is a substantial
literature base describing its use for other psychiatric disorders, neurological and
neurodevelopmental disorders, movement disorders, epilepsy, chronic pain and tinnitus (Tikka
et al, 2023; Mann & Malhi, 2023; Moses et al, 2023; Hyde et al, 2022; Lefaucher et al, 2020).
Protocols for rTMS can vary by:
• length or number of sessions frequency during a treatment block
• frequency, intensity, duration, or pattern of stimulus
• brain region targeted
Page 371 of 425
FOI 24/25- 0013
• coil-type or other device parameters
• additional or simultaneous treatments (Gutierrez et al, 2022; Klomjai et al, 2015).
Recognised varieties of rTMS include:
• theta-burst stimulation (TBS) –uses multiple bursts of high frequency stimulation
over a shorter session (Voigt et al, 2021)
• accelerated TMS (aTMS) – treatment sessions are scheduled multiple times per day
over a shorter overall treatment period (Somnez et al, 2019)
• deep TMS (dTMS) –uses a specialised coil to deliver pulses to deeper brain regions
(Gutierrez et al, 2022)
• priming TMS (pTMS) – a sub-threshold stimulus is delivered with the intention of
making the brain region more receptive to subsequent treatment (Lee et al, 2021).
4. Guidelines
Professional Practice Guidelines from the Royal Australian and New Zealand College of
Psychiatrists (RANZCP) supports the use of rTMS for depression, especially treatment
resistant depression and as a treatment of auditory hallucinations in schizophrenia (RANZCP,
2018a; RANZCP, 2018b).
Further evidence has emerged since the publication of the RANZCP guidelines. 2020 clinical
guidelines from a European team of clinicians notes definite efficacy of rTMS for depression
and probable efficacy for its use in treating PTSD, auditory hallucinations and negative
symptoms of schizophrenia. These guidelines note only possible efficacy for treatment of OCD
(Lefaucher et al, 2020).
A clinical practice guideline jointly published by the U.S. Department of Veterans Affairs and
U.S. Department of Defense recommends TMS for treatment resistant MDD, but notes only
weak evidence in its favour (McQuaid et al, 2022).
Recent clinical guidelines from the Indian Psychiatric Society offer a strong recommendation
for the use of high frequency rTMS to treat acute episodes of depression. They offer moderate
or low strength recommendations for the use of rTMS to treat bipolar disorder, generalised
anxiety disorder, OCD, post-traumatic stress disorder, negative symptoms of schizophrenia,
nicotine use disorder, Alzheimer’s disease, insomnia, migraine, fibromyalgia and tinnitus
(Tikka et al, 2023).
Page 372 of 425
FOI 24/25- 0013
5. Major Depressive Disorder
Clinical practice guidelines and systematic reviews generally support TMS as a safe and
effective treatment for MDD. Evidence is strongest for the efficacy of high frequency rTMS on
acute depressive episodes (Tikka et al, 2023; Hyde et al, 2022; Lefaucher et al, 2020) and
treatment resistant depression (McQuaid et al, 2022; RANZCP, 2018b).
Brini et al (2022) reviewed 29 systematic reviews including 15 meta-analyses of TMS efficacy
for patients with MDD. They found authors of all studies agreed that TMS is effective for
reducing depressive symptoms of MDD. However, the authors conclude that TMS may be less
efficacious and less well tolerated than current literature suggests. After reviewing meta-
analyses, Brini et al found that the effect sizes were generally smaller than reported. They also
report that systematic reviews included in the study are mostly of very low quality and show
high risk of bias. Primary studies included in the reviews also show a high level of
heterogeneity in treatment protocols.
There is evidence of improved cognitive function after TMS in people with MDD, including
executive function, set-shifting ability, visual scanning, and psychomotor speed (Xu et al 2023;
Torres et al, 2023; Tateishi et al, 2022; Struckman et al, 2021; Schaffer et al, 2020; Martin et
al, 2017). Begeman et al (2020) found only small improvements in working memory and
attention. Tikka et al (2023) note that if a patient’s depressive symptoms respond to TMS, it is
more likely they wil see improvements in executive function as well.
Very few studies report on other functional outcomes of TMS treatments. A Canadian health
technology assessment offers some qualitative evidence that rTMS treatment improves
patient’s quality of life:
When it came to the nature of the improvement, participants often described the lifting of
a weight off their shoulders and the disappearance of negative thoughts. Often activities
of daily living were easier to do and could be done with greater energy. Some
participants mentioned a change in sleep pattern or greater appetite (Ontario Health,
2021, p.119)
The same report conducted a systematic review of 68 studies and found only one that reported
functional outcomes (Taylor et al, 2018). Another government funded Canadian review
identified Taylor et al (2018) as the only study reporting functional outcomes (Pohar & Farah,
2019). This RCT assessed efficacy of rTMS on 32 people with MMD. The Work and Social
Adjustment Scale (WSAS) and the Global Assessment of Function (GAF) were used as
secondary outcome measures. The study found no significant effect on either WSAS or GAF
scores after rTMS treatment (Taylor et al, 2018).
One large observational study of 257 people with treatment resistant MDD found a significant
improvement in function following rTMS treatment using the Clinical Global Impressions survey
(CGI-S). The effect was maintained at 3, 6, 9 and 12 month follow ups (Denner et al, 2014).
Page 373 of 425
FOI 24/25- 0013
6. Bipolar disorder
Mutz (2023) and Tikka et al (2023) note evidence that TMS is effective in treating bipolar
disorder using high frequency stimulation of the dorsolateral prefrontal cortex. However,
numerous other studies find no significant effect compared to sham controls. Researchers
conclude that further research is needed to determine if TMS is effective in treating bipolar
(Mutz, 2023; Hyde et al, 2022; Elsayed et al, 2022; Hett & Marhawa, 2020; Gold et al, 2019).
Mutz et al (2023) report evidence from 2 studies indicating improvement in cognitive function
after TMS. An RCT assessing 52 people with bipolar disorder found improve across all
cognitive measures compared to sham control. A pilot study assessing 16 people with bipolar
disorder found improvements in verbal learning but no other cognitive functions. However,
more studies reviewed found no significant effect (Mutz et al, 2023; Hett & Marhawa, 2020).
No other information on functional outcomes was found.
7. Obsessive-Compulsive Disorder
Recent systematic reviews note general positive results from studies investigating effects of
TMS on symptoms of OCD, especially low frequency stimulation of the dorsolateral prefrontal
cortex or supplementary motor area. However, reviewers also uniformly cite small sample
sizes, inconsistent results and heterogeneity of treatment protocols as factors reducing
confidence in any positive recommendations (Tikka et al, 2023; Hyde et al, 2022; Fitzimmons
et al, 2022; Pellegrini et al, 2022; Yu et al, 2022; Liang et al, 2021; Lefaucher et al, 2020;
Rapinesi et al, 2019). Liang et al (2021) observe that despite evidence of efficacy, research
into the effect of TMS on OCD stil requires adequately sized and controlled studies.
Rapinesi et al suggest rTMS may be a suitable treatment for patients who do not respond to
pharmacological treatment. This is echoed in the 2017 OCD clinical practice guidelines from
the Indian Psychiatric Society, which suggests TMS only after multiple unsuccessful
medication trials (Janardhan Reddy et al, 2017). In contrast, Pellegrini et al (2022) find that
rTMS is most effective in patients not resistant to medication or who have had only one
unsuccessful medication trial. They therefore recommend TMS earlier rather than later in the
treatment pathway.
Fitzimmons et al (2022) and Yu et al (2022) note large and significant improvements in CGI-S
after rTMS, indicating likelihood of some functional improvement in patients. No other
information on functional outcomes was found.
Page 374 of 425
FOI 24/25- 0013
8. References
Begemann, M. J., Brand, B. A., Ćurčić-Blake, B., Aleman, A., & Sommer, I. E. (2020). Efficacy
of non-invasive brain stimulation on cognitive functioning in brain disorders: a meta-
analysis.
Psychological medicine,
50(15), 2465–2486.
https://doi.org/10.1017/S0033291720003670
Dunner, D. L., Aaronson, S. T., Sackeim, H. A., Janicak, P. G., Carpenter, L. L., Boyadjis, T.,
Brock, D. G., Bonneh-Barkay, D., Cook, I. A., Lanocha, K., Solvason, H. B., &
Demitrack, M. A. (2014). A multisite, naturalistic, observational study of transcranial
magnetic stimulation for patients with pharmacoresistant major depressive disorder:
durability of benefit over a 1-year follow-up period.
The Journal of clinical psychiatry,
75(12), 1394–1401. https://doi.org/10.4088/JCP.13m08977
Elsayed, O. H., Ercis, M., Pahwa, M., & Singh, B. (2022). Treatment-Resistant Bipolar
Depression: Therapeutic Trends, Challenges and Future Directions.
Neuropsychiatric
disease and treatment, 18, 2927–2943. https:/ doi.org/10.2147/NDT.S273503
Fitzsimmons, S. M. D. D., van der Werf, Y. D., van Campen, A. D., Arns, M., Sack, A. T.,
Hoogendoorn, A. W., other members of the TETRO Consortium, & van den Heuvel, O.
A. (2022). Repetitive transcranial magnetic stimulation for obsessive-compulsive
disorder: A systematic review and pairwise/network meta-analysis.
Journal of affective
disorders, 302, 302–312. https:/ doi.org/10.1016/j.jad.2022.01.048
Hett, D., & Marwaha, S. (2020). Repetitive Transcranial Magnetic Stimulation in the Treatment
of Bipolar Disorder.
Therapeutic advances in psychopharmacology, 10,
2045125320973790. https://doi.org/10.1177/2045125320973790
Hyde, J., Carr, H., Kel ey, N., Seneviratne, R., Reed, C., Parlatini, V., Garner, M., Solmi, M.,
Rosson, S., Cortese, S., & Brandt, V. (2022). Efficacy of neurostimulation across mental
disorders: systematic review and meta-analysis of 208 randomized controlled trials.
Molecular psychiatry,
27(6), 2709–2719. https://doi.org/10.1038/s41380-022-01524-8
Gold, A. K., Ornelas, A. C., Ciril o, P., Caldieraro, M. A., Nardi, A. E., Nierenberg, A. A., &
Kinrys, G. (2019). Clinical applications of transcranial magnetic stimulation in bipolar
disorder.
Brain and behavior,
9(10), e01419. https://doi.org/10.1002/brb3.1419
Gutierrez, M. I., Poblete-Naredo, I., Mercado-Gutierrez, J. A., Toledo-Peral, C. L., Quinzaños-
Fresnedo, J., Yanez-Suarez, O., & Gutierrez-Martinez, J. (2022). Devices and
Technology in Transcranial Magnetic Stimulation: A Systematic Review.
Brain sciences,
12(9), 1218. https://doi.org/10.3390/brainsci12091218
Janardhan Reddy, Y. C., Sundar, A. S., Narayanaswamy, J. C., & Math, S. B. (2017). Clinical
practice guidelines for Obsessive-Compulsive Disorder.
Indian journal of psychiatry,
59(Suppl 1), S74–S90. https://doi.org/10.4103/0019-5545.196976
Page 375 of 425
FOI 24/25- 0013
Klomjai, W., Katz, R., & Lackmy-Vallée, A. (2015). Basic principles of transcranial magnetic
stimulation (TMS) and repetitive TMS (rTMS).
Annals of physical and rehabilitation
medicine,
58(4), 208–213. https://doi.org/10.1016/j.rehab.2015.05.005
Lee, J. C., Corlier, J., Wilson, A. C., Tadayonnejad, R., Marder, K. G., Ngo, D., Krantz, D. E.,
Wilke, S. A., Levit , J. G., Ginder, N. D., & Leuchter, A. F. (2021). Subthreshold
stimulation intensity is associated with greater clinical efficacy of intermittent theta-burst
stimulation priming for Major Depressive Disorder.
Brain stimulation,
14(4), 1015–1021.
https://doi.org/10.1016/j.brs.2021.06.008
Lefaucheur, J. P., Aleman, A., Baeken, C., Benninger, D. H., Brunelin, J., Di Lazzaro, V.,
Filipović, S. R., Grefkes, C., Hasan, A., Hummel, F. C., Jääskeläinen, S. K., Langguth,
B., Leocani, L., Londero, A., Nardone, R., Nguyen, J. P., Nyffeler, T., Oliveira-Maia, A.
J., Oliviero, A., Padberg, F., … Ziemann, U. (2020). Evidence-based guidelines on the
therapeutic use of repetitive transcranial magnetic stimulation (rTMS): An update (2014-
2018).
Clinical neurophysiology: official journal of the International Federation of Clinical
Neurophysiology,
131(2), 474–528. https://doi.org/10.1016/j.clinph.2019.11.002
Liang, K., Li, H., Bu, X., Li, X., Cao, L., Liu, J., Gao, Y., Li, B., Qiu, C., Bao, W., Zhang, S., Hu,
X., Xing, H., Gong, Q., & Huang, X. (2021). Ef icacy and tolerability of repetitive
transcranial magnetic stimulation for the treatment of obsessive-compulsive disorder in
adults: a systematic review and network meta-analysis.
Translational psychiatry,
11(1),
332. https://doi.org/10.1038/s41398-021-01453-0
Mann, S. K., & Malhi, N. K. (2023). Repetitive Transcranial Magnetic Stimulation. In
StatPearls. StatPearls Publishing.
Martin, DM, McClintock, SM, Forster, J, Lo, TY, Loo, CK. (2017). Cognitive enhancing effects
of rTMS administered to the prefrontal cortex in patients with depression: A systematic
review and meta-analysis of individual task effects.
Depression and Anxiety. 34: 1029–
1039. https://doi.org/10.1002/da.22658
McQuaid, J. R., Buelt, A., Capaldi, V., Ful er, M., Issa, F., Lang, A. E., Hoge, C., Oslin, D. W.,
Sall, J., Wiechers, I. R., & Wil iams, S. (2022). The Management of Major Depressive
Disorder: Synopsis of the 2022 U.S. Department of Veterans Af airs and U.S.
Department of Defense Clinical Practice Guideline.
Annals of internal medicine,
175(10), 1440–1451. https://doi.org/10.7326/M22-1603
Moses, T. E. H., Gray, E., Mischel, N., & Greenwald, M. K. (2023). Effects of neuromodulation
on cognitive and emotional responses to psychosocial stressors in healthy humans.
Neurobiology of stress, 22, 100515. https://doi.org/10.1016/j.ynstr.2023.100515
Mutz J. (2023). Brain stimulation treatment for bipolar disorder.
Bipolar disorders,
25(1), 9–24.
https://doi.org/10.1111/bdi.13283
Ontario Health (Quality) (2021). Repetitive Transcranial Magnetic Stimulation for People With
Treatment-Resistant Depression: A Health Technology Assessment.
Ontario health
Page 376 of 425
FOI 24/25- 0013
technology assessment series,
21(4), 1–232.
https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/34055112/
Pel egrini, L., Garg, K., Enara, A., Gottlieb, D. S., Wel sted, D., Albert, U., Laws, K. R., &
Fineberg, N. A. (2022). Repetitive transcranial magnetic stimulation (r-TMS) and
selective serotonin reuptake inhibitor-resistance in obsessive-compulsive disorder: A
meta-analysis and clinical implications.
Comprehensive psychiatry,
118, 152339.
https://doi.org/10.1016/j.comppsych.2022.152339
Pohar, R., & Farrah, K. (2019). Repetitive Transcranial Magnetic Stimulation for Patients with
Depression: A Review of Clinical Effectiveness, Cost-Effectiveness and Guidelines – An
Update. Canadian Agency for Drugs and Technologies in Health.
https://www.ncbi.nlm.nih.gov/books/NBK545105/
Janardhan Reddy, Y. C., Sundar, A. S., Narayanaswamy, J. C., & Math, S. B. (2017). Clinical
practice guidelines for Obsessive-Compulsive Disorder.
Indian journal of psychiatry,
59(Suppl 1), S74–S90. https://doi.org/10.4103/0019-5545.196976
Rapinesi, C., Kotzalidis, G. D., Ferracuti, S., Sani, G., Girardi, P., & Del Casale, A. (2019).
Brain Stimulation in Obsessive-Compulsive Disorder (OCD): A Systematic Review.
Current neuropharmacology,
17(8), 787–807.
https://doi.org/10.2174/1570159X17666190409142555
Royal Australian and New Zealand College of Psychiatrists. (2018a). Position Statement –
Repetitive transcranial magnetic stimulation. https://www.ranzcp.org/clinical-guidelines-
publications/clinical-guidelines-publications-library/repetitive-transcranial-magnetic-
stimulation
Royal Australian and New Zealand College of Psychiatrists. (2018b). Professional Practice
Guideline – Administration of repetitive transcranial magnetic stimulation.
https://tmsact.com.au/wp-content/uploads/2020/02/PPG16-Administration-of-repetitive-
transcranial-magnetic-stimulation-rTMS-2.pdf
Schaffer, D. R., Okhravi, H. R., & Neumann, S. A. (2021). Low-Frequency Transcranial
Magnetic Stimulation (LF-TMS) in Treating Depression in Patients With Impaired
Cognitive Functioning.
Archives of clinical neuropsychology : the official journal of the
National Academy of Neuropsychologists,
36(5), 801–814.
https://doi.org/10.1093/arclin/acaa095
Sonmez, A. I., Camsari, D. D., Nandakumar, A. L., Voort, J. L. V., Kung, S., Lewis, C. P., &
Croarkin, P. E. (2019). Accelerated TMS for Depression: A systematic review and meta-
analysis.
Psychiatry research,
273, 770–781.
https://doi.org/10.1016/j.psychres.2018.12.041
Struckmann, W., Persson, J., Gingnell, M., Weigl, W., Wass, C., & Bodén, R. (2021).
Unchanged Cognitive Performance and Concurrent Prefrontal Blood Oxygenation After
Page 377 of 425
FOI 24/25- 0013
Accelerated Intermittent Theta-Burst Stimulation in Depression: A Sham-Controlled
Study.
Frontiers in psychiatry, 12, 659571. https://doi.org/10.3389/fpsyt.2021.659571
Tateishi, H., Mizoguchi, Y., & Monji, A. (2022). Is the Therapeutic Mechanism of Repetitive
Transcranial Magnetic Stimulation in Cognitive Dysfunctions of Depression Related to
the Neuroinflammatory Processes in Depression?.
Frontiers in psychiatry, 13, 834425.
https://doi.org/10.3389/fpsyt.2022.834425
Tikka, S. K., Siddiqui, M. A., Garg, S., Pattojoshi, A., & Gautam, M. (2023). Clinical Practice
Guidelines for the Therapeutic Use of Repetitive Transcranial Magnetic Stimulation in
Neuropsychiatric Disorders.
Indian journal of psychiatry,
65(2), 270–288.
https://doi.org/10.4103/indianjpsychiatry.indianjpsychiatry 492 22
Torres, I. J., Ge, R., McGirr, A., Vila-Rodriguez, F., Ahn, S., Basivireddy, J., Walji, N., Frangou,
S., Lam, R. W., & Yatham, L. N. (2023). Effects of intermittent theta-burst transcranial
magnetic stimulation on cognition and hippocampal volumes in bipolar depression.
Dialogues in clinical neuroscience,
25(1), 24–32.
https://doi.org/10.1080/19585969.2023.2186189
Voigt, J.D., Leuchter, A.F. & Carpenter, L.L. (2021). Theta burst stimulation for the acute
treatment of major depressive disorder: A systematic review and meta-analysis.
Translational Psychiatry,
11, 330. https://doi.org/10.1038/s41398-021-01441-4
Xu, M., Nikolin, S., Samaratunga, N. et al. Cognitive Effects Following Of line High-Frequency
Repetitive Transcranial Magnetic Stimulation (HF-rTMS) in Healthy Populations: A
Systematic Review and Meta-Analysis. (2023) Neuropsychology Review.
https://doi.org/10.1007/s11065-023-09580-9
Yu, L., Li, Y., Yan, J., Wen, F., Wang, F., Liu, J., Cui, Y., & Li, Y. (2022). Transcranial Magnetic
Stimulation for Obsessive-Compulsive Disorder and Tic Disorder: A Quick Review.
Journal of integrative neuroscience,
21(6), 172. https:/ doi.org/10.31083/j.jin2106172
Page 378 of 425
FOI 24/25- 0013
DOCUMENT 35
Evaluation of CANS, ABAS-3 and LSP-16 outcome
measures
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: For each functional outcome measure (CANS; ABAS-3; LSP-16):
• What is the intended population?
• What populations is the measure reliable and valid for?
• How can the measure be used to maximise utility in prediction of care needs?
• What are the limitations?
• What are the risks and benefits of using the measure:
- as a stand alone tool?
- as part of a more comprehensive assessment?
- by a therapist who is unfamiliar with the client?
Date: 23/1/24
Requestor: Sarah s22(1)(a)(ii)
- irrelev
Endorsed by: Shannon s22(1)(a)(ii)
- irrelev
Researcher: Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Aaron s22(1)(a)(ii)
- irrelevant ma
Page 379 of 425
FOI 24/25- 0013
1. Contents
Evaluation of CANS, ABAS-3 and LSP-16 outcome measures ................................................. 1
1.
Contents ....................................................................................................................... 2
2.
Summary ...................................................................................................................... 2
3.
Care and Needs Scale .................................................................................................. 3
4.
Adaptive Behavior Assessment System, 3rd Edition ..................................................... 3
5.
Abbreviated Life Skil s Profile (LSP-16) ........................................................................ 4
6.
Summary of outcome measure features ....................................................................... 6
7.
References ................................................................................................................... 9
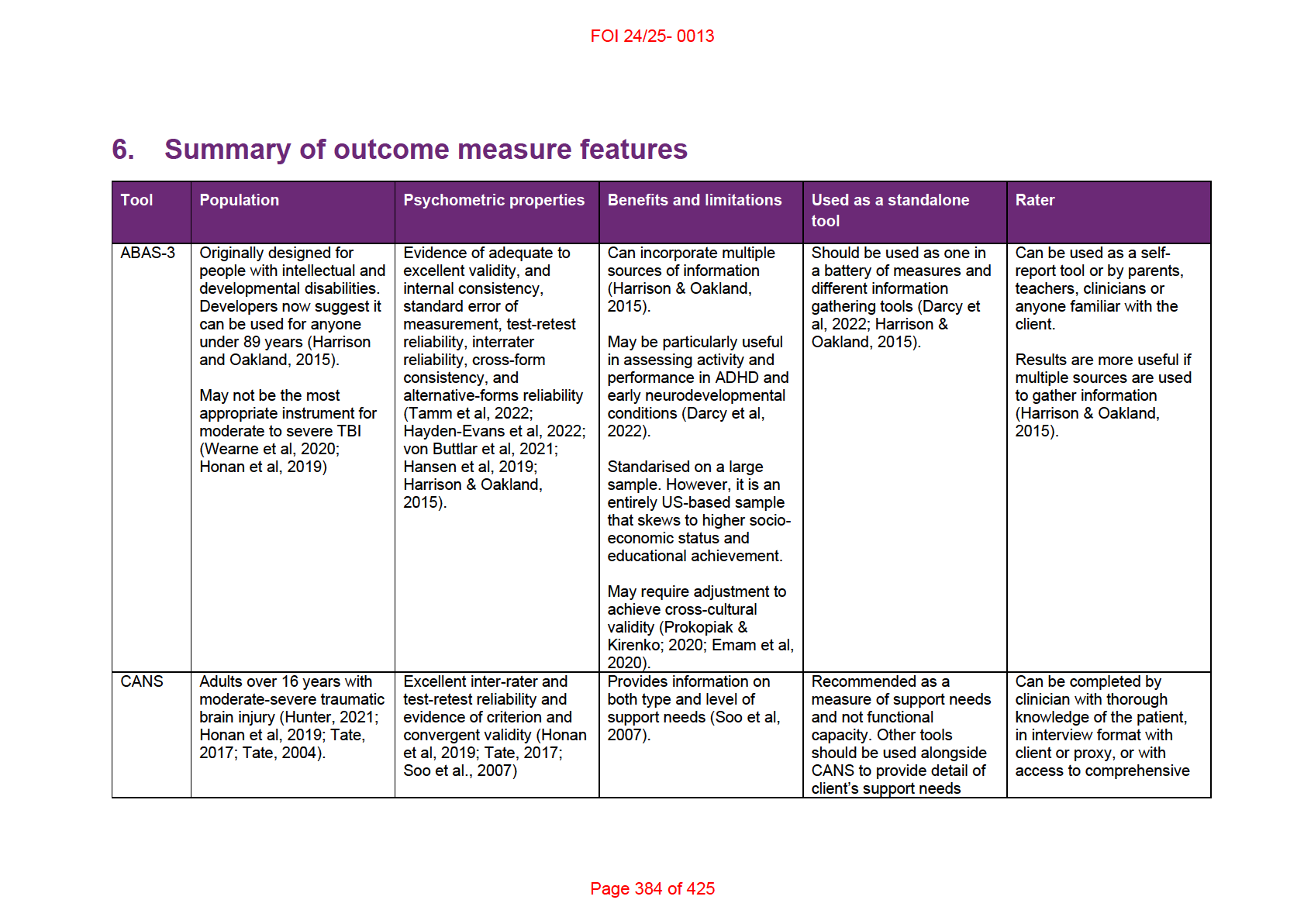
2. Summary
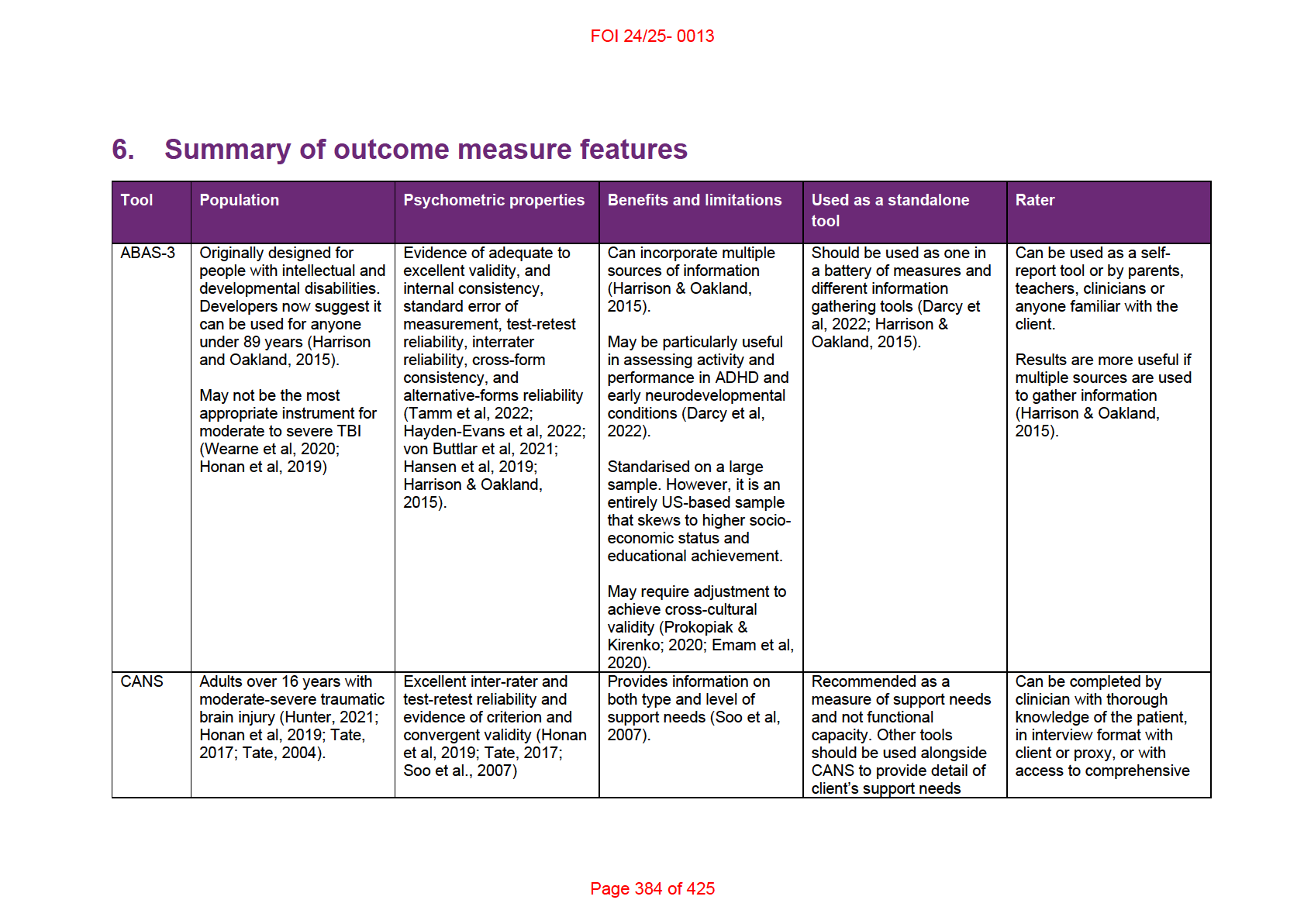
This paper examines the scope, psychometric properties and other features of three
commonly used outcome measures: Care and Needs Scale (CANS), Adaptive Behavior
Assessment System, 3rd Edition (ABAS-3) and Abbreviated Life Skil s Profile (LSP-16).
The outcome measures vary from narrow to general in scope. CANS is intended to assess
support needs for people over 16 years with moderate to severe traumatic brain injury. LSP-16
is designed for adults with severe or chronic mental health conditions. ABAS-3 is more general
and developers suggest it can be used to assess adaptive behaviours for anyone under 89
years.
None of the three outcome measures are intended to be a standalone tool. It is intended that
all three are used in combination with other measures, assessments and information gathering
methods to generate a fuller picture of a person’s functional capacity or support needs.
The source of the information used to completed the assessments varies. ABAS-3 can be
completed by parents, teachers, co-workers, friends or clinicians familiar with the client and it
is recommended that information is collected from multiple sources. LSP-16 is usually
completed by a clinician but preference should be given to the treating professional or support
person with the greatest understanding of the client’s situation. CANS is completed by a
clinician but familiarity may be gained through an informal interview with the client or their
carer/proxy, or by sufficiently detailed medical records.
Results are further summarised in 6. Summary of outcome measure features.
Page 380 of 425
FOI 24/25- 0013
3. Care and Needs Scale
CANS was developed to assess support needs for people over 16 years with moderate to
severe traumatic brain injury (TBI) (Honan et al, 2019; Tate, 2017; Soo et al, 2007). A version
for younger people (PCANS) was also developed (Tate et al, 2014; Soo et al, 2010). CANS
can be completed in an interview format with the client or proxy or by a clinician with sufficient
knowledge of the client (Tate, 2017). The manual also notes:
the CANS can be completed on the basis of information derived from the patient’s
medical record, scales of disability and so forth. In situations where the clinician has
knowledge of the patient/client and direct interview is not required, the CANS wil only
take a few minutes to complete. Interview format with an informant generally takes
somewhat longer (10-15 mins)." (Tate, 2017, p.11)
Few studies have examined the psychometric properties of the CANS. The only studies found
were authored by the developers. Existing evidence indicates excellent inter-rater and test-
retest reliability as well as adequate convergent and criterion validity (Tate, 2017; Soo et al,
2007; Tate, 2004).
There are some sources of potential bias which may impact reliability. For example, Honan et
al (2019) note that the assessment depends on subjective judgement of the clinician and that
training is required in order to achieve high levels of inter-rater reliability. Further, the manual
states that it is not advised to separate out the support needs that may be due to conditions
other than TBI, such as support needs due to health conditions or aging (Tate, 2017).
However, this may impact reliability given that CANS has only been validated for TBI
populations and not general or other clinical cohorts.
4. Adaptive Behavior Assessment System, 3rd Edition
ABAS-3 was originally designed for people with intellectual and developmental conditions. It
has been standardised on a large scale and developers now suggest it can be used for
anyone under the age of 89 years, including:
persons who exhibit the effects of trauma, display attention-deficit/hyperactivity disorder
(ADHD), disruptive behaviors, anxiety disorders, mood disorders, neurocognitive
impairments, autism spectrum disorder (ASD), developmental delays and disorders,
eating disorders, health impairment, language disorders, learning disabilities and
disorders, neurobehavioral and neurodevelopmental disorders, motor impairment,
physical disabilities, personality disorders, psychotic and thought disorders, sensory
impairments, sleep disorders, substance-related disorders, or traumatic brain injury
(Harrison & Oakland, 2015, p.57).
Most evidence of psychometric properties of ABAS-3 comes from studies conducted by the
tool’s developers (Hayden-Evans et al, 2022). There is evidence of excellent internal
consistency, test-retest reliability and adequate to excellent inter-rater reliability and alternate-
Page 381 of 425
FOI 24/25- 0013
forms reliability. There is evidence of excellent content, construct and criterion validity
(Hayden-Evans et al, 2022; Harrison & Oakland, 2015.
Validity studies targeted at specific populations were conducted for autism, intellectual
disability, and ADHD. In addition, validity studies were conducted for the second edition
(ABAS-II) for people with:
developmental delay, low birth weight, perinatal respiratory distress, chromosomal
abnormalities, fetal alcohol syndrome and prenatal drug exposure, Down syndrome,
motor and physical disorders, expressive and receptive language disorders, behavioural
and emotional issues, learning disabilities, and hearing impairments; adults with
Alzheimer's and unspecified neuro-psychological disorders (Harrison & Oakland, 2015,
p.127).
The developers argue that ABAS-II is sufficiently similar to ABAS-3 for the previous version’s
evidence to stand in favour of the current version (Harrison & Oakland, 2015). However, there
are some notable differences. For example, ABAS-3 scores are generally higher than ABAS-II
scores (von Buttlar et al, 2021; Harrison & Oakland, 2015).
Some limitations were described in the literature. Despite evidence of good psychometric
properties, Hayden-Evans et al (2022) note that ABAS-3 does not have very good coverage
against the International Classification of Functioning, Disability and Health (ICF) codes
deemed most relevant to children with autism. Further, while efforts were made to ensure
ABAS-3 was comprehensive, it should not be relied on as the sole instrument of assessment.
Clinicians should also look to other data such as “information derived from concurrent or
former assessments; detailed interviews and history taking; developmental, school, or work
records; and direct observations" (Harrison & Oakland, 2015, p.7).
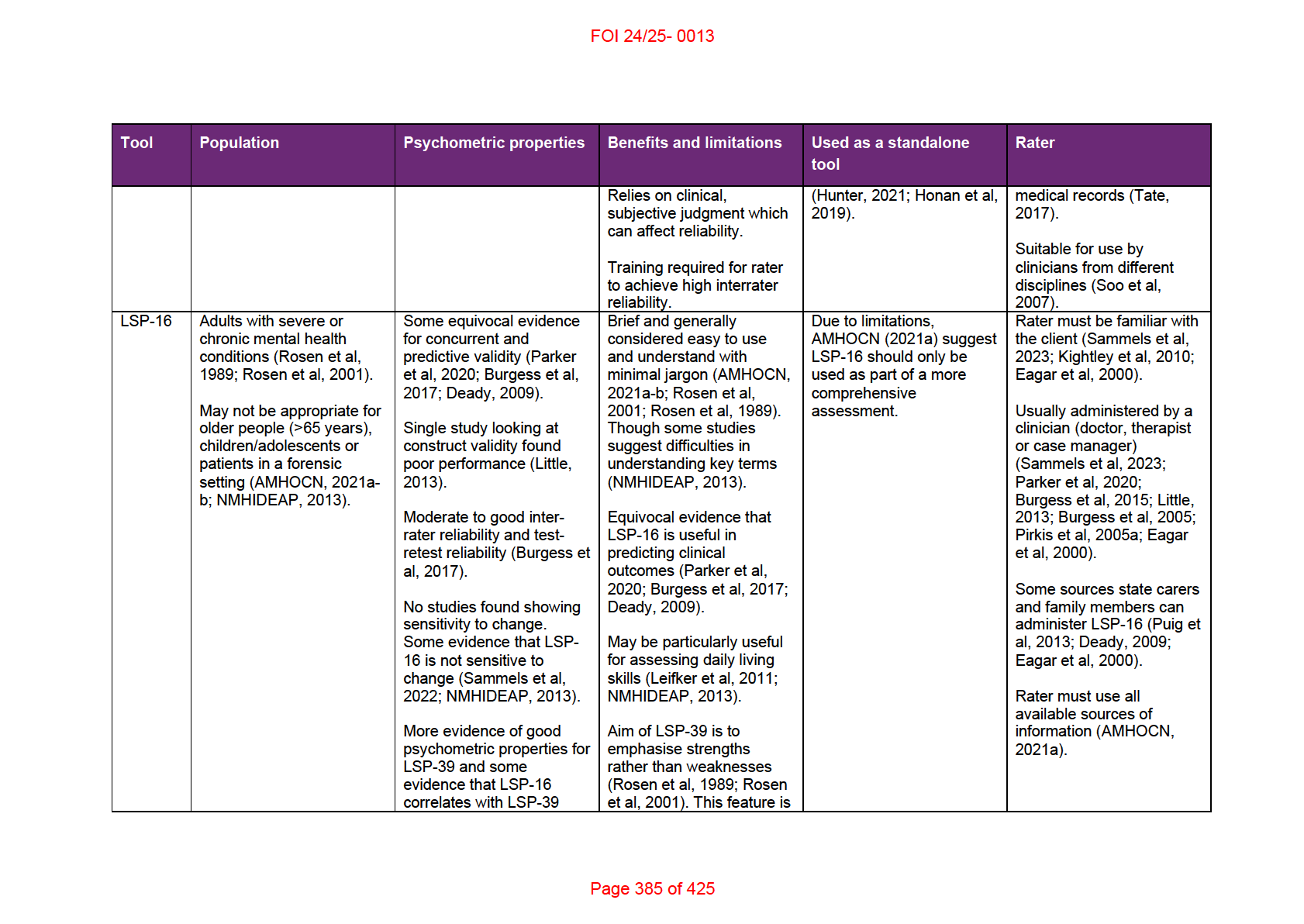
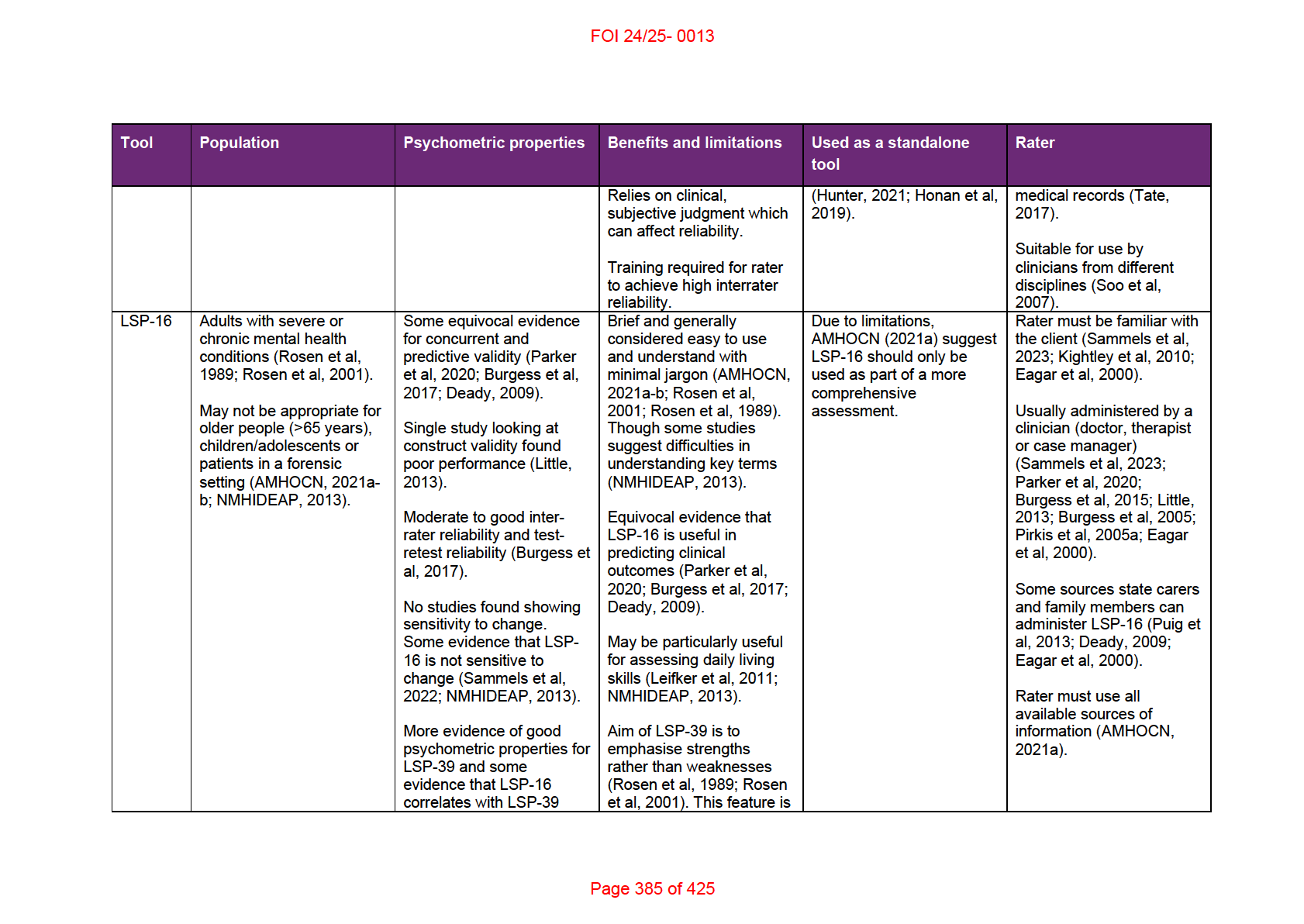
5. Abbreviated Life Skil s Profile
LSP-16 is a measure of community functioning and disability for people with severe or chronic
mental health conditions (Little, 2013; Kightley et al, 2010; Pirkis et al, 2005a; Rosen et al,
2001). It was developed for Australian public mental health services to reduce the rating
burden on clinicians (NMHIDEAP, 2013; Little, 2013; Pirkis et al, 2005a). As part of the
National Outcome Casemix Collection (NOCC), LSP-16 is now required to be used at certain
points in the treatment cycle for adults receiving specialised public sector mental health
services across Australia (AMHOCN, 2021a; Little, 2013; Rosen et al, 2001).
It is a shortened form of the 39 item Life Skills Profile (LSP-39). Rosen et al (1989) developed
the original LSP-39 to assess the daily functioning of people with schizophrenia and it has
since been applied generally for people with mental health or psychiatric conditions (Burgess
et al, 2017; Deady et al, 2005; Pirkis et al, 2005a). The developers note that only a few of the
items in the Communication subscale of LSP-39 related directly to features specific to
schizophrenia (Rosen et al, 1989). The Communication subscale was removed in the
development of LSP-16 (Deady et al, 2005; Rosen et al, 2001).
Page 382 of 425
FOI 24/25- 0013
Few studies have investigated the psychometric properties of LSP-16. There is equivocal
evidence of concurrent and predictive validity. It was shown to correlate with Health of the
Nation Outcome Scale and LSP-39 but not with the Behaviour and Symptom Identification
Scale (Burgess et al, 2017). There is some evidence that LSP-16 can predict clinical outcomes
such as hospital admission and length of stay, though other studies were not able to find
significant correlations (Parker et al, 2020; Burgess et al, 2017; Deady, 2009). There is
evidence of poor construct validity (Little, 2013). Studies have found moderate to good inter-
rater reliability and test-retest reliability (Burgess et al, 2017). Some studies suggest potential
problems for LSP-16’s sensitivity to change but no study has investigated this directly
(Sammels et al, 2022; NMHIDEAP, 2013).
More research has been conducted on the psychometric properties of LSP-39. The longer
version has been shown to be a valid and reliable measure for people with schizophrenia and
severe mental health issues. There is evidence that LSP-39 has moderately good content,
construct, concurrent and predictive validity, adequate inter-rater reliability, high test-retest
reliability and good sensitivity to change (Burgess et al, 2017; Deady, 2009; Pirkis et al,
2005a).
Some argue that evidence for LSP-39 can be used to support the validity and reliability of LSP-
16 as all 16 items of the abbreviated form are included in the longer version (Pirkis et al,
2005a; Rosen et al, 2001). And LSP-16 has been shown to correlate with LSP-39 (Burgess et
al, 2017; Rosen et al, 2001). However, there are some important differences between the two
forms. For example, LSP-39 is a strengths-based scale with higher scores indicating greater
functioning in a particular task, whereas LSP-16 is an impairment-based scale with higher
scores indicating greater impairment (Pirkis et al, 2005a; Rosen et al, 2001).
Several limitations of LSP-16 have been identified. A review of the NOOC in 2013
recommended removing the LSP-16 from the collection due to its reported limitations. Despite
the measure being mandatory, the 3-month period between reviews meant that it was not
administered to most service users, who are in community rehabilitation settings for less than
3 months. While its use in capturing some information around daily living skil s in adults was
seen as useful, it was found to be inappropriate for children and adolescents, older people and
those in a forensic setting. In addition:
Issues were noted in relation to particular items, including domains that are not
captured, the glossary and the language of the measure. Participants consistently raised
concerns regarding items 10, 11 and 16, which they thought required clarification in the
glossary. Some participants suggested that the tool does not capture fluctuations in
functioning between reviews, which they thought was of particular clinical relevance.
The language was felt to be outdated, not strengths based and not supporting the
recovery agenda.. Participants suggested that there were more useful types of
information to collect, including capturing aspects of social inclusion (NMHIDEAP, 2013,
p.130).
Page 383 of 425
FOI 24/25- 0013
7. References
Australian Mental Health Outcomes and Classification Network. (2021a).
National Outcomes
and Casemix Collection (NOCC) basic training manual: adult services 2nd Edition.
https://www.amhocn.org/__data/assets/pdf_file/0003/731019/Adult-Basic-NOCC-
Training-Manual.pdf
Australian Mental Health Outcomes and Classification Network. (2021b).
National Outcomes
and Casemix Collection (NOCC) basic training manual: child and adolescent services.
https://www.amhocn.org/ data/assets/pdf file/0019/731026/Child-Adolescent-Basic-
NOCC-Training-Manual.pdf
Australian Mental Health Outcomes and Classification Network. (2021c).
Rater and clinical
utility training manual: Adult. Rev. ed. Sydney: Australian Mental Health Outcomes and
Classification Network.
https://www.amhocn.org/ data/assets/pdf file/0004/694030/Adult Rater Clinical Utilit
y Training Manual 100523.pdf
Australian Mental Health Outcomes and Classification Network. (2021d). Rater and clinical
utility training manual: Child and adolescent. Rev. ed. Sydney: Australian Mental Health
Outcomes and Classification Network.
https://www.amhocn.org/ data/assets/pdf file/0009/694467/CA Rater-and-Clinical-
Utility-Manual-100523.pdf
Burgess, P. M., Harris, M. G., Coombs, T., & Pirkis, J. E. (2017). A systematic review of
clinician-rated instruments to assess adults' levels of functioning in specialised public
sector mental health services.
The Australian and New Zealand journal of psychiatry,
51(4), 338–354. https:/ doi.org/10.1177/0004867416688098
Burgess, P., Pirkis, J., & Coombs, T. (2015). Routine outcome measurement in Australia.
International review of psychiatry,
27(4), 264–275.
https://doi.org/10.3109/09540261.2014.977234
Burgess, P., Coombs, T., Clarke, A., Dickson, R., & Pirkis, J. (2012). Achievements in mental
health outcome measurement in Australia: Reflections on progress made by the
Australian Mental Health Outcomes and Classification Network (AMHOCN).
International journal of mental health systems,
6(1), 4. https://doi.org/10.1186/1752-
4458-6-4
D'Arcy, E., Wal ace, K., Chamberlain, A., Evans, K., Milbourn, B., Bölte, S., Whitehouse, A. J.,
& Girdler, S. (2022). Content validation of common measures of functioning for young
children against the International Classification of Functioning, Disability and Health and
Code and Core Sets relevant to neurodevelopmental conditions.
Autism : the
international journal of research and practice,
26(4), 928–939.
https://doi.org/10.1177/13623613211036809
Page 387 of 425
FOI 24/25- 0013
Deady, M. (2009).
A review of screening, assessment and outcome measures for drug and
alcohol settings. Drug and Alcohol and Mental Health Information Management Project.
Sydney: NSW Department of Health.
https://www.drugsandalcohol.ie/18266/1/NADA A Review of Screening%2C Assess
ment and Outcome Measures for Drug and Alcohol Settings.pdf
Eagar K, Buckingham B, Coombs T, Trauer T, Graham C, Eagar L & Callaly T. (2000).
Outcome Measurement in Adult Area Mental Health Services: Implementation
Resource Manual. Department of Human Services Victoria.
https://www.vgls.vic.gov.au/client/en_AU/search/asset/1160101/0
Emam, M. M., Al-Sulaimani, H., Omara, E., & Al-Nabhany, R. (2019). Assessment of adaptive
behaviour in children with intellectual disability in Oman: an examination of ABAS-3
factor structure and validation in the Arab context.
International journal of
developmental disabilities,
66(4), 317–326.
https://doi.org/10.1080/20473869.2019.1587939
Hansen, L. (2019). A Concurrent validity study of the Missouri Adaptive Ability Scale and the
Adaptive Behavior Assessment System, Third Edition — Teacher Form. Murray State
Theses and Dissertations. 149. https://digitalcommons.murraystate.edu/etd/149
Harrison, P. L., & Oakland, T. (2015). ABAS-3. Torrance: Western Psychological Services.
Hayden-Evans, M., Milbourn, B., D’Arcy, E., Chamberlain, A., Afsharnejad, B., Evans, K., ... &
Girdler, S. (2022). An evaluation of the overal utility of measures of functioning suitable
for school-aged children on the autism spectrum: A scoping review.
International
Journal of Environmental Research and Public Health,
19(21), 14114.
Honan, C. A., McDonald, S., Tate, R., Ownsworth, T., Togher, L., Fleming, J., Anderson, V.,
Morgan, A., Catroppa, C., Douglas, J., Francis, H., Wearne, T., Sigmundsdottir, L., &
Ponsford, J. (2019). Outcome instruments in moderate-to-severe adult traumatic brain
injury: recommendations for use in psychosocial research.
Neuropsychological
rehabilitation,
29(6), 896–916. https://doi.org/10.1080/09602011.2017.1339616
Hunter, S. (2021).
Occupational Therapy Australia response to question taken on notice at
public hearing in Melbourne on 23 April 2021. Occupational Therapy Australia.
https://everyaustraliancounts.com.au/wp-content/uploads/QoN 03 IA.pdf
Kightley, M., Einfeld, S., & Hancock, N. (2010). Routine outcome measurement in mental
health: feasibility for examining effectiveness of an NGO.
Australasian psychiatry :
bulletin of Royal Australian and New Zealand College of Psychiatrists,
18(2), 167–169.
https://doi.org/10.3109/10398560903473660
Leifker, F. R., Patterson, T. L., Heaton, R. K., & Harvey, P. D. (2011). Validating measures of
real-world outcome: the results of the VALERO expert survey and RAND panel.
Schizophrenia bulletin,
37(2), 334–343. https://doi.org/10.1093/schbul/sbp044
Page 388 of 425
FOI 24/25- 0013
Little J. (2013). Multilevel confirmatory ordinal factor analysis of the Life Skil s Profile-16.
Psychological assessment,
25(3), 810–825. https://doi.org/10.1037/a0032574
National Mental Health Information Development Expert Advisory Panel. (2013).
Mental Health
National Outcomes and Casemix Collection: NOCC Strategic Directions 2014 – 2024.
Commonwealth of Australia, Canberra. https:/ www.amhocn.org/training-and-service-
development/special-projects/nocc-strategic-directions-2014-2024
Parker, S., Arnautovska, U., Siskind, D., Dark, F., McKeon, G., Korman, N., & Harris, M.
(2020). Community-care unit model of residential mental health rehabilitation services in
Queensland, Australia: Predicting outcomes of consumers 1-year post discharge.
Epidemiology and Psychiatric Sciences, 29, E109.
https://doi.org/10.1017/S2045796020000207
Pirkis, J., Burgess, P., Kirk, P., Dodson, S., & Coombs, T. (2005a).
Review of standardised
measures used in the National Outcomes and Casemix Collection (NOCC). New South
Wales Institute of Psychiatry. http:/ hdl.handle.net/10536/DRO/DU:30073558
Pirkis, J., Burgess, P., Coombs, T., Clarke, A., Jones-Ellis, D., & Dickson, R. (2005b). Routine
measurement of outcomes in Australia's public sector mental health services.
Australia
and New Zealand health policy,
2(1), 8. https://doi.org/10.1186/1743-8462-2-8
Prokopiak, A. & Kirenko, J. (2020). ABAS-3 – an instrument for assessing adaptive skil s in
people with an intellectual disability.
Hrvatska revija za rehabilitacijska istraživanja,
56(2), 154-168. https://doi.org/10.31299/hrri.56.2.9
Puig, O., Penadés, R., Baeza, I., De la Serna, E., Sánchez-Gistau, V., Lázaro, L., Bernardo,
M., & Castro-Fornieles, J. (2013). Assessment of real-world daily-living skills in early-
onset schizophrenia trough the Life Skil s Profile scale.
Schizophrenia research,
145(1-
3), 95–100. https://doi.org/10.1016/j.schres.2012.12.026
Rosen, A., Hadzi-Pavlovic, D., & Parker, G. (1989). The life skil s profile: a measure assessing
function and disability in schizophrenia.
Schizophrenia bulletin,
15(2), 325–337.
https://doi.org/10.1093/schbul/15.2.325
Rosen, A., Trauer, T., Hadzi-Pavlovic, D., & Parker, G. (2001). Development of a brief form of
the Life Skil s Profile: the LSP-20.
The Australian and New Zealand journal of
psychiatry,
35(5), 677–683. https://doi.org/10.1080/0004867010060518
Sammells, E., Logan, A., & Sheppard, L. (2023). Participant Outcomes and Facilitator
Experiences Following a Community Living Skil s Program for Adult Mental Health
Consumers.
Community mental health journal,
59(3), 428–438.
https://doi.org/10.1007/s10597-022-01020-x
Soo, C., Tate, R. L., Anderson, V., & Waugh, M.-C. (2010). Assessing care and support needs
for children with acquired brain injury: Normative data for the Paediatric Care and
Needs Scale (PCANS).
Brain Impairment,
11(2), 183–196.
https://doi.org/10.1375/brim.11.2.183
Page 389 of 425
FOI 24/25- 0013
Soo, C., Tate, R., Hopman, K., Forman, M., Secheny, T., Aird, V., Browne, S., & Coulston, C.
(2007). Reliability of the care and needs scale for assessing support needs after
traumatic brain injury.
The Journal of head trauma rehabilitation,
22(5), 288–295.
https://doi.org/10.1097/01.HTR.0000290973.01872.4c
Tate, R.L. (2017).
Manual for the Care and Needs Scale (CANS). Unpublished manuscript.
John Walsh Centre for Rehabilitation Research, University of Sydney. Updated version
2. https:/ www.sydney.edu.au/content/dam/corporate/documents/faculty-of-medicine-
and-health/research/centres-institutes-groups/Care-and-needs-scale-manual.pdf
Tate, R. L. (2004). Assessing support needs for people with traumatic brain injury: the care
and needs scale (CANS),
Brain Injury,
18(5), 445-460,
https://doi.org/10.1080/02699050310001641183
Tamm, L., Day, H. A., & Duncan, A. (2022). Comparison of Adaptive Functioning Measures in
Adolescents with Autism Spectrum Disorder Without Intellectual Disability.
Journal of
autism and developmental disorders,
52(3), 1247–1256. https://doi.org/10.1007/s10803-
021-05013-9
von Buttlar, A. M., Zabel, T. A., Pritchard, A. E., & Cannon, A. D. (2021). Concordance of the
Adaptive Behavior Assessment System, second and third editions.
Journal of
intellectual disability research : JIDR,
65(3), 283–295. https:/ doi.org/10.1111/jir.12810
Wearne, T., Anderson, V., Catroppa, C., Morgan, A., Ponsford, J., Tate, R., Ownsworth, T.,
Togher, L., Fleming, J., Douglas, J., Docking, K., Sigmundsdottir, L., Francis, H.,
Honan, C., & McDonald, S. (2020). Psychosocial functioning following moderate-to-
severe pediatric traumatic brain injury: recommended outcome instruments for research
and remediation studies.
Neuropsychological rehabilitation,
30(5), 973–987.
https://doi.org/10.1080/09602011.2018.1531768
Page 390 of 425
FOI 24/25- 0013
DOCUMENT 36
Thermoregulation and air conditioning
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: What medical conditions or disabilities involve an impairment in thermoregulation?
What cooling systems are available for use in Australia?
Is air conditioning effective in managing symptoms of thermoregulation impairment
compared to other cooling systems?
Date: 8/2/2024
Requestor: Helen s22(1)(a)(ii) - irrelevant material
Endorsed by: Melinda s22(1)(a)(ii) - irrelevant ma
Researcher: Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Stephanie s22(1)(a)(ii) - irrelevant mat
Page 391 of 425
FOI 24/25- 0013
1. Contents
Thermoregulation and air conditioning ....................................................................................... 1
1.
Contents ....................................................................................................................... 2
2.
Summary ...................................................................................................................... 3
3.
Human thermoregulation .............................................................................................. 4
3.1 Thermoeffectors ........................................................................................................ 4
4.
Conditions resulting in thermoregulation impairment .................................................... 5
4.1 Spinal cord injury ....................................................................................................... 7
4.2 Acquired brain injury .................................................................................................. 7
4.3 Parkinson’s Disease .................................................................................................. 8
4.4 Multiple Sclerosis ....................................................................................................... 8
4.5 Peripheral neuropathy ............................................................................................... 9
4.6 Psychosocial conditions ............................................................................................. 9
4.7 Epilepsy and seizure disorders ................................................................................ 10
4.8 Autism ...................................................................................................................... 10
4.9 Motor neurone disease / Amyotrophic lateral sclerosis............................................ 11
4.10 Huntington’s disease ............................................................................................ 11
4.11 Severe burns ........................................................................................................ 12
5.
Management of thermoregulation impairment ............................................................ 12
5.1 Air conditioning compared to other cooling strategies ............................................. 13
6.
Air conditioning and other cooling systems ................................................................. 14
6.1 Cooling garments .................................................................................................... 14
6.2 Fans ......................................................................................................................... 15
6.3 Evaporative cooling ................................................................................................. 15
6.4 Air conditioning (refrigerated cooling) ...................................................................... 15
7.
Air conditioning use in Australia .................................................................................. 17
8.
References ................................................................................................................. 19
Page 392 of 425
FOI 24/25- 0013
2. Summary
Note: This paper is a substantial revision of a research paper originally completed in October
2019 and reviewed in February 2024.
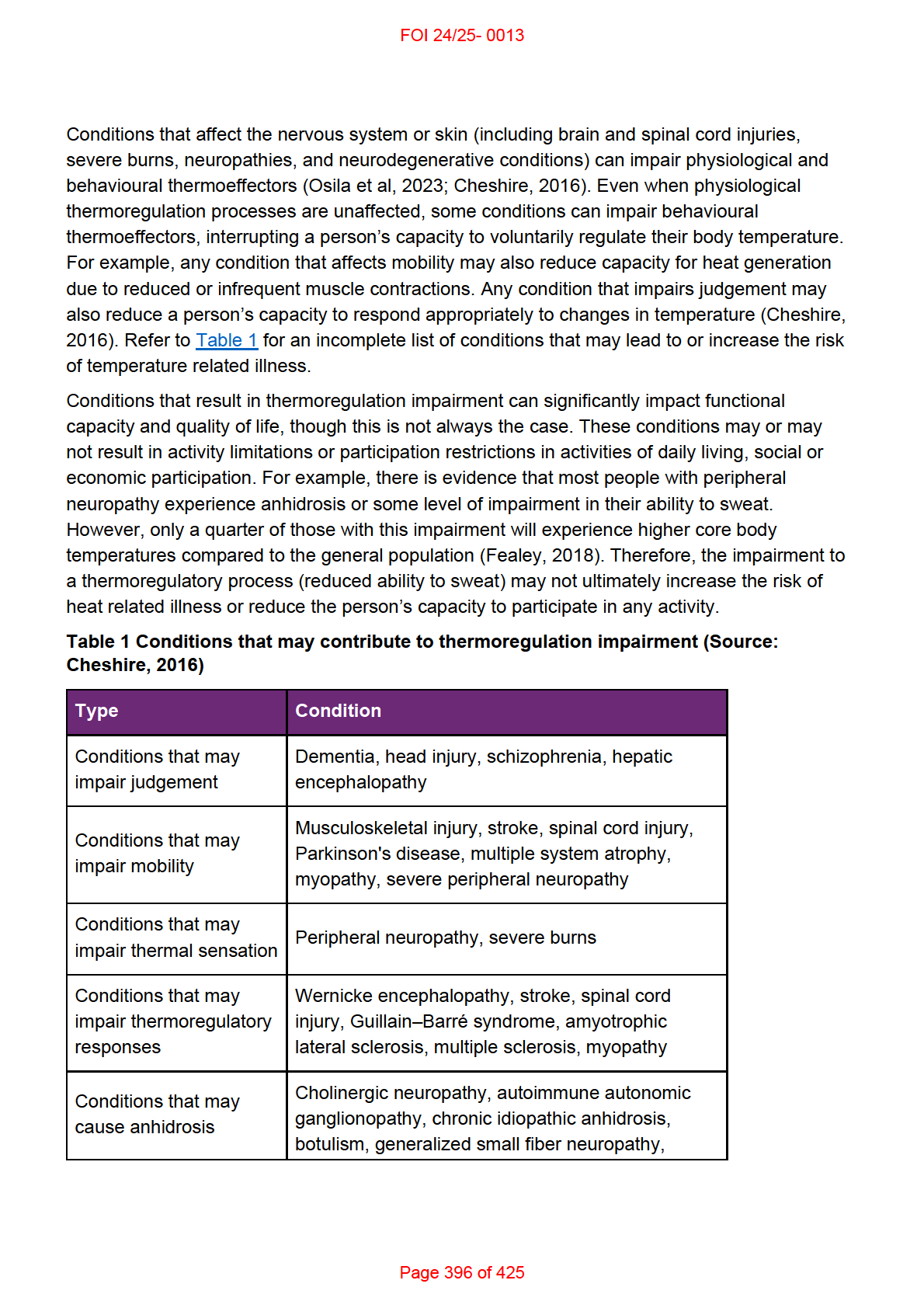
Thermoregulation impairment can result from a wide range of health conditions and
disabilities. The human thermoregulatory system involves perceptual, physiological and
behavioural components. A condition may result in a thermoregulatory impairment if it affects
the peripheral or central nervous systems, or if the condition impacts strength, mobility, motor
control, cognition or emotional regulation.
The main types of cooling systems found in Australian homes are fans, evaporative and
refrigerative air conditioners. Refrigerative air conditions, including reverse cycle air
conditioners, are the most common type of air conditioner used in Australia. The cost-
effectiveness of cooling systems depends on several factors including climate, location, energy
prices, architectural features of the home, device running time, temperature set-point and other
lifestyle factors.
There is evidence for the benefits of air conditioner use in the general population to manage
the effects of heat, especially in very hot and dry climates. However, there is very little
evidence comparing air conditioning with other cooling devices or strategies and very little
experimental evidence showing the circumstances in which air conditioning might contribute to
managing the symptoms of thermoregulation impairment.
Despite this, public health messaging and recommendations from researchers and clinicians
are consistent. They suggest that simple behavioural strategies and easily accessible cooling
devices have a role in managing the symptoms of thermoregulation impairment. Behavioural
strategies include:
• understanding personal heat tolerance and preferences
• staying inside during the hotter times of day
• planning outdoor or strenuous activities for cooler times of day
• wearing loose or light clothing
• wearing wet clothes or wraps
• taking regular breaks from activity
• consuming cold foods and drinks
• taking cold baths or showers.
Recommended equipment or devices include:
• space coolers (including evaporative coolers and air conditioning)
• electric fans
• cooling garments.
Page 393 of 425
FOI 24/25- 0013
3. Human thermoregulation
Humans are homeothermic animals, which means that human body temperature is maintained
at a nearly constant level largely, but not entirely, independent of the environment. Core
human body temperature is maintained at around 37°C (+/- 0.5°C), while peripheral body
temperature may vary more widely (Romanovsky, 2018; Cheshire, 2016).
When the core body temperature is too low, this is called hypothermia. When the core body
temperature is too high, this is called hyperthermia. Some sources refer to hypo and
hyperthermia as any variation outside the normal range of core body temperature.
(Romanovsky, 2018). Other sources define states more specifically as below 35°C for
hypothermia and above 40°C for hyperthermia (Cheshire, 2016).
Slight changes outside the accepted range can be controlled with physiological or behavioural
responses. Extreme changes to core body temperature may lead to significant injury or death
(Osila et al, 2023; Cheshire, 2016). Age can affect the ability to regulate body temperature due
to both physiological changes (such as changes in metabolism or the cardiovascular system)
and behavioural changes (spending more time at home, reduced activity), which is why older
people are more susceptible to complications from environmental extremes (Osila et al, 2023;
Bennetts et al, 2020).
Thermoregulation is the process of maintaining body temperature by balancing heat
generation and heat loss. Temperature variations are picked up by thermoreceptors on the
skin or inside the body. These receptors alert the thermoregulatory centre located in the
hypothalamus to enact thermoeffectors, physiological or behavioural responses that regulate
body temperature.
3.1 Thermoeffectors
Physiological thermoeffectors are involuntary body processes that help to control heat loss or
heat generation. They include:
• skin vasodilation or vasoconstriction
• sweating
• shivering
• piloerection
• panting.
Behavioural thermoeffectors are voluntary or instinctual complex behaviours. They include
behaviours such as changing posture, drinking water, adding or removing clothing, turning on
a fan or air conditioning etc (Osila et al, 2023; Romanovsky, 2018).
Thermoeffectors aid in heat loss, conservation or generation by affecting one or more of the
four processes of heat exchange: conduction, convection, radiation, and evaporation (Osila et
al, 2023; Romanovsky, 2018; Cheshire, 2016).
Page 394 of 425
FOI 24/25- 0013
Conduction
Conduction occurs when heat is transferred from one object to another object in direct contact.
Materials with high conductivity are more able to draw heat away from the body. For example,
water has a high conductivity and so submersion in water is a good way to draw heat from the
body (Osila et al, 2023; Romanovsky, 2018).
Convection
Convection occurs when a body is submerged in a gas or liquid. Movement of the fluid
replaces layers of fluid closer to the body with fluid further from the body. The layers of fluid
closer to the body have a temperature closer to the temperature of the skin, while the more
distant fluid has a temperature closer to the ambient temperature. Convection therefore
intensifies conduction. If the environment is hotter, the body is exposed to hotter material and
so heats up faster. If the environment is colder, the body is exposed to colder material and so
cools down faster. For example, a ceiling fan cools by convection by increasing movement of
air on the skin, removing warmer air closer to the body and replacing it with cooler air further
from body (Osila et al, 2023; Romanovsky, 2018).
Radiation
All materials emit and absorb heat via radiation in the form of electromagnetic waves. The
human body loses approximately 60% of its heat via radiation. Unlike conduction or
convection, radiation does not require contact with a medium. For example, solar radiation can
warm the earth despite passing through colder layers of earth’s atmosphere (Osila et al, 2023;
Connor, 2022; Romanovsky, 2018; Cheshire, 2016).
Evaporation
Liquid requires energy in the form of heat to evaporate. The heat required is drawn from the
environment or from the liquid itself and transferred from the liquid to the gas. For example,
animals make use of evaporative cooling in the form of sweating and panting (Osila et al,
2023; Romanovsky, 2018; Lohner, 2017). Evaporation accounts for about 22-30% of heat lost
from the body (Osila et al, 2023; Cheshire, 2016). Evaporation is the most efficient form of
heat loss in the human body, though it can be less effective in more humid environments and
does consume large amounts of water. Evaporation is the only form of heat transfer that also
works when the ambient temperature is higher than the temperature of the skin (Romanovsky,
2018).
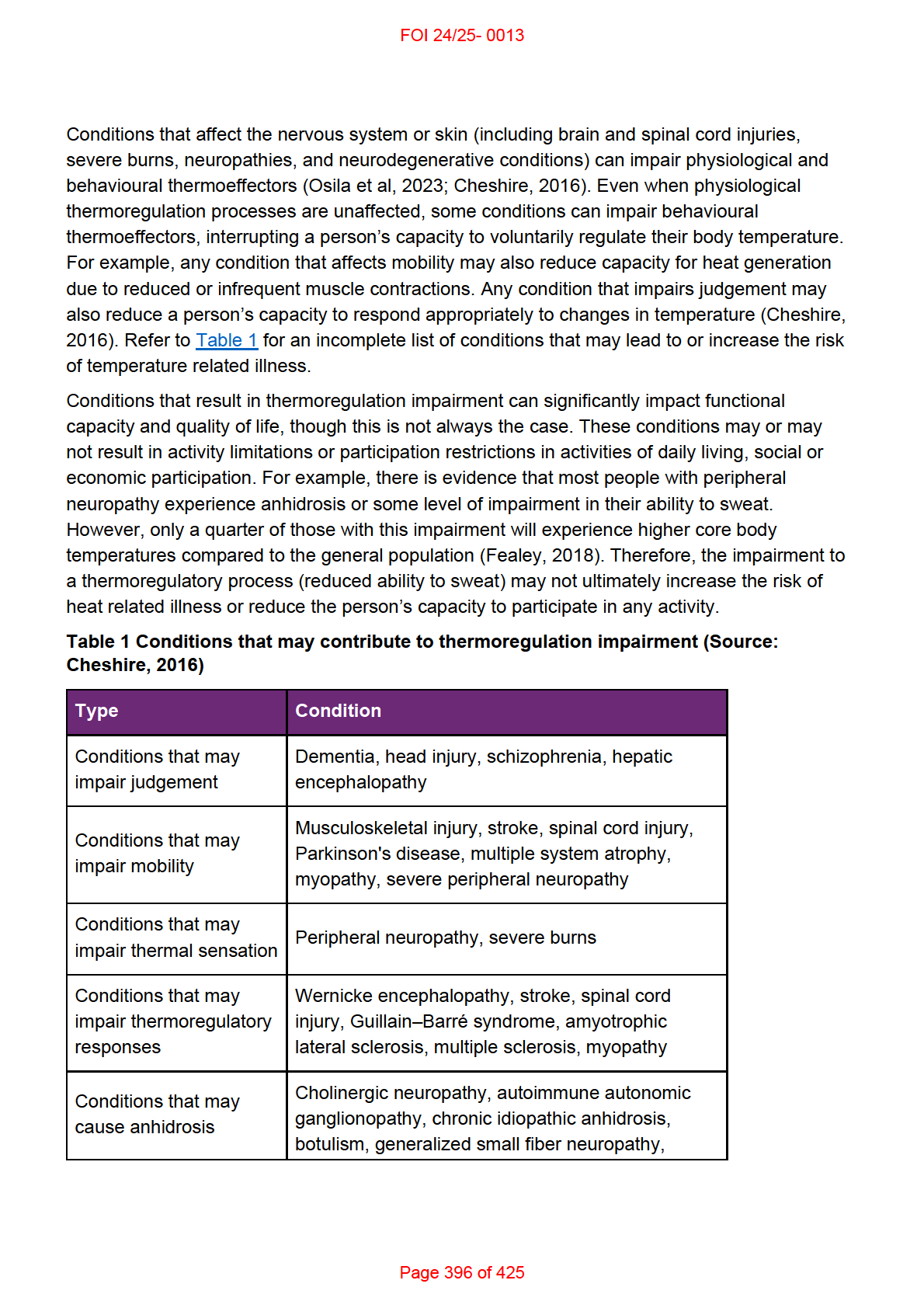
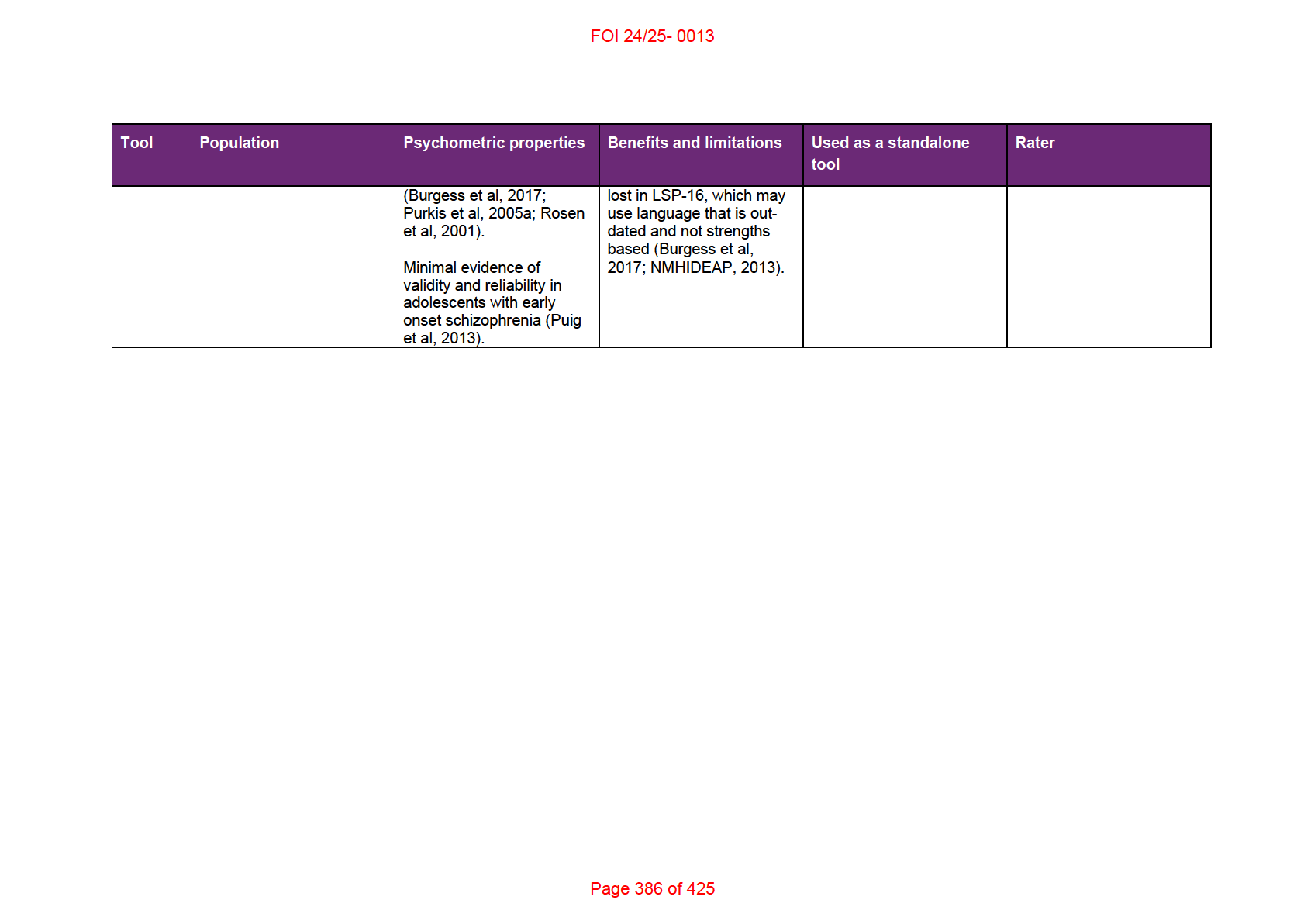
4. Conditions resulting in thermoregulation impairment
Some conditions can impair our thermoregulatory processes and therefore increase the risk of
temperature related health problems. The sections below describe some, though not all,
conditions for which there is evidence of thermoregulatory impairment. For most conditions,
whether thermoregulation impairment occurs, or whether the impairment is substantial and
results in activity limitations or participation restrictions, will vary for individuals.
Page 395 of 425
FOI 24/25- 0013
Sjögren syndrome, multiple system atrophy,
Fabry's disease, bilateral cervical sympathectomy
Conditions that may
Status epilepticus, neuroleptic malignant
increase thermogenesis syndrome, malignant hyperthermia
Other conditions that
Hypoglycemia, Diabetic ketoacidosis,
may lead to
Hypothyroidism, Adrenal failure, Hypopituitarism,
thermoregulatory
Renal failure, Shock, Sepsis, Anorexia nervosa,
impairment
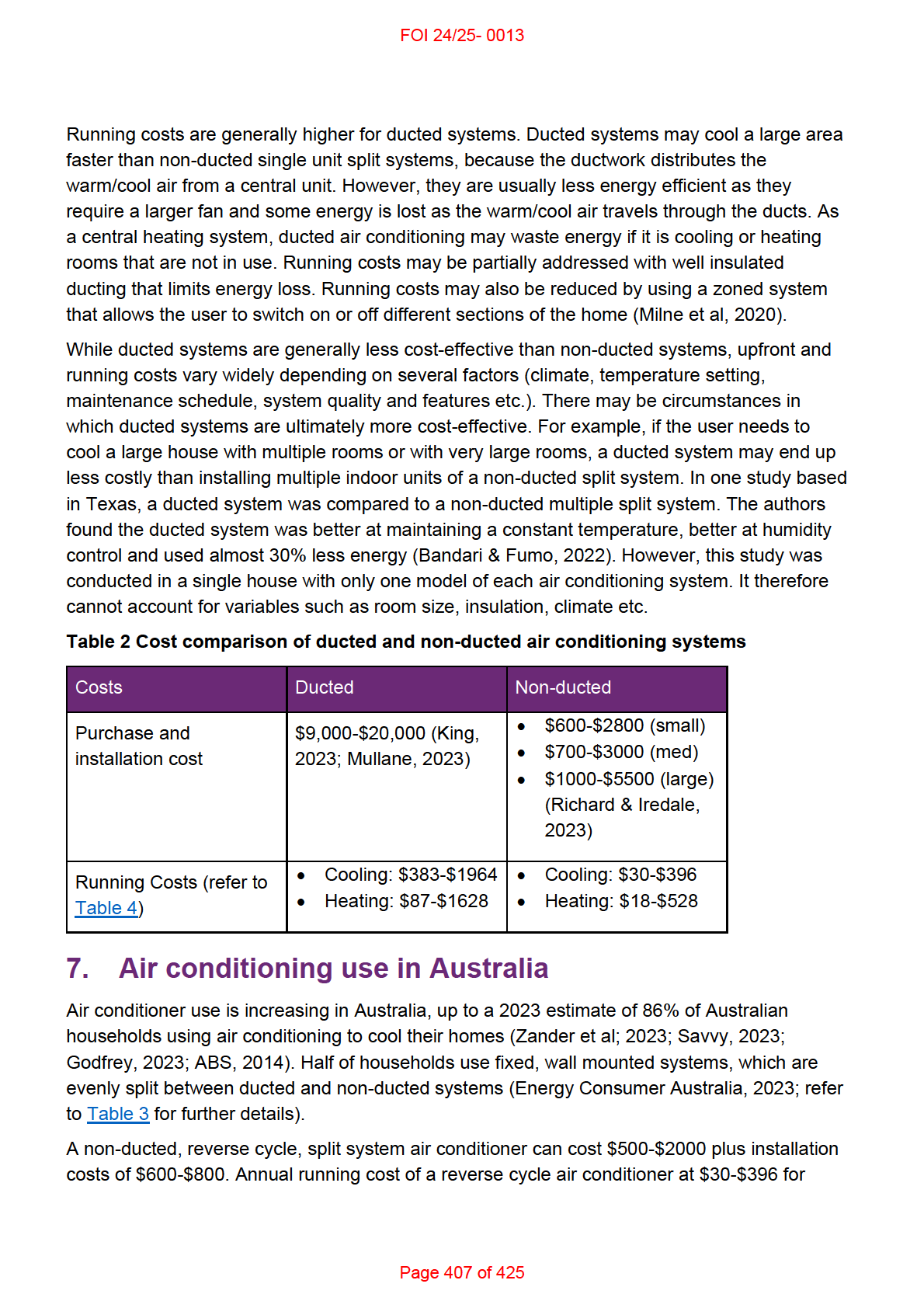
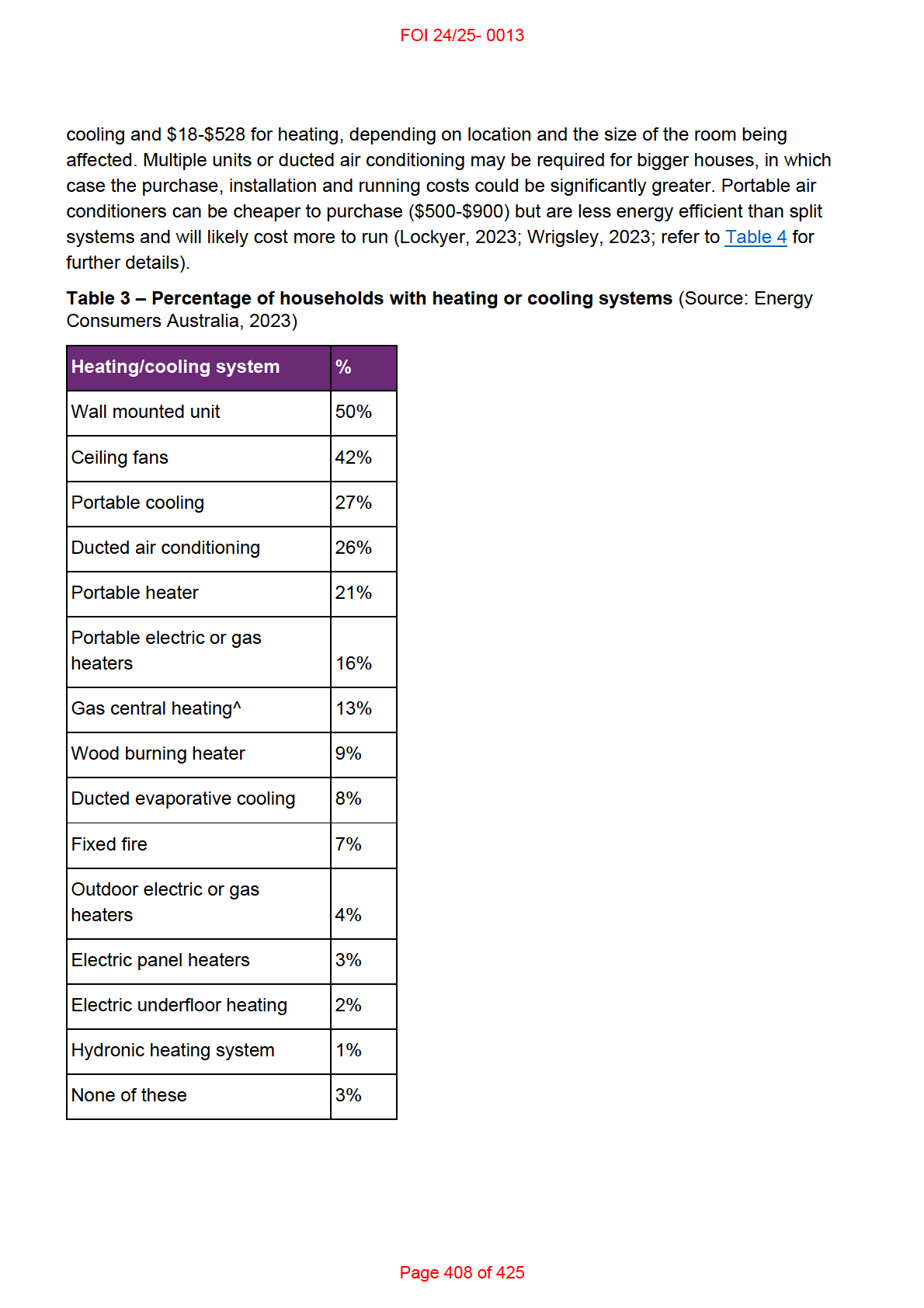
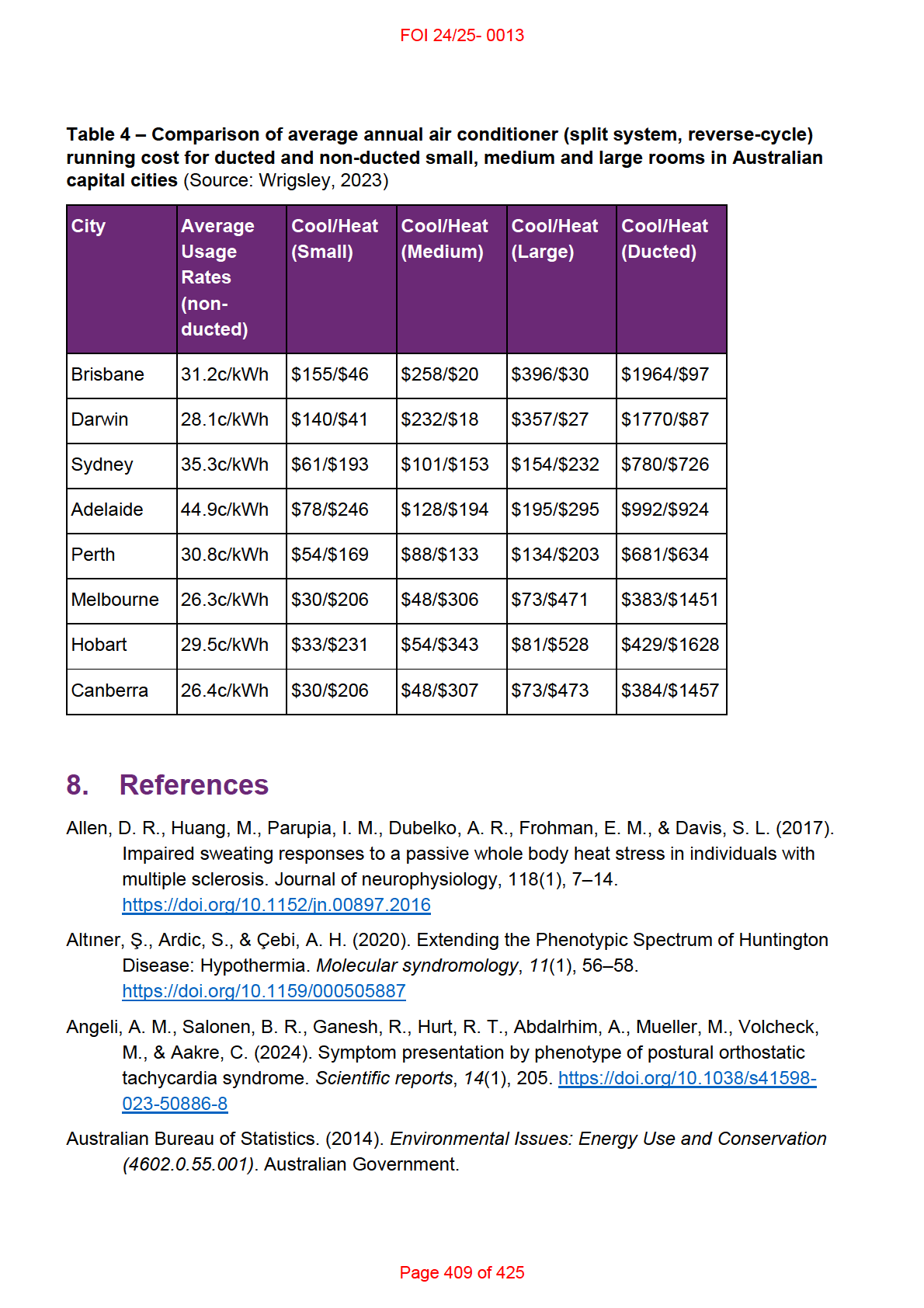
Thyrotoxicosis, Pheochromocytoma
4.1 Spinal cord injury
There is evidence of impaired thermoregulation in people with spinal cord injury, mostly likely
due to a combination of reduced activity of thermoreceptors to detect changes in temperature,
reduced muscle mass and impairment in thermoeffectors such as sweating, vasoconstriction
and vasodilation (Osila et al, 2023; Grossman et al, 2021; Zhang, 2019; Price & Trbovich,
2018; Cheshire, 2016; Girard, 2015). People with higher level of lesion show greater
thermoregulatory impairment (Osila et al, 2023; Grossman et al, 2021). There is evidence that
people with spinal cord injury below the level of T6 can regulate body temperature as
effectively as people without spinal cord injury (Grossman et al, 2021; Price & Trbovich, 2018).
There is some evidence that thermoregulation impairment in people with spinal cord injuries
above T6 may also lead to activity limitations. For example, high or low temperatures may
prevent people with tetraplegia from participating in activities outside the home (Price &
Trbovich, 2018).
4.2 Acquired brain injury
Thermoregulatory impairment after brain injury (traumatic brain injury or stroke) may involve
injury to the hypothalamus, changes in blood flow, vascular control and metabolism, and
difficulties with mobility or judgement (Gowda et al, 2018; Cheshire, 2016; Thompson et al,
2003). There is evidence that around 70% of people experience hyperthermia during the acute
phase after traumatic brain injury. This may be due to the nature of the injury, post-traumatic
inflammation or post-injury infection (Thompson et al, 2003). Hyperthermia is a risk factor for
secondary injury. This includes rebound hyperthermia, which is a possible consequence of
rewarming after induced hypothermia (Gowda et al, 2018; Childs & Lunn, 2013). Clinicians
regularly induce hypothermia soon after the initial brain injury to prevent secondary brain injury
and improve other outcomes. Thermoregulatory impairment may be more common in some
people with brain injury, though affected sub-groups have not been identified (Gowda et al,
2018).
Page 397 of 425
FOI 24/25- 0013
4.3 Parkinson’s Disease
Thermoregulation difficulties are common in people with Parkinson’s disease and may lead to
difficulties with sweating, sleep, and altered perception of heat and cold (Pfeiffer, 2020; Coon
& Low, 2018; Zhong et al, 2013). The presence of peripheral neuropathy in people with
Parkinson’s disease can result in impairments to thermoeffectors such as
vasoconstriction/dilation, sweating and piloerection (Coon & Low, 2018). Around 30-70% of
people with Parkinson’s experience problems with sweating, including hyperhidrosis
(increased sweating) and hypohidrosis (reduced sweating). This may be related to
neurological changes or to medications used to treat the core symptoms of Parkinson’s
disease. Hypohidrosis can increase risk of overheating, while hyperhidrosis can be
uncomfortable and lead to sleep difficulties (Pfeiffer, 2020; Jost, 2017). Thermoregulation
impairment can affect well-being and quality of life for people with Parkinson’s disease:
Patients are often bothered by heat intolerance which may influence activity levels and
social endeavors. Needing to frequently change clothing or bedding due to excessive
sweating episodes is also problematic for patients and their caregivers, particularly
when motor function is compromised. Temperature intolerance or night sweats may
impair a patient’s sleep, which is often affected due to motor dysfunction or concomitant
sleep disorders. Social function is also affected by sweating episodes, leaving some
patients to feel embarrassed and contributing to social isolation (Coon & Law, 2018,
p.271).
4.4 Multiple Sclerosis
Thermoregulation impairment is more researched in multiple sclerosis than for any other
condition. Around 60-80% of people with multiple sclerosis experience temperature sensitivity.
Thermoregulatory dif iculties in people with multiple sclerosis, especially susceptibility to
hyperthermia, may be due to impaired sweating function, decreased sensitivity of
thermoreceptors or hypothalamic dysfunction. Hyperthermia is a significant risk as it can
exacerbate symptoms including muscle weakness, spasticity, fatigue, blurred vision and pain,
as well as worsening existing difficulties with balance, processing speed, concentration, and
attention (Osila et al, 2023; Christogianni et al, 2022; Razi et al, 2022; Davis et al, 2018;
Christogianni et al, 2018; Al en et al, 2017). Hyperthermia may be induced by environmental
increases in temperature, hot baths or exercise (Razi et al, 2022; Christogianni et al, 2022;
Davis et al, 2018; Christogianni et al, 2018). However, there is evidence that regular exercise
for people with multiple sclerosis can improve symptoms and quality of life. Therefore, heat
management strategies should be in place when clinicians recommend an exercise program
for people with multiple sclerosis (Huang et al, 2015). Cold temperatures can also lead to a
worsening of symptoms, though this is less common and less studied (Christogianni et al,
2018).
Page 398 of 425
FOI 24/25- 0013
4.5 Peripheral neuropathy
Peripheral neuropathy is a general term for conditions that cause damage to the nerves of the
peripheral nervous system. Damage can occur to large-diametre or small-diametre nerve
fibres. Large fibres mediate motor and sensory functions, while small fibres mediate autonomic
functions, pain and temperature (Novello & Pobre, 2023; Castelli et al, 2020).
Conditions that can result in peripheral neuropathy include Guil aine-Barre syndrome, diabetes
mellitus, Fabry disease, Parkinson’s disease, Ehlers Danlos syndrome, postural orthostatic
tachycardia syndrome (POTS) and Sjögren syndrome. Diabetes related peripheral neuropathy
is the most prevalent form of the peripheral neuropathy in developed countries (Osila et al,
2023; Fealey, 2018; Cheshire, 2016).
There is evidence that most people with some form of peripheral neuropathy experience
abnormalities in core body temperature. Common thermoregulatory concerns for people with
peripheral neuropathy include impairments to physiological thermoeffectors such as
vasoconstriction/dilation, sweating, piloerection and shivering (Fealey, 2018; Cheshire, 2016).
As peripheral neuropathy is associated with reduced sensitivity of thermoreceptors, there is
also reason to believe the condition may lead to disruption of behavioural thermoeffectors
(Fealey, 2018).
Heat intolerance is a possible symptom of POTS. High ambient temperatures may also
exacerbate core symptom of orthostatic intolerance. (Fedorowski, 2018; Landero, 2014;
Goodkin & Bellew, 2014). These symptoms may be associated with the presence of small fibre
neuropathy. In a study of 276 participants with POTS, Angeli et al (2024) found 35% showed
altered sweat patterns, which characterised the neuropathic phenotype. A small study of 30
people with POTS found significant differences in thermal perception and pain threshold (Bil ig
et al, 2020). POTS is also a common co-occurring condition in Ehlers Danlos syndrome, which
itself can present with thermoregulatory dif iculties (Colman et al, 2023; Thwaites et al, 2022;
Hakim et al, 2017).
4.6 Psychosocial conditions
While there is preliminary evidence that some people with anxiety disorders show
abnormalities in physiological thermoeffectors such as vasodilation and sweating (Fischer et
al, 2021), psychosocial conditions may coincide with thermoregulatory impairments in the form
of altered sensation or disrupted behavioural thermoeffectors (due to altered cognition,
judgement or executive control). RES 319 Weather and Bipolar Disorder contains some
discussion of the effects of temperature on outcomes for people with bipolar and other
psychosocial conditions.
Page 399 of 425
FOI 24/25- 0013
4.7 Epilepsy and seizure disorders
Temperature may affect epilepsy and seizure activity differently, depending on the individual,
the type of epilepsy or type of seizure.
Hyperthermia is both a possible trigger and a possible consequence of seizure. It may be a
consequence of seizure due to excessive muscle activity or activation of the autonomic system
(Pollandt & Bleck, 2018; Cheshire, 2016). Hyperthermia can also cause seizures, as in the
case of febrile seizures experienced mainly by children during episodes of fever. In Dravet
syndrome, seizures can follow even small temperature increases caused by higher ambient
temperatures, fever, cold-warm shifts, warm baths or exercise (Gulcebi et al, 2021; Pollandt &
Bleck, 2018).
However, colder temperatures may also increase risk of seizure in epilepsy. Hospital
admission studies in Taiwan, Germany and Korea found that seizure risk increases in colder
temperatures (Chang et al, 2019; Kim et al, 2017; Rakers et al, 2017). However, these studies
take place in climates that tend to have mild summers and may not generalise to Australia. For
example, Rakers et al (2017) found that ambient temperatures higher than 20°C decrease the
risk of seizure, though the highest recorded temperature in the study was 28°C.
Epilepsy Action Australia (n.d.) states:
Whilst research related to weather and seizures has been limited, and based in the
northern hemisphere, there is no scientific evidence that hot weather itself causes
seizures to occur in people with epilepsy. In Australia it appears most people report that
the heat, or becoming overheated, tends to increase the likelihood of seizures.
Becoming severely overheated can cause seizures, but an average hot day is not in
itself the culprit.
Obviously, heat can be a major contributor to dehydration. If someone is exposed to
heat for a long period of time and does not drink enough fluid, this can cause
dehydration which can increase the risk of a seizure in someone with epilepsy,
sometimes later in the day. When fluid loss from the body (mostly perspiration) is
greater than fluid intake, it causes a change in electrolytes – a drop in sodium (salt) and
glucose (sugar) levels in the body. Ultimately, this can lead to low blood sugar levels
(hypoglycemia) which can also trigger seizures for some people.
4.8 Autism
People with autism may experience sensory differences such as hypo or hypersensitivity to
heat or cold (Raising Children Network, 2024; Zaniboni et al, 2023; Hidaka et al, 2023). Based
on their review, Zaniboni et al suggest the following sensory dif erences with respect to
perception of heat and cold:
Page 400 of 425
FOI 24/25- 0013
• Different tactile sensitivity, as well as higher variability in warm and cold detection:
paradoxical heat sensation (the perception of heat when it should not be perceived,
hyper-sensitivity), lower thresholds in heat and cold detection (hypo-sensitivity).
• Thermal processing might be related with environment adoption or self-injury.
• Difficulties with interoception (heart-rate and body-temperature perception) and self-
regulation and identification of emotions.
• Differences in hypothalamus development (related to homeostasic regulation, including
metabolic rate, temperature and emotion). This can also lead to depression, anxiety,
sleep disorders and obesity (2023, p.10).
4.9 Motor neurone disease / Amyotrophic lateral sclerosis
There is a lack of evidence regarding thermoregulatory impairments in motor neurone
diseases such as amyotrophic lateral sclerosis (ALS). It is likely that behavioural
thermoeffectors are impaired in ALS considering symptoms related to mobility and cognitive
functions. There is minimal evidence that people with ALS experience altered heat sensation
and that hypothalamus volume may be reduced. Physiological thermoeffectors such as
shivering may be affected by progressive impairment in skeletal muscles (Dupuis et al, 2018).
Much of the evidence for involvement of thermoregulatory systems in ALS comes from studies
of animal models (Rodríguez-Sánchez et al, 2022; Braun et al, 2019). In their review of the
subject, Dupuis et al state:
In our clinical experience, we observed that ALS patients often complain of feeling hot,
or conversely of being unable to warm up, and some patients develop low body
temperature. Also, some patients report a worsening of symptoms in cold weather.
However, these symptoms are generally not considered as being part of the core clinical
picture, mostly because they are attributed to muscle atrophy and/or nerve
degeneration. Therefore, potential thermoregulatory defects to the best of our
knowledge have never been systematically studied in ALS patients (2018, p.750).
Since then, at least one study has shown a high rate of hypothermia in people with ALS who
have had tracheostomy or invasive ventilation for longer than five years (Nakayama et al,
2018).
4.10 Huntington’s disease
Thermoregulation problems are sometimes reported by people with Huntington’s disease:
some clinicians do occasionally report anecdotally that some of their [Huntington’s
disease] patients seem to have a striking indifference to cold and that they wil dress too
lightly for the weather, while others wil sweat so profusely that they resort to wearing
cooling vests (Weydt et al, 2018, p.766).
The first case study of a person with Huntington’s disease presenting with hypothermia was
submit ed in 2020 (Altiner et al, 2020). Most of the evidence of thermoregulation impairment in
Page 401 of 425
FOI 24/25- 0013
Huntington’s disease comes from animal models. These studies have shown evidence of
hypothermia, weight loss, involuntary movements, as well as differences in circadian rhythms,
brown adipose tissue, skeletal muscle and the hypothalamus. This suggests a possible effect
of Huntington’s disease on heat retention, shivering and non-shivering thermogenesis.
Development of psychiatric conditions and problems with mobility and cognitive function may
also contribute to disruption of behavioural thermoeffectors. There are few studies directly
investigating thermoregulation associated with Huntington’s disease in humans (Altiner et al,
2020; Weydt et al, 2018).
4.11 Severe burns
The skin plays an important role in thermoregulatory processes including heat retention,
sensation, sweating, piloerection, vasodilation and vasoconstriction. When large parts of the
skin are lost or damaged, this enables increased heat loss and contributes to difficulties
sensing changes in temperature, thereby increasing the risk of hypothermia. People with
severe burns are also at risk of hypermetabolism, which can lead to hyperthermia, excessive
sweating, weight loss, muscle wasting and other symptoms (Radzikowska-Büchner et al,
2023; Mertin et al, 2022). In cases of severe burn injury, metabolic changes can last up to
three years after the initial injury and function of damaged skin may not return (Radzikowska-
Büchner et al, 2023; Jeshke et al, 2011).
5. Management of thermoregulation impairment
Researchers and clinicians have recommended behavioural strategies to manage
thermoregulation impairment in people with multiple sclerosis (Christogianni et al, 2022; Davis
et al, 2018), autism (Zaniboni et al, 2023), and spinal cord injury (Girard, 2015). Behavioural
strategies can include moving to a cooler area, planning activities for cooler times of the day,
taking regular breaks from strenuous activity, choosing weather appropriate clothing, or
gradual acclimatisation in warmer or colder temperatures (Healthdirect, 2024; Zaniboni et al,
2023; Grossman et al, 2021; Davis et al, 2018; Girard, 2015; Australian Red Cross, n.d.).
Standard first line treatment for hyperthermia includes cooling strategies that are usually low
cost or readily accessible: air conditioning, misting fans, cold bath or shower, drinking cold
water and applying cold packs or ice packs (Healthdirect, 2024; Grossman et al, 2021;
Christogianni et al, 2022; Davis et al, 2018; Gowda et al, 2018; Hopkins et al, 2018;
Zawardska et al, 2017; Cheshire, 2016; Australian Red Cross, n.d.). These non-invasive
methods are less easy to control than invasive cooling strategies such as intravenous injection
of cooling substances. Where non-invasive strategies succeed in lowering body temperature,
they are not easily able to maintain a stable target temperature and therefore require
monitoring and adjustment (Gowda et al, 2018).
There is evidence of effectiveness of non-invasive cooling strategies to improve exercise
performance and lower the risk of heat related effects of exercise in the general population
(Heydenreich et al, 2023; Douzi et al, 2019). There is mixed evidence for the effectiveness of
Page 402 of 425
FOI 24/25- 0013
non-invasive strategies in people with thermoregulatory impairment. The inconsistency in the
evidence may be due to the frequency of smal , low powered studies and the heterogeneity of
climatic conditions and outcome measures (Grossman et al, 2021).
In a review of cooling strategies for people with spinal cord injury, Grossman et al (2021) found
inconsistent evidence for the temperature reducing effects of cooling garments, cold drinks
and misting fans. Some studies show cooling garments reduce skin temperature but not core
body temperature, whereas a consistent effect across several studies showed pre-cooling
using cooling garments or other methods could improve endurance during exercise and lower
rate of increase of body temperature (Grossman et al, 2021; Davis et al, 2018).
A 2023 systematic review into the use of cooling garments for people with Multiple Sclerosis
found that cooling garments are effective in reducing body temperature and improving walking
capacity and functional mobility (Stevens et al, 2023). The authors found no significant
differences between types of cooling garment. Active treatment groups were compared with
either other cooling garments, sham active controls or passive controls. No study was
reviewed that compared cooling garments with other cooling strategies such as air
conditioning.
5.1 Air conditioning compared to other cooling strategies
Researchers and clinicians have recommended reducing the ambient temperature of the
environment with space cooling strategies/devices as a way of managing thermoregulation
impairment in people with multiple sclerosis (Christogianni et al, 2022; Davis et al, 2018),
autism (Zaniboni et al, 2023), spinal cord injury (Price & Trbovich, 2018), epilepsy (Epilepsy
Action Australia, n.d.), and severe burns (Radzikowska-Büchner et al, 2023).
Existing evidence indicates that air conditioning has a role in managing thermoregulation
impairment. Hospital studies show air conditioning can improve or maintain patients’ thermal
comfort, recovery rates and well-being, and reduce infections and length of hospital stays.
However, more research is required to determine the optimum ambient temperature to
maximise patient outcomes (Lenzer et al, 2020; Shajahan et al, 2019). In the case of severe
burns, raising the ambient temperature of the room to 24°C – 38°C may prevent or reduce the
risk of a hypermetabolic reaction (Radzikowska-Büchner et al, 2023).
There are very few studies in which air conditioning is assessed as an intervention aimed to
manage thermoregulation impairment. In a survey study of 438 heat-sensitive people with
multiple sclerosis, Christogianni et al (2022) found that around three quarters used air
conditioning to manage risks of overheating. However, in a review of cooling
therapies/interventions for people with multiple sclerosis, Bilgin et al (2022) did not find any
studies that used any conditioning as an intervention.
No studies were found comparing the use of air conditioning with other cooling methods in
il ness management or treatment. One study compared the use of air conditioning with electric
fans in the general population (Morris et al, 2021). The authors found that electric fans are an
Page 403 of 425
FOI 24/25- 0013
appropriate way to manage risk of heat stress for adults in Australia when the ambient
temperature is under 38°C. However, the authors also examined older people taking
medication that may impair sweating function. They found impaired sweating function lowers
the effectiveness of electric fans. This is because fans cool by both convection and
evaporation (refer to 6.2 Fans for more detail). Therefore, the authors recommend
supplementing electric fan use with air conditioning systems for people with impaired sweating
function.
Most recommendations cited above are based on clinical opinion. Furthermore, the
recommendations focus on achieving or maintaining cool indoor air temperatures, and rarely
mention the means to achieve those temperatures. They do not differentiate between air
conditioning and other space cooling strategies (evaporative cooling, ceiling fans, passive
cooling).
6. Air conditioning and other cooling systems
Common home cooling systems include fans, evaporative cooling or refrigerated cooling.
Sometimes the term air conditioning is used to refer to all these systems. Most often it is used
to refer only to refrigerated cooling systems.
Not all systems wil be appropriate in all circumstances. The most appropriate air conditioning
system for a person wil depend on factors including:
• environment – regional climate, average temperature, humidity
• building – size, layout, solar power, air flow and other passive cooling features
• occupancy – whole house or single room, rent or own, number of residents
• lifestyle – budget, habits, cooling needs, sustainability preferences (Wrigsley, 2023;
Barnes, 2023; Lockyer, 2023; Milne et al, 2020; Gilmour & Steen, n.d.).
6.1 Cooling garments
Cooling garments can include jackets, vests, hats, hoods, gloves, wrist bands and thigh straps
(Stevens et al. 2023; Laique & Hussain, 2018). Ren et al (2022) identify six types of cooling
mechanism used in garments:
• ice cooling – garment contains insulated pockets to hold ice
• phase change materials cooling – made from a designed material that uses the latent
heat from the body to lower the temperature of the microclimate between the body and
the garment
• radiative cooling – made from a designed material that aims to maximise heat loss
allowing more infrared radiation to escape the body
• thermo-electric cooling – garment contains conductors which can be used to directly
draw heat energy from the body as an electric current is passed through the conductor
• liquid cooling – garment contains pipes carrying cold liquid and a pump to ensure liquid
is spread over the garment
Page 404 of 425
FOI 24/25- 0013
• air-cooling – garment that maximises ventilation through the use of design and small
electric fans.
6.2 Fans
Fans work by moving air around a room more quickly. They do not cool the air, but rather aid
the body’s thermoregulatory processes. Faster moving air helps sweat evaporate more quickly
(evaporation) and blows cooler air at the skin (convection). Fans are less effective in higher
temperatures, though the exact threshold is stil being debated in the literature (Morris et al,
2021; Milne et al, 2020; Iorio, 2019). Fans can be effective for healthy adults in temperatures
up to 38°C (Morris et al, 2021) and may help to a lesser extent up to 42°C (Iorio, 2019). The
Australian government’s Your Home site states:
Fans should be the first appliance of choice for cooling. They are cheap to run and
generally use less energy than evaporative coolers or air-conditioners. Typically, the air
flow created by a fan provides a similar improvement to comfort as reducing the
temperature by around 3°C. With good design and insulation, fans can often supply
adequate cooling for acclimatised residents in all Australian climates (Department of
Climate Change, Energy, the Environment and Water; n.d).
Fans are most effective when aimed directly toward the body, in humid climates or when used
in combination with water spray, wet clothing or wraps (Morris et al, 2021; Milne et al, 2020;
Iorio, 2019; Department of Climate Change, Energy, the Environment and Water; n.d.).
6.3 Evaporative cooling
An evaporative cooler blows cool, humid air into a space by drawing outside air through a wet
filter which is then expelled by a fan. An evaporative cooler may be less expensive to purchase
and run than an air conditioning system, but this depends on the model. Evaporative coolers
are less effective in humid environments and require large amount of water to operate (Milne
et al, 2020; Department of Climate Change, Energy, the Environment and Water; n.d.).
6.4 Air conditioning (refrigerated cooling)
An air conditioning system that operates by refrigerated cooling draws warm air from inside the
space and cools it via contact with a refrigerant gas. The cool air is blown back into the space
and the extracted heat is expelled outside (Barnes, 2023; Milne et al, 2020; Barnes, 2019;
Department of Climate Change, Energy, the Environment and Water; n.d.). Air conditioning
systems can vary by cost, size, energy efficiency and type of refrigerant used. Air conditioners
can be:
• fixed or portable
• single unit, split system, or multi-split system
• ducted or non-ducted
Page 405 of 425
FOI 24/25- 0013
• reverse cycle or cooling only (Wrigsley, 2023; Barnes, 2023; Department of Climate
Change, Energy, the Environment and Water, n.d.; Milne et al, 2020).
For comparison of purchase and running costs of different air conditioning systems in
Australia, refer to 7. Air conditioning in Australia.
Reverse cycle air conditioning
A reverse cycle air conditioner operates in a similar way to a cooling-only system. However, a
reverse cycle system is also able to reverse the refrigeration process, sending cold air outside
and warm air inside. Reverse cycle air conditioners are often considered the most efficient
systems because they can provide both heating and cooling. However, energy efficiency
ultimately depends on a range of factors (Department of Climate Change, Energy, the
Environment and Water, n.d.; Milne et al, 2020; Barnes, 2019).
Single unit, split system, or multi-split system air conditioning
Split system air conditioners have an outside unit and an inside unit. They are the most
common fixed air conditioning systems and are usually more energy efficient than single unit
systems. Split systems can be ducted or non-ducted. Multi-split systems have an outside unit
and multiple indoor units, which can be placed in dif erent rooms. They are an alternative to
ducted systems (Barnes, 2023; Department of Climate Change, Energy, the Environment and
Water, n.d.; Milne et al, 2020; Barnes, 2019).
Single unit systems are generally suited to smaller areas. They are generally less energy
efficient than split systems. They can be fixed or portable. Portable systems are generally less
expensive to purchase than fixed systems. They may be appropriate for smaller areas or when
the system needs to be moved to different areas. They may also be appropriate when
installing a fixed unit is not feasible, such as in rental properties (Lockyer, 2023; Milne et al,
2020; Barnes, 2019).
Ducted air conditioning
A ducted system is a central heating or cooling system, which means it is designed to warm or
cool a whole house or building rather than a single room. Ducted systems can be evaporative
coolers, reverse-cycle split systems or cooling only split systems. There is usually an outdoor
unit on the roof and an indoor unit under the floor or in the ceiling. Ducts extend from the
indoor unit and into multiple rooms or multiple areas of a bigger space (Department of Climate
Change, Energy, the Environment and Water, n.d.; Milne et al, 2020; Barnes, 2019).
In terms of cost, ducted systems are generally more expensive to purchase, install and run,
and therefore are generally less cost effective than non-ducted systems (refer to Table 2).
Installation is a significant upfront cost for ducted systems as work is required to install the roof
unit as well as ducts throughout the home. Furthermore, ducted systems are not possible in
some houses due to lack of space or other architectural features (King, 2023; Mullane, 2023).
Page 406 of 425
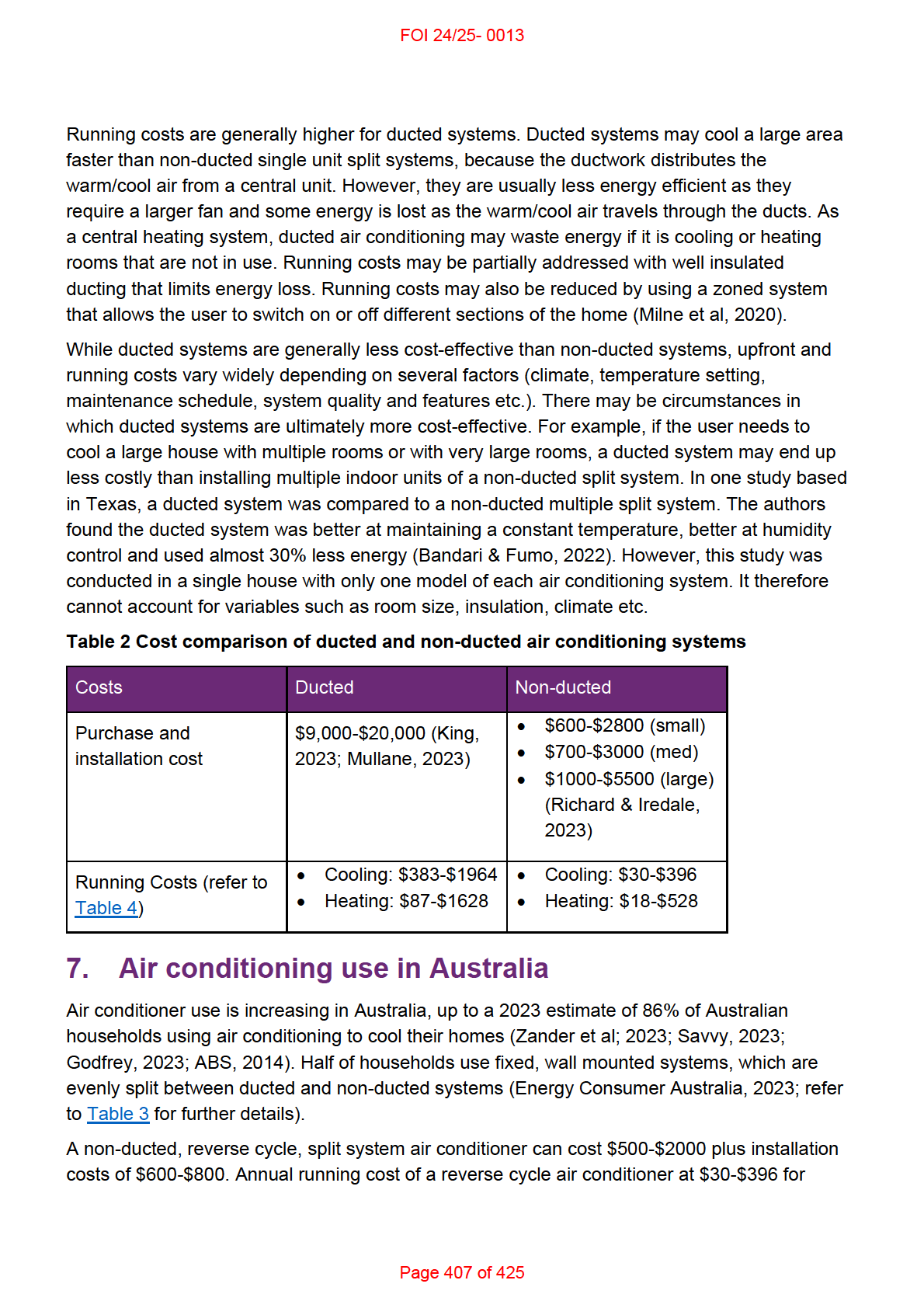
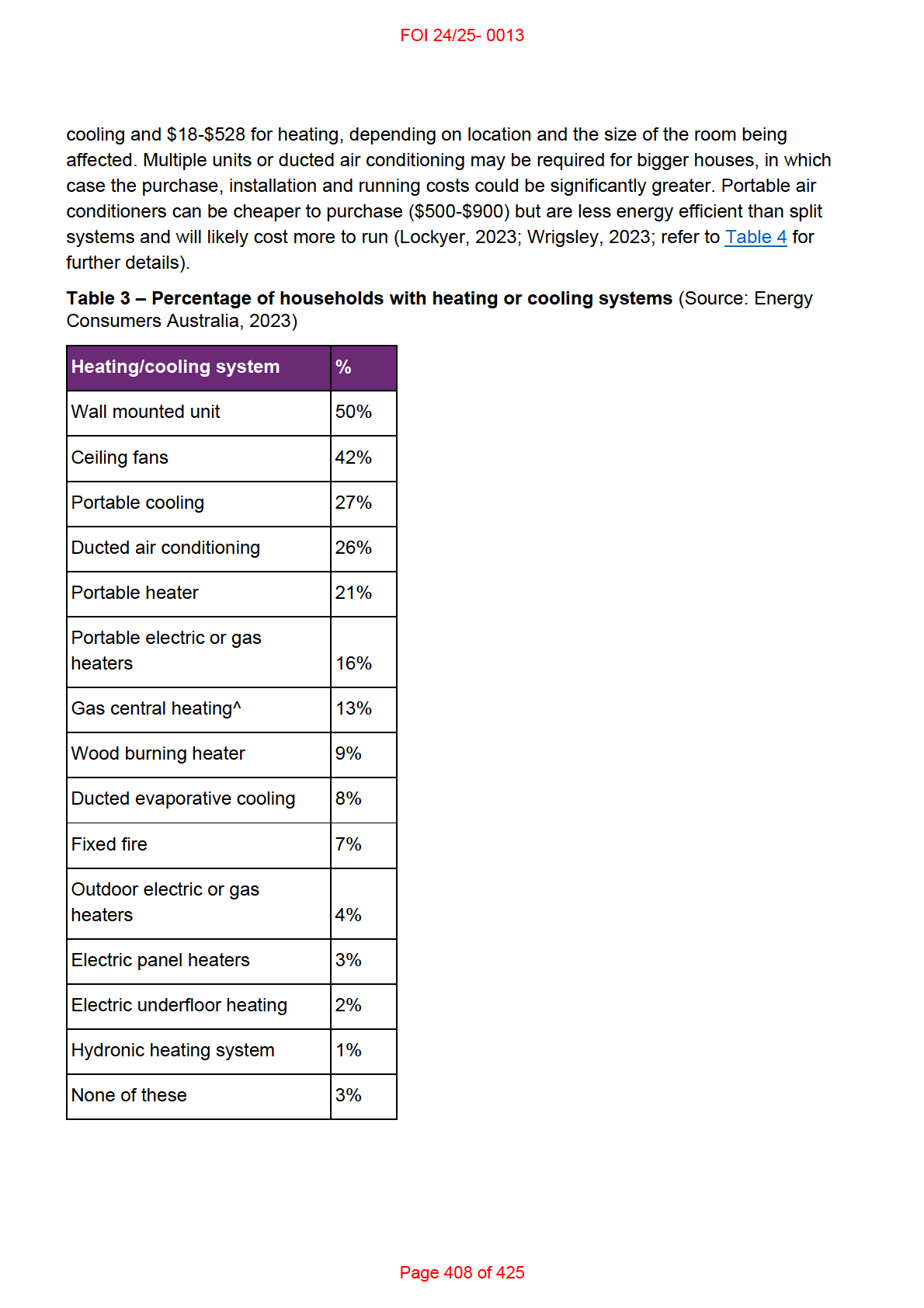
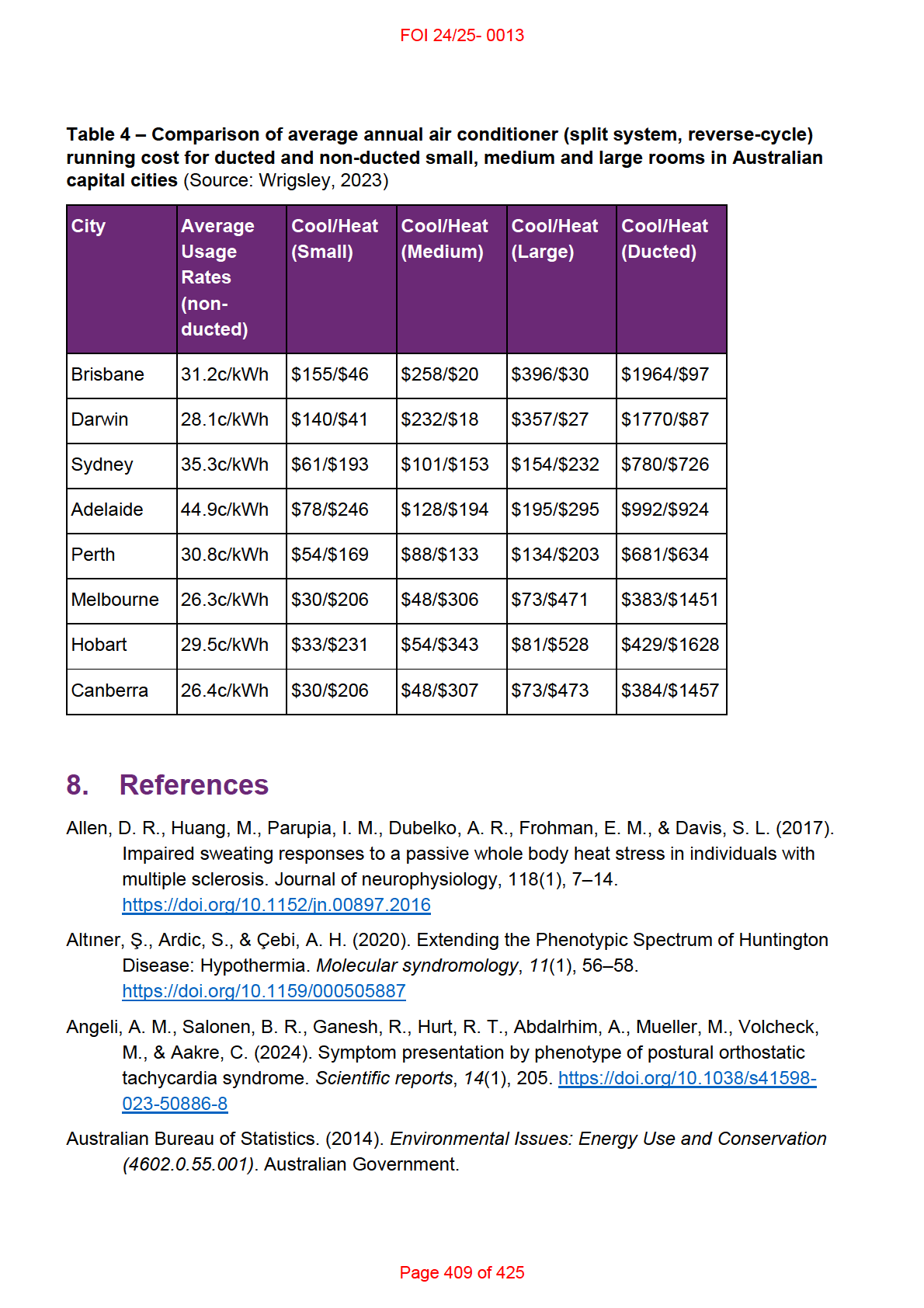
FOI 24/25- 0013
https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4602.0.55.001Mar%202014
?OpenDocument
Australian Red Cross. (n.d.).
Heatstroke and heat exhaustion.
https://www.redcross.org.au/emergencies/prepare/heatstroke-and-heat-exhaustion/
Barnes, C. (2023).
What to know before buying an air conditioner. CHOICE.
https://www.choice.com.au/home-and-living/cooling/air-conditioners/buying-guides/air-
conditioners
Barnes, C. (2019).
How to buy ducted reverse-cycle air conditioning. CHOICE.
https://www.choice.com.au/home-and-living/cooling/ducted-reverse-cycle-air-
conditioning/buying-guides/ducted-reverse-cycle-air-conditioning
Bennetts, H., Arakawa Martins, L., van Hoof, J., & Soebarto, V. (2020). Thermal Personalities
of Older People in South Australia: A Personas-Based Approach to Develop Thermal
Comfort Guidelines. International journal of environmental research and public health,
17(22), 8402. https://doi.org/10.3390/ijerph17228402
Bhandari, M. & Fumo, N. (2022). Comparison Study of a Traditional Ducted Heat Pump and a
Multi Split Heat Pump.
International Refrigeration and Air Conditioning Conference.
Paper 2321. https://docs.lib.purdue.edu/iracc/2321
Bil ig, S. C. I., Schauermann, J. C., Rolke, R., Katona, I., Schulz, J. B., & Maier, A. (2020).
Quantitative sensory testing predicts histological small fiber neuropathy in postural
tachycardia syndrome.
Neurology, Clinical practice,
10(5), 428–434.
https://doi.org/10.1212/CPJ.0000000000000770
Braun, M. C., Castillo-Ruiz, A., Indic, P., Jung, D. Y., Kim, J. K., Brown, R. H., Jr, Swoap, S. J.,
& Schwartz, W. J. (2019). Defective daily temperature regulation in a mouse model of
amyotrophic lateral sclerosis.
Experimental neurology, 311, 305–312.
https://doi.org/10.1016/j.expneurol.2018.07.008
Castelli, G., Desai, K. M., & Cantone, R. E. (2020). Peripheral Neuropathy: Evaluation and
Differential Diagnosis.
American family physician, 102(12), 732–739.
Chang, K. C., Wu, T. H., Fann, J. C. Y., Chen, S. L. S., Yen, A. M. F., Chiu, S. Y. H., ... & Liou,
H. H. (2019). Low ambient temperature as the only meteorological risk factor of seizure
occurrence: A multivariate study.
Epilepsy & Behavior, 100, 106283.
Cheshire W. P., Jr (2016). Thermoregulatory disorders and il ness related to heat and cold
stress.
Autonomic neuroscience: basic & clinical, 196, 91–104.
https://doi.org/10.1016/j.autneu.2016.01.001
Childs, C., & Lunn, K. W. (2013). Clinical review: brain-body temperature differences in adults
with severe traumatic brain injury.
Critical Care, 17, 1-17.
Christogianni, A., O'Garro, J., Bibb, R., Filtness, A., & Filingeri, D. (2022). Heat and cold
sensitivity in multiple sclerosis: A patient-centred perspective on triggers, symptoms,
Page 410 of 425
FOI 24/25- 0013
and thermal resilience practices.
Multiple sclerosis and related disorders, 67, 104075.
https://doi.org/10.1016/j.msard.2022.104075
Christogianni, A., Bibb, R., Davis, S. L., Jay, O., Barnett, M., Evangelou, N., & Filingeri, D.
(2018). Temperature sensitivity in multiple sclerosis: An overview of its impact on
sensory and cognitive symptoms. Temperature (Austin, Tex.), 5(3), 208–223.
https://doi.org/10.1080/23328940.2018.1475831
Colman, M., Syx, D., De Wandele, I., Rombaut, L., Wil e, D., Malfait, Z., ... & Malfait, F. (2023).
Sensory profiling in classical Ehlers-Danlos syndrome: a case-control study revealing
pain characteristics, somatosensory changes, and impaired pain modulation. The
Journal of Pain, 24(11), 2063-2078 https://doi.org/10.1016/j.jpain.2023.06.015
Connor, N. (2022).
What is Radiation Heat Transfer – Definition. thermal-engineering.org.
https://www.thermal-engineering.org/what-is-radiation-heat-transfer-definition/
Coon, E. A., & Low, P. A. (2018). Thermoregulation in Parkinson disease.
Handbook of clinical
neurology, 157, 715–725. https://doi.org/10.1016/B978-0-444-64074-1.00043-4
Davis, S. L., Jay, O., & Wilson, T. E. (2018). Thermoregulatory dysfunction in multiple
sclerosis. Handbook of clinical neurology, 157, 701–714. https://doi.org/10.1016/B978-
0-444-64074-1.00042-2
Department of Climate Change, Energy, the Environment and Water. (n.d.).
Heating and
cooling. Australian Government. https://www.energy.gov.au/households/heating-and-
cooling
Douzi, W., Dugué, B., Vinches, L., Al Sayed, C., Hallé, S., Bosquet, L., & Dupuy, O. (2019).
Cooling during exercise enhances performances, but the cooled body areas matter: A
systematic review with meta-analyses.
Scandinavian journal of medicine & science in
sports,
29(11), 1660–1676. https://doi.org/10.1111/sms.13521
Dupuis, L., Petersen, Å., & Weydt, P. (2018). Thermoregulation in amyotrophic lateral
sclerosis.
Handbook of clinical neurology, 157, 749–760. https://doi.org/10.1016/B978-
0-444-64074-1.00046-X
Energy Consumers Australia. (2023).
Energy Consumer Behaviour Survey.
https://ecss.energyconsumersaustralia.com.au/wp-content/uploads/2023/10/ECBS-
October-2023-Household-Toplines.pdf
Epilepsy Action Australia. (n.d.).
E-360 Edition 20: Weather conditions & epilepsy.
https://www.epilepsy.org.au/e-360-edition-20-weather-conditions-epilepsy/
Fealey R. D. (2018). Thermoregulation in neuropathies.
Handbook of clinical neurology, 157,
777–787. https://doi.org/10.1016/B978-0-444-64074-1.00048-3
Fischer, S., Haas, F., & Strahler, J. (2021). A Systematic Review of Thermosensation and
Thermoregulation in Anxiety Disorders.
Frontiers in physiology, 12, 784943.
https://doi.org/10.3389/fphys.2021.784943
Page 411 of 425
FOI 24/25- 0013
Gilmour, K., & Steen, M. (n.d.).
Portable air conditioner buying guide. CHOICE.
https://www.choice.com.au/home-and-living/cooling/portable-air-conditioners/buying-
guides/portable-air-conditioners
Girard O. (2015). Thermoregulation in wheelchair tennis-How to manage heat stress?.
Frontiers in physiology, 6, 175. https:/ doi.org/10.3389/fphys.2015.00175
Godfrey, J. (2023).
Air conditioning usage statistics 2023-2024. Finder.
https://www.finder.com.au/energy/aircon-statistics
Goodkin, M. B., & Bellew, L. J. (2014). Osteopathic manipulative treatment for postural
orthostatic tachycardia syndrome.
The Journal of the American Osteopathic
Association,
114(11), 874–877. https:/ doi.org/10.7556/jaoa.2014.173
Gowda, R., Jaffa, M., & Badjatia, N. (2018). Thermoregulation in brain injury.
Handbook of
clinical neurology, 157, 789–797. https://doi.org/10.1016/B978-0-444-64074-1.00049-5
Grossmann, F., Flueck, J. L., Perret, C., Meeusen, R., & Roelands, B. (2021). The
Thermoregulatory and Thermal Responses of Individuals With a Spinal Cord Injury
During Exercise, Acclimation and by Using Cooling Strategies-A Systematic Review.
Frontiers in physiology, 12, 636997. https://doi.org/10.3389/fphys.2021.636997
Gulcebi, M. I., Bartolini, E., Lee, O., Lisgaras, C. P., Onat, F., Mifsud, J., Striano, P., Vezzani,
A., Hildebrand, M. S., Jimenez-Jimenez, D., Junck, L., Lewis-Smith, D., Scheffer, I. E.,
Thijs, R. D., Zuberi, S. M., Blenkinsop, S., Fowler, H. J., Foley, A., Epilepsy Climate
Change Consortium, & Sisodiya, S. M. (2021). Climate change and epilepsy: Insights
from clinical and basic science studies.
Epilepsy & behavior, 116, 107791.
https://doi.org/10.1016/j.yebeh.2021.107791
Hakim, A., O'Cal aghan, C., De Wandele, I., Stiles, L., Pocinki, A., & Rowe, P. (2017).
Cardiovascular autonomic dysfunction in Ehlers–Danlos syndrome—hypermobile type.
American Journal of Medical Genetics Part C: Seminars in Medical Genetics,
175(1)
168-174 https://doi.org/10.1002/ajmg.c.31543
Healthdirect. (2024).
How to take care of yourself in a heatwave. Australian Government.
https://www.healthdirect.gov.au/blog/how-to-handle-the-heatwave
Heydenreich, J., Koehler, K., Braun, H., Grosshauser, M., Heseker, H., Koenig, D., Lampen,
A., Mosler, S., Niess, A., Schek, A., & Carlsohn, A. (2023). Effects of internal cooling on
physical performance, physiological and perceptional parameters when exercising in
the heat: A systematic review with meta-analyses.
Frontiers in physiology, 14, 1125969.
https://doi.org/10.3389/fphys.2023.1125969
Hidaka, S., Gotoh, M., Yamamoto, S., & Wada, M. (2023). Exploring relationships between
autistic traits and body temperature, circadian rhythms, and age.
Scientific reports,
13(1), 5888. https://doi.org/10.1038/s41598-023-32449-z
Page 412 of 425
FOI 24/25- 0013
Hopkins, P., Gupta, P. K., & Bilmen, J. G. (2018).
Malignant hyperthermia.
Handbook of
clinical neurology, 157, 645–661. https://doi.org/10.1016/B978-0-444-64074-1.00038-0
Huang, M., Jay, O., & Davis, S. L. (2015). Autonomic dysfunction in multiple sclerosis:
implications for exercise. Autonomic neuroscience: basic & clinical, 188, 82–85.
https://doi.org/10.1016/j.autneu.2014.10.017
Iorio, K. (2019).
Do fans make any difference in a heatwave? ABC News.
https://www.abc.net.au/news/2019-12-20/are-fans-completely-useless-in-a-
heatwave3f/11808944
Jeschke, M. G., Gauglitz, G. G., Kulp, G. A., Finnerty, C. C., Wil iams, F. N., Kraft, R., Suman,
O. E., Mlcak, R. P., & Herndon, D. N. (2011). Long-term persistance of the
pathophysiologic response to severe burn injury.
PloS one,
6(7), e21245.
https://doi.org/10.1371/journal.pone.0021245
Jost W. H. (2017). Autonomic Dysfunction in Parkinson's Disease: Cardiovascular Symptoms,
Thermoregulation, and Urogenital Symptoms.
International review of neurobiology, 134,
771–785. https://doi.org/10.1016/bs.irn.2017.04.003
Kim, S. H., Kim, J. S., Jin, M. H., & Lee, J. H. (2017). The effects of weather on pediatric
seizure: a single-center retrospective study (2005–2015).
Science of the total
environment, 609, 535-540.
King, K. (2023).
Ducted Air Conditioning vs Split System. Canstar Blue.
https://www.canstarblue.com.au/appliances/ducted-vs-split-system-air-con-the-pros-
and-cons/
Laique, M. B., & Hussain, T. (2018). Comparison Between Traditional Air Conditioning System
and Wearable Cooling/Heating Devices.
International Journal of Engineering Research
and Technology,
7(1), 111-113.
Landero J. (2014). Postural orthostatic tachycardia syndrome: a dermatologic perspective and
successful treatment with losartan.
The Journal of clinical and aesthetic dermatology,
7(8), 41–47 https:/ www.ncbi.nlm.nih.gov/pmc/articles/PMC4142820
Lenzer, B., Rupprecht, M., Hoffmann, C., Hoffmann, P., & Liebers, U. (2020). Health effects of
heating, ventilation and air conditioning on hospital patients: a scoping review.
BMC
public health,
20(1), 1287. https://doi.org/10.1186/s12889-020-09358-1
Lockyer, K. (2023).
Portable Air Conditioner vs Split System. Canstar Blue.
https://www.canstarblue.com.au/appliances/portable-or-split-system-air-conditioning-
the-pros-and-cons/
Lohner, S. (2017).
Chil ing Science: Evaporative Cooling with Liquids. Scientific American.
https://www.scientificamerican.com/article/chilling-science-evaporative-cooling-with-
liquids/
Page 413 of 425
FOI 24/25- 0013
Milne, G., Reardon, C., Ryan, P., Pavia, M., & Wyndham, J. (2020).
Heating and cooling. Your
Home: Australian Government. https://www.yourhome.gov.au/energy/heating-and-
cooling
Morris, N. B., Chaseling, G. K., English, T., Gruss, F., Maideen, M. F. B., Capon, A., & Jay, O.
(2021). Electric fan use for cooling during hot weather: a biophysical modelling study.
The Lancet Planetary Health, 5(6), e368-e377. https:/ doi.org/10.1016/S2542-
5196(21)00136-4
Mullane, J. (2023).
How Much Does Ducted Air Conditioning Cost? Canstar Blue.
https://www.canstarblue.com.au/appliances/ducted-air-conditioning-cost
Nakayama, Y., Shimizu, T., Matsuda, C., Haraguchi, M., Hayashi, K., Mochizuki, Y., Nagao,
M., Kawata, A., & Isozaki, E. (2018). Non-motor manifestations in ALS patients with
tracheostomy and invasive ventilation.
Muscle & nerve,
57(5), 735–741.
https://doi.org/10.1002/mus.26004
Novello, B. J., & Pobre, T. (2023). Electrodiagnostic Evaluation of Peripheral Neuropathy. In
StatPearls. StatPearls Publishing.
Osil a, E. V., Marsidi, J. L., Shumway, K. R., & Sharma, S. (2023).
Physiology, Temperature
Regulation. In StatPearls. StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK507838/
Pfeiffer R. F. (2020). Autonomic Dysfunction in Parkinson's Disease. Neurotherapeutics : the
journal of the American Society for Experimental NeuroTherapeutics, 17(4), 1464–1479.
https://doi.org/10.1007/s13311-020-00897-4
Pollandt, S., & Bleck, T. P. (2018). Thermoregulation in epilepsy. Handbook of clinical
neurology, 157, 737–747. https://doi.org/10.1016/B978-0-444-64074-1.00045-8
Price, M. J., & Trbovich, M. (2018). Thermoregulation following spinal cord injury.
Handbook of
clinical neurology, 157, 799–820. https://doi.org/10.1016/B978-0-444-64074-1.00050-1
Raising Children Network. (2024). Sensory sensitivities & autism: 4-18 years.
https://raisingchildren.net.au/autism/behaviour/understanding-behaviour/sensory-
sensitivities-asd
Rakers, F., Walther, M., Schiffner, R., Rupprecht, S., Rasche, M., Kockler, M., ... & Schwab,
M. (2017). Weather as a risk factor for epileptic seizures: a case‐crossover study.
Epilepsia,
58(7), 1287-1295.
Razi, O., Tartibian, B., Teixeira, A. M., Zamani, N., Govindasamy, K., Suzuki, K., Laher, I., &
Zouhal, H. (2022). Thermal dysregulation in patients with multiple sclerosis during
SARS-CoV-2 infection. The potential therapeutic role of exercise.
Multiple sclerosis and
related disorders, 59, 103557. https://doi.org/10.1016/j.msard.2022.103557
Ren, S., Han, M., & Fang, J. (2022). Personal Cooling Garments: A Review.
Polymers,
14(24),
5522. https://doi.org/10.3390/polym14245522
Page 414 of 425
FOI 24/25- 0013
Richard, A., & Iredale, A. (2023).
What size air conditioner do you need? CHOICE
https://www.choice.com.au/home-and-living/cooling/air-conditioners/articles/what-size-
air-conditioner-do-i-need
Rodríguez-Sánchez, S., Valiente, N., Seseña, S., Cabrera-Pinto, M., Rodríguez, A., Aranda,
A., Palop, L., & Fernández-Martos, C. M. (2022). Ozone modified hypothalamic
signaling enhancing thermogenesis in the TDP-43A315T transgenic model of
Amyotrophic Lateral Sclerosis.
Scientific reports,
12(1), 20814.
https://doi.org/10.1038/s41598-022-25033-4
Romanovsky, A. A. (2018).
Thermoregulation Part I: From basic neuroscience to clinical
neurology. Elsevier.
Savvy. (2023). Air Conditioning Use in Australia. https://www.savvy.com.au/energy/air-
conditioning-use-in-australia
Shajahan, A., Culp, C. H., & Wil iamson, B. (2019). Effects of indoor environmental parameters
related to building heating, ventilation, and air conditioning systems on patients' medical
outcomes: A review of scientific research on hospital buildings.
Indoor air,
29(2), 161–
176. https://doi.org/10.1111/ina.12531
Stevens, C. J., Singh, G., Peterson, B., Vargas, N. T., & Périard, J. D. (2023). The effect of
cooling garments to improve physical function in people with multiple sclerosis: A
systematic review and meta-analysis.
Multiple sclerosis and related disorders, 78,
104912. https:/ doi.org/10.1016/j.msard.2023.104912
Strengers, Y., Dahlgren, K., Nichol s, L., Pink, S., Martin, R. (2021).
Digital Energy Futures:
Future Home Life. Emerging Technologies Research Lab (Monash University).
Melbourne, Australia.
https://www.monash.edu/ data/assets/pdf file/0011/2617157/DEF-Future-Home-Life-
Full-Report.pdf
Thompson, H. J., Tkacs, N. C., Saatman, K. E., Raghupathi, R., & McIntosh, T. K. (2003).
Hyperthermia following traumatic brain injury: a critical evaluation.
Neurobiology of
disease,
12(3), 163-173.
Thwaites, P. A., Gibson, P. R., & Burgell, R. E. (2022). Hypermobile Ehlers-Danlos syndrome
and disorders of the gastrointestinal tract: What the gastroenterologist needs to know.
Journal of gastroenterology and hepatology,
37(9), 1693–1709.
https://doi.org/10.1111/jgh.15927
Weydt, P., Dupuis, L., & Petersen, Å. (2018). Thermoregulatory disorders in Huntington
disease.
Handbook of clinical neurology, 157, 761–775. https://doi.org/10.1016/B978-0-
444-64074-1.00047-1
Wrigsley, K. (2023).
How much electricity does an air conditioner use? Canstar Blue.
https://www.canstarblue.com.au/appliances/how-much-electricity-does-aircon-use/
Page 415 of 425
FOI 24/25- 0013
Zander, K. K., Mathew, S., & Carter, S. (2024). Behavioural (mal) adaptation to extreme heat
in Australia: Implications for health and wellbeing.
Urban Climate, 53, 101772.
https://doi.org/10.1016/j.uclim.2023.101772
Zander, K. K., van Hoof, J., Carter, S., & Garnett, S. T. (2023). Living comfortably with heat in
Australia–preferred indoor temperatures and climate zones.
Sustainable Cities and
Society, 104706. https://doi.org/10.1016/j.scs.2023.104706
Zaniboni, L., & Toftum, J. (2023). Indoor environment perception of people with autism
spectrum condition: a scoping review.
Building and Environment, 110545.
Zawadzka, M., Szmuda, M., & Mazurkiewicz-Bełdzińska, M. (2017). Thermoregulation
disorders of central origin - how to diagnose and treat.
Anaesthesiology intensive
therapy,
49(3), 227–234. https:/ doi.org/10.5603/AIT.2017.0042
Zhang Y. (2019). Thermoregulation following Spinal Cord Injury: Theory and Fact.
Medicine
and science in sports and exercise,
51(11), 2425.
https://doi.org/10.1249/MSS.0000000000002086
Zhong, G., Bolitho, S., Grunstein, R., Naismith, S. L., & Lewis, S. J. (2013). The relationship
between thermoregulation and REM sleep behaviour disorder in Parkinson's disease.
PloS one,
8(8), e72661. https:/ doi.org/10.1371/journal.pone.0072661
Page 416 of 425
FOI 24/25- 0013
DOCUMENT 37
Support workers administering medication in
Australia
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research question: What Federal, State and Territory regulations apply to administration of medication by
disability support workers?
Are there additional rules for disability support workers providing high intensity support?
Date: 30/5/24
Requestor: Theresa s22(1)(a)(ii) - irreleva
Endorsed by: Katrin s22(1)(a)(ii)
- irreleva
Researcher: Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Aaron s22(1)(a)(ii)
- irrelevant ma
1. Contents
Support workers administering medication in Australia .............................................................. 1
1. Contents .......................................................................................................................... 1
2. Summary ......................................................................................................................... 2
3. Administering medication in the context of high intensity supports ................................. 3
4. NDIS Practice Standards ................................................................................................ 4
5. Delegation and supervision of care ................................................................................. 4
6. Australian Community Industry Al iance Practice Guidelines .......................................... 5
Page 417 of 425
FOI 24/25- 0013
7. State and territory regulations ......................................................................................... 6
7.1
Australian capital territory ......................................................................................... 6
7.2
New South Wales ..................................................................................................... 6
7.3
Northern Territory ..................................................................................................... 6
7.4
Queensland .............................................................................................................. 6
7.5
South Australia ......................................................................................................... 7
7.6
Tasmania ................................................................................................................. 7
7.7
Victoria ..................................................................................................................... 7
7.8
Western Australia ..................................................................................................... 7
8. Gaps in the regulatory framework ................................................................................... 7
9. References ...................................................................................................................... 8
2. Summary
There is a lack of clarity regarding legal and policy requirements for disability support workers
who administer medications to clients. Federal regulations and policies regarding training and
delegation of care apply to NDIS providers and their employees. However, these regulations
are variously interpreted and inconsistently implemented. In addition, providers may develop
their own policies regarding minimum training standards or qualifications for staff administering
medication to clients.
State and territories take different approaches to regulating the supply and administering of
medication. Only New South Wales, Tasmania, Victoria and Western Australia explicitly make
allowances for carers, but these do not distinguish between formal and informal carers in most
instances. Only Tasmania’s legislation refers to disability support workers but this is only in the
context of disability support workers who receive funding from the Tasmanian state
government. Tasmania is also the only jurisdiction with a Medication Management Framework
that elaborates on the requirements of the legislation.
Regulations and policy relating to delivery of high intensity supports covers minimum skills and
knowledge required by disability support workers who administer medication:
• through an enteral tube
• via subcutaneous injection
• for participants requiring dysphagia supports
• for participants requiring support to prior to and after seizure.
No state or territory policy or legislation was found regulating the administering of medication
by disability support workers delivering high intensity supports.
Page 418 of 425
FOI 24/25- 0013
3. Administering medication in the context of high
intensity supports
High intensity supports can be provided in a participant’s NDIS plan if they require support for
frequent behaviours of concern or at least one of the activities described in the High Intensity
Support Skil s Descriptors (NDIA, 2023a). The high intensity support skil s descriptors assist
NDIS providers and disability support workers to understand the skil s required when
supporting participants with high intensity daily personal care activities (NDIS Commission,
2022). High intensity daily personal care activities are defined in
National Disability Insurance
Scheme (Provider Registration and Practice Standards) Rules 2018, Schedule 2 as including:
• complex bowel care
• enteral feeding and management
• severe dysphagia management
• tracheostomy management
• urinary catheter management
• ventilator management
• subcutaneous injections
• complex wound management (NDIS Commission, 2024).
Sections 29 – 35 of
National Disability Insurance Scheme (Quality Indicators for NDIS Practice
Standards) Guidelines 2018 specify that in order to meet their obligations under
NDIS
(Provider Registration and Practice Standards) Rules 2018, providers should ensure workers
are trained in the high intensity skil s descriptors relevant to the activity.
Regarding the administering of medication by disability support workers, the high intensity
skil s descriptors describe the knowledge and skil s required to administer medication:
• through an enteral tube
• via subcutaneous injection
• for participants requiring dysphagia supports
• for participants requiring support to prior to and after seizure (NDIS Commission, 2022).
These concepts (‘high intensity supports’, ‘high intensity daily personal care activities’) relate to
NDIS funded supports, NDIS provider registration categories and knowledge and skil s
required by disability support workers to ensure NDIS providers are meeting their obligations
regarding quality supports. High intensity support does not appear to be relevant outside of
these contexts. No State or Territory legislation, regulations or policy was found that mandates
medication of any kind be delivered by support workers meeting the high intensity skil s
descriptors.
Page 419 of 425
FOI 24/25- 0013
4. NDIS Practice Standards
The
NDIS (Provider Registration and Practice Standards) Rules 2018 states:
Each participant requiring medication is confident that their provider administers, stores
and monitors the effects of the participant’s medication and works to prevent errors and
incidents (s.26(2)).
Requirements of this practice standard are elaborated in section 26 of the
NDIS (Quality
Indicators for NDIS Practice Standards) Guidelines 2018. To meet this practice standard,
providers should ensure the relevant disability support workers:
• have access to all the information required to identify, monitor and administer
medication (s26(1))
• understand the effects and side-effects of the medication (s26(2))
• are aware of the steps to take in the event of an incident involving medication (s26(2)).
These practice standards are further elaborated in the NDIS Commission’s Workforce
Capability Framework.
5. Delegation and supervision of care
The Disability-Related Health Supports operational guideline describes the circumstances in
which disability support workers may deliver disability-related health supports. This can include
administering medication. In some circumstances, a registered nurse may delegate tasks to a
disability support worker:
It is the registered nurse who must decide if a task can be delegated or not, as they
remain responsible for the care being provided. A registered nurse can’t delegate a task
if your health needs are inconsistent or likely to change. Also, some tasks can’t be
delegated and wil need to be done by a registered nurse.
When a registered nurse delegates a task they retain responsibility for the tasks being
provided. Before a registered nurse can delegate a task to someone else, they must
make sure the person is trained and competent to do that task. They must also be
available for direct and indirect supervision of the person doing the task.” (NDIA, 2023,
p.13).
The Nursing and Midwifery Board of Australia (NMBA) is the regulatory body for nurses and
midwives in Australia. NMBA’s practice standards and decision-making frameworks do not
specify which tasks can be delegated, or which people these tasks can be to. Instead, the
guidance describes the responsibilities of the registered nurse and what factors are relevant to
decisions to delegate care (NMBA, 2022; 2016).
The
Registered Nurse Standards for Practice describes a registered nurse’s responsibility
regarding delegation and supervision of care:
Page 420 of 425
FOI 24/25- 0013
Delegations are made to meet peoples’ needs and to enable access to health care
services, that is, the right person is available at the right time to provide the right service.
The RN who is delegating retains accountability for the decision to delegate. They are
also accountable for monitoring of the communication of the delegation to the relevant
persons and for the practice outcomes. Both parties share the responsibility of making
the delegation decision, which includes assessment of the risks and capabilities. In
some instances delegation may be preceded by teaching and competence assessment
(NMBA, 2016, p.6).
The
Decision-making framework for nursing and midwifery provides some decision-making
guidance related to the delegation and supervision of care. When determining whether to
delegate tasks to another individual, a registered nurse should:
• have a comprehensive understanding of the patient’s health needs
• obtain consent from the patient to delegate the task and to delegate the task to the
nominated person
• consider the qualifications, experience, competence, and confidence of the nominated
person
• have the capacity to provide any required supervision and training to the nominated
person
• understand and consider relevant legislation and policy, including organisational
policies and procedures (NMBA, 2022, p.6).
6. Australian Community Industry Al iance Practice
Guidelines
The Australian Community Industry Al iance (ACIA) is a peak body for community services
organisations in Australia. ACIA has released a series of practice standards describing best
medication administering practices. These include:
• Medication Management in the Community
• Administration of Oral Medications in Community by Support Workers
• Administration of Non-Oral and Non Injectable Medication in Community
• Subcutaneous Injections in the Community by Support Workers
• Psychotropic Medication Management in the Community
• Diabetic Management in the Community
• Cytotoxic Medication Management in the Community.
However, it is not clear whether these practice standards are widely adopted within disability
services.
Page 421 of 425
FOI 24/25- 0013
7. State and territory regulations
Not all regions have frameworks in place to regulate the administering of medication by
disability support workers (NDS, 2023; Duckworth & Wilson, 2022). Al states and territories
have legislation which allows people to administer, or assist others to self-administer,
medication. New South Wales, Tasmania, Victoria and Western Australia explicitly make
allowances for carers, but do not distinguish between formal and informal carers in most
instances. Only Tasmania refers to disability support workers but this is only in the context of
disability support workers who receive funding from the Tasmanian state government.
7.1 Australian capital territory
Section 5.2.361 of the
Medicines, Poisons and Therapeutic Goods Regulation 2008 (ACT)
authorises someone to administer medication to another person if the medicine was legally
supplied and is administered:
• according to the instructions on the label
• with the consent of the person taking the medicine or their legal guardian.
7.2 New South Wales
Section 10.4(c1) of the
Poisons and Therapeutic Goods Act 1966 (NSW) and section 59.1 of
the
Poisons and Therapeutic Goods Regulation 2008 (NSW) authorise a carer to administer or
supply medication to another person if the medication is supplied and administered according
to a valid prescription.
7.3 Northern Territory
According to the
Medicines, Poisons and Therapeutic Goods Act 2012 (NT), a prescription can
act as an authorisation to administer medication to a person. Provided that the instructions of a
valid prescription are followed, any person may administer:
• schedule 3 drugs (s75.2)
• schedule 4 and 8 drugs (s76.3).
7.4 Queensland
Section 51.1 of the
Medicines and Poisons Act 2019 (Qld) allows anyone to administer
medication to another person if the medication has been lawfully supplied and is administered
according to the instructions on the label. Section 34.1-2 extend this for people administering
schedule 4 and schedule 8 drugs.
Page 422 of 425
FOI 24/25- 0013
7.5 South Australia
Section 18.1d(c) of the
Controlled Substances Act 1984 (SA) allows a person to administer a
controlled drug to another person if the drug was lawfully prescribed or supplied to that other
person.
7.6 Tasmania
Sections 127 and 128 of the
Poisons Regulations 2018 (Tas) explicitly allows disability support
workers funded by the Tasmanian government to administer or assist with the self-
administering of medications providing the person being assisted has a lawful prescription.
Disability support workers must not administer schedule 8 medications unless the person they
are assisting does not have the capacity to self-administer or the medication is either
dexamphetamine, methylphenidate or lisdexamphetamine.
Section 135 of the
Poisons Regulations 2018 extends the provisions described in sections 127
and 128 for anyone who “has the care of, and responsibility for” the person receiving the
medication.
These provisions are elaborated in Tasmania’s Medication Management Framework.
7.7 Victoria
Section 103 of the
Drugs, Poisons and Controlled Substances Regulations 2017 (Vic) allows
those caring for someone prescribed schedule 4, 8 or 9 medications to administer that
medication.
7.8 Western Australia
Section 14.4(e) of the
Medicines and Poisons Act 2014 (WA) allows a person to possess
schedule 4 or 8 medicines if they are a carer for someone with a lawful prescription and they
intend to administer or supply the medicine to that person.
8. Gaps in the regulatory framework
There is a lack of clarity regarding legal and policy requirements for disability support workers
who administer medications to clients (NDS, 2023; Disability Royal Commission, 2023;
Duckworth & Wilson, 2022; O’Donovan, 2022). An analysis in the context of medication
administration for people with intellectual disability notes the lack of legislative coverage:
With respect to medications, national legislation includes the Therapeutic Goods Act
(1989) and the Poisons Standard (2021), but neither relate to the administration of
medication. On the other hand, state and territory legislation regulate the use and
possession of poisons and medications in specified settings, although most predate the
NDIS, and there is considerable variability regarding relevance or reference to
disabilities (Duckworth & Wilson, 2022, pp.75-76).
Page 423 of 425
FOI 24/25- 0013
The
Quality Use of Medication report identifies the following difficulties with implementing
existing policy:
• existing guidance is high level and lacks details
• variations in service providers’ organisational policy and interpretation of national
standards
• minimal guidance to distinguish between administering medication, assisting with
administering medication and assisting with self-administering medication.
The report also notes:
The intersections between disability and health; national and state governments; the
rights of the patient; the role and responsibility of support staff and disability support
providers; the place and availability of community, practice, and specialist nurses; and
the professional responsibility of doctors are currently inadequately defined and
regulated with respect to medication use, oversight, and monitoring (NDS, 2023, p.11).
9. References
Duckworth, N. J., & Wilson, N. J. (2022). Medication oversight, governance, and administration
in intellectual disability services: Legislative limbo.
Research and Practice in Intellectual
and Developmental Disabilities,
9(1), 73-83.
https://doi.org/10.1080/23297018.2021.2015424
National Disability Insurance Agency. (2023a).
Pricing Arrangements and Price Limits 2023-
24. https://www.ndis.gov.au/providers/pricing-arrangements
National Disability Insurance Agency. (2023).
Disability-Related Health Supports.
https://ourguidelines.ndis.gov.au/supports-you-can-access-menu/disability-related-
health-supports
NDIS Quality and Safeguards Commission. (2024).
High Intensity Daily Personal Activities.
Australian Government. https://www.ndiscommission.gov.au/providers/registered-ndis-
providers/provider-obligations-and-requirements/high-intensity-daily-personal-activities
NDIS Quality and Safeguards Commission. (2022). High Intensity Support Skil s Descriptors.
Australian Government. https://www.ndiscommission.gov.au/sites/default/files/2022-
12/Revised%20High%20Intensity%20Support%20Skil s%20Descriptors.pdf
Nursing and Midwifery Board of Australia. (2022).
Decision-making framework for nursing and
midwifery. The Australian Health Practitioner Regulation Agency.
https://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-
Statements/Frameworks.aspx
Nursing and Midwifery Board of Australia. (2016).
Registered nurse standards for practice. The
Australian Health Practitioner Regulation Agency.
Page 424 of 425
FOI 24/25- 0013
https://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Professional-
standards/registered-nurse-standards-for-practice.aspx#
Page 425 of 425