Resear
Resear
FOI
ch pap
23/24-1015
er
OFFICIAL
For Internal Use Only
Myalgic encephalomyelitis / Chronic fatigue
syndrome
The content of this document is OFFICIAL.
Please note:
The research and literature reviews collated by our TAB Research Team are not to be shared
external to the Branch. These are for internal TAB use only and are intended to assist our
advisors with their reasonable and necessary decision-making.
Delegates have access to a wide variety of comprehensive guidance material. If Delegates
require further information on access or planning matters, they are to call the TAPS line for
advice.
The Research Team are unable to ensure that the information listed below provides an
accurate & up-to-date snapshot of these matters
Research questions: What are the diagnostic features of ME-CFS?
What is the prognosis for someone diagnosed with ME-CFS? What factors affect prognosis?
What evidence-based treatment or management strategies are most effective for people
with ME-CFS?
What is the prevalence of communication difficulties for people diagnosed with ME-CFS?
What evidence-based treatment or management strategies are most effective for addressing
communication difficulties caused by ME-CFS?
Date: 18/3/2024
Requestor: Nicole s22(1)(a)(ii) - irrelevant ma
Endorsed by: Jane s22(1)(a)(ii) - irrelev
Researcher: Aaron s22(1)(a)(ii)
- irrelevant ma
Cleared by: Stephanie s22(1)(a)(ii) - irrelevant mat
ME-CFS
Page 1 of 10
OFFICIAL
Page 1 of 10
 Resear
Resear
FOI
ch pap
23/24-1015
er
OFFICIAL
For Internal Use Only
1. Contents
Myalgic encephalomyelitis / Chronic fatigue syndrome .............................................................. 1
1.
Contents ....................................................................................................................... 2
2.
Summary ...................................................................................................................... 2
3.
What is ME-CFS? ......................................................................................................... 3
3.1 Symptoms .................................................................................................................. 3
3.2 Diagnosis ................................................................................................................... 3
4.
Management and recovery ........................................................................................... 4
4.1 Pacing ........................................................................................................................ 6
4.2 Cognitive behavioural therapy ................................................................................... 6
4.3 Exercise and physical activity .................................................................................... 7
5.
Communication difficulties in ME-CFS .......................................................................... 7
6.
References ................................................................................................................... 8
2. Summary
Myalgic encephalomyelitis-Chronic fatigue syndrome (ME-CFS) is a condition characterised by
excessive fatigue, especially after activity, along with a wide variety of multi-system symptoms.
ME-CFS can be debilitating and result in significant functional impairment.
There are important sites of disagreement in research related to ME-CFS preventing strong
recommendations about diagnosis or management. The causes and mechanisms are stil
unclear. There are multiple definitions of ME-CFS with overlapping but distinct diagnostic
criteria. Estimates of those that recover or improve after an ME-CFS diagnosis vary widely
from 4% to 83%. There is no gold standard management strategy. There are some proposed
pharmacological and non-pharmacological treatments, though their efficacy is stil debated.
Cognitive behavioural therapy, exercise therapy and energy conservation techniques are
widely recommended though evidence in support of these strategies is often of low or very low
quality.
Communication difficulties are a recognised symptom of ME-CFS. Word finding problems are
the most reported speech dif iculty. No studies or recommendations were found that directly
address problems with language or communication in ME-CFS.
ME-CFS
Page 2 of 10
OFFICIAL
Page 2 of 10
 Resear
Resear
FOI
ch pap
23/24-1015
er
OFFICIAL
For Internal Use Only
3. What is ME-CFS?
3.1 Symptoms
ME-CFS may include chronic, severe and unexplained fatigue, along with other symptoms
affecting bodily functions including sleep, circulation, respiration, digestion, mood, cognition,
thermoregulation, and sensory processing (Steiner et al, 2023; Grach et al, 2023; NICE,
2021a-b; Deumer et al, 2021).
According to the UK’s National Institute for Health and Care Excellence (NICE), core
symptoms of ME-CFS include:
• Debilitating fatigue that is worsened by activity, is not caused by excessive cognitive,
physical, emotional or social exertion, and is not significantly relieved by rest.
• Post-exertional malaise after activity in which the worsening of symptoms:
is often delayed in onset by hours or days
is disproportionate to the activity
has a prolonged recovery time that may last hours, days, weeks or longer.
• Unrefreshing sleep or sleep disturbance (or both), which may include:
feeling exhausted, feeling flu-like and stiff on waking
broken or shallow sleep, altered sleep pattern or hypersomnia.
• Cognitive difficulties (sometimes described as 'brain fog'), which may include
problems finding words or numbers, difficulty in speaking, slowed responsiveness,
short-term memory problems, and dif iculty concentrating or multitasking (2021a,
p.12).
3.2 Diagnosis
There are different sets of diagnostic criteria used in research and medical practice (Steiner et
al, 2023; Grach et al, 2023; NICE, 2021a-b; Deumer et al, 2021; Bateman et al, 2021; Noor et
al, 2021).
The World Health Organisation (WHO) states, “Currently there is no consensus agreement
amongst medical professionals as to how chronic fatigue syndrome may be definitively
diagnosed” (WHO, n.d.). This is because “Without a biomarker it is not possible to definitively
know if a person has or does not have ME/CFS. Without such a reference standard (or ‘gold
standard’) it is not possible to assess the measurement validity of the dif erent criteria” (NICE,
2021b, p.47).
ME-CFS
Page 3 of 10
OFFICIAL
Page 3 of 10
 Resear
Resear
FOI
ch pap
23/24-1015
er
OFFICIAL
For Internal Use Only
Nevertheless, different sets of diagnostic criteria may be justified on pragmatic grounds,
including ability to distinguish between cases and controls or the preference for over- or under-
diagnosis (NICE, 2021b).
Emerge, the Australian peak body supporting people with ME-CFS, endorses the United
States’ National Academy of Medicine diagnostic criteria:
Diagnosis requires that the patient have the fol owing three symptoms:
• A substantial reduction or impairment in the ability to engage in pre-illness levels of
occupational, educational, social, or personal activities that persists for more than 6
months and is accompanied by fatigue, which is often profound, is of new or definite
onset (not lifelong), is not the result of ongoing excessive exertion, and is not
substantially alleviated by rest
• Post-exertional malaise
• Unrefreshing sleep.
At least one of the two following manifestations is also required:
• Cognitive impairment
• Orthostatic intolerance (Institute of Medicine, 2015, p.6)
This contrasts with the 2021 NICE clinical guideline in three ways. According to the NICE
criteria:
• Diagnosis can be made when symptoms are present for a minimum of 6 weeks for
adults and 4 weeks for children.
• Cognitive symptoms are necessary for diagnosis.
• Symptoms cannot be explained by another condition (NICE, 2021a).
4. Management and recovery
Researchers disagree about whether there are effective treatments for ME-CFS (Vink & Vink-
Niese, 2023; NICE, 2021a). There is still ongoing debate regarding the use of cognitive
behavioural therapy and graded exercise programs. Seton et al (2024) identify a number of
antivirals and other pharmacological treatments that may be effective but require further
investigation.
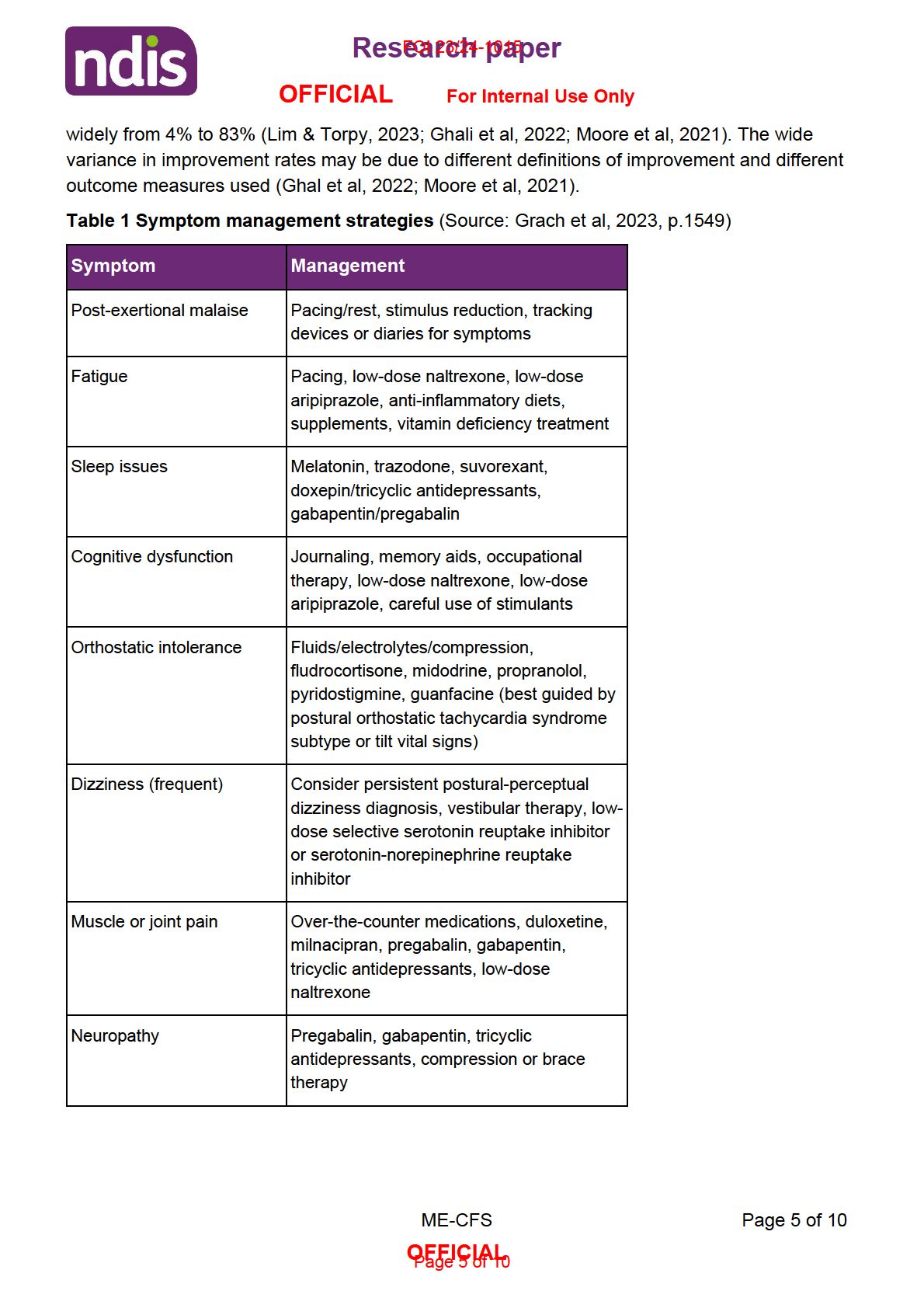
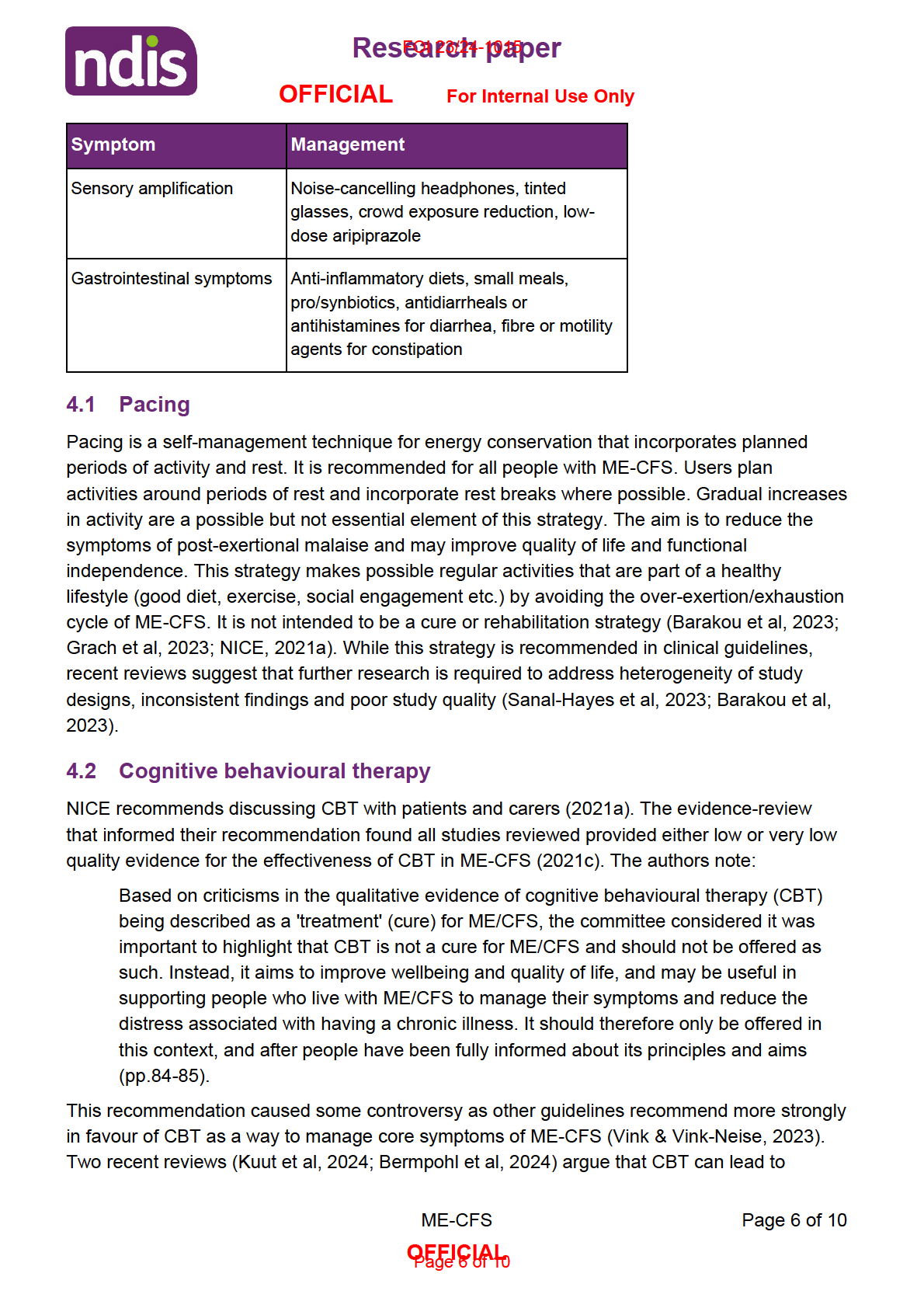
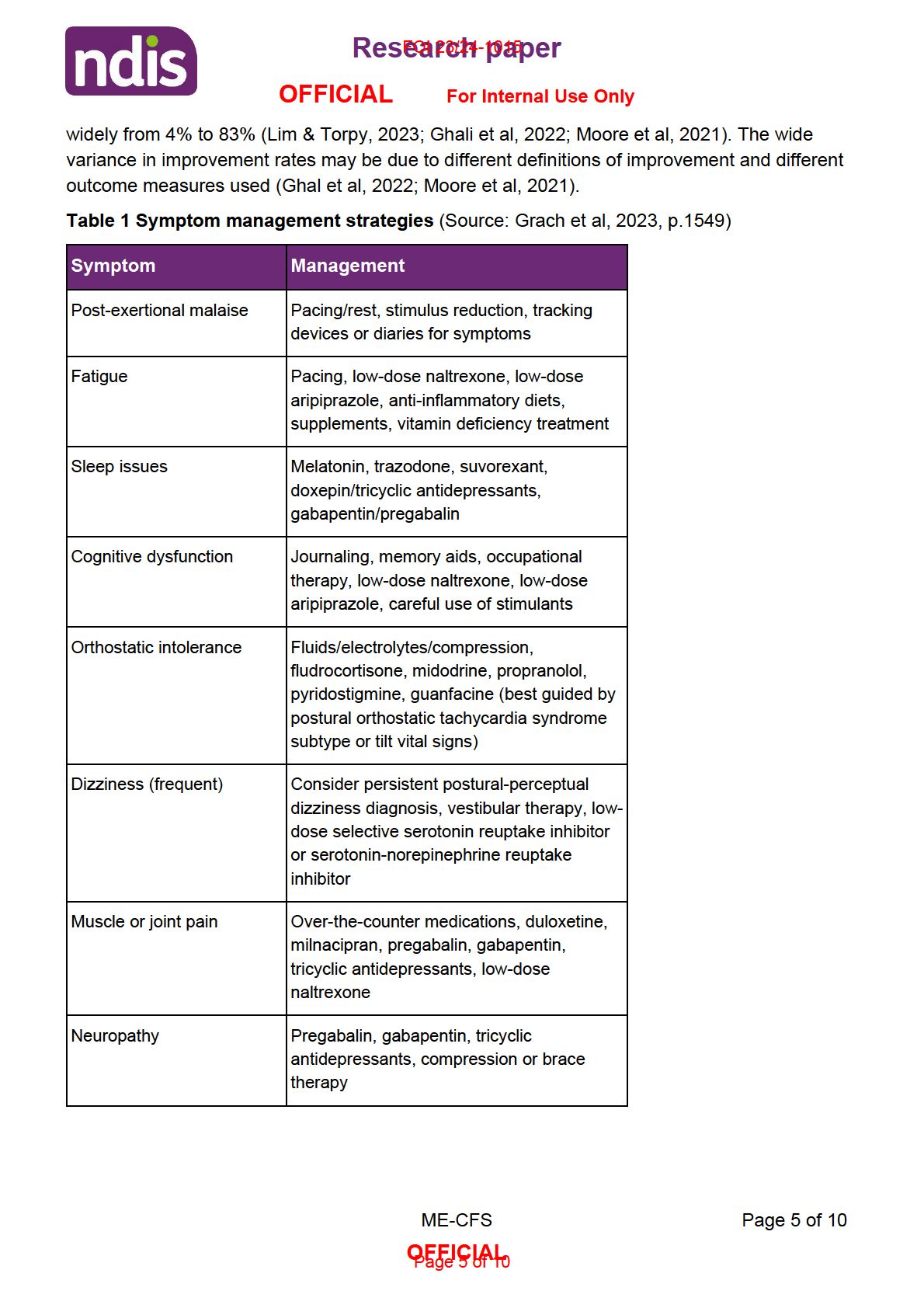
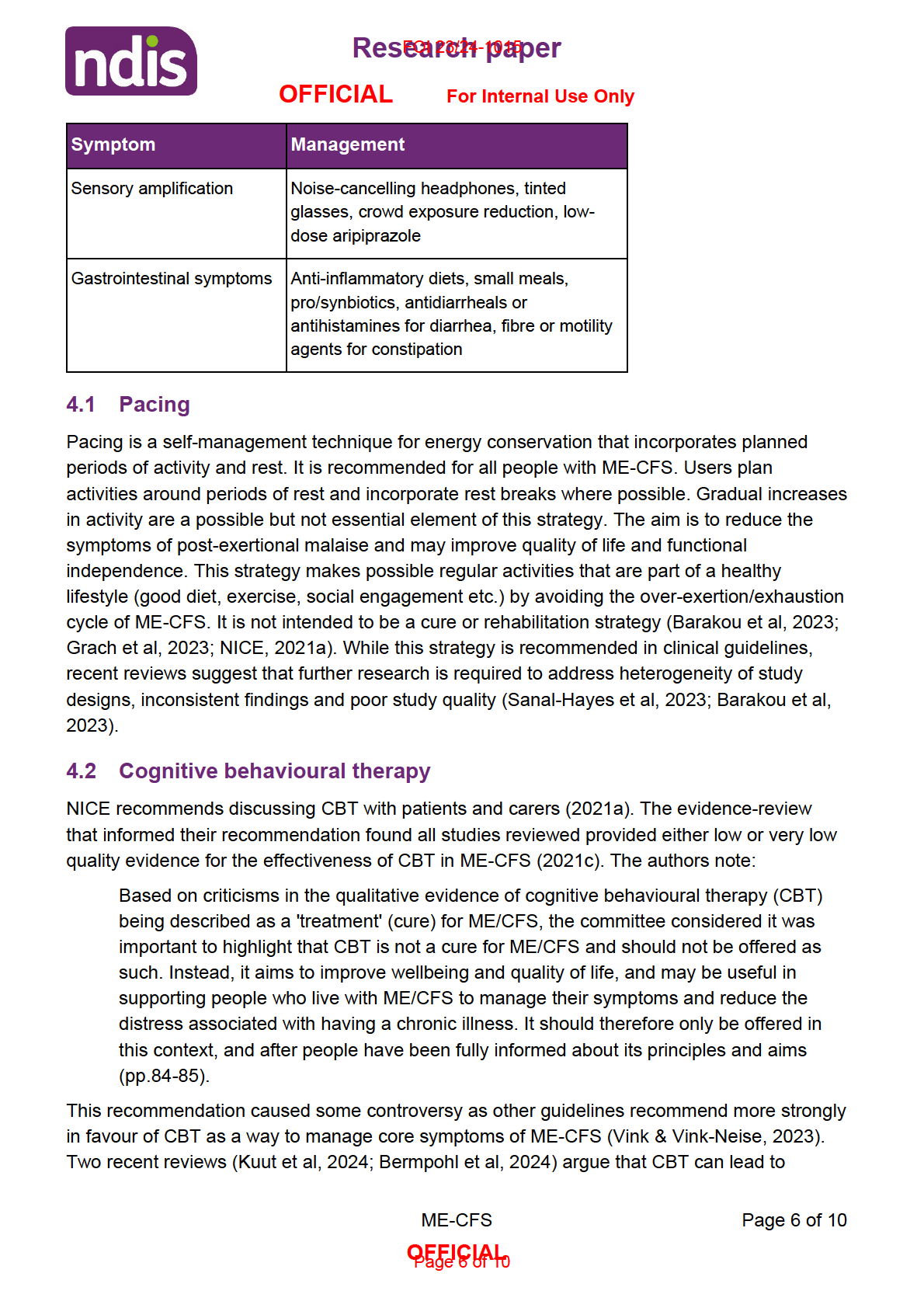
Most clinical guidelines focus on symptom management and lifestyle changes. Lifestyle
interventions include strategies such as scheduling activities and rest, ensuring good sleep
hygiene and appropriate diet.
Reported recovery rates for people with ME-CFS are likely low, with one study reporting 8%
recovery rate in a sample of 168 people (Ghali et al, 2022). Reported improvement rates vary
ME-CFS
Page 4 of 10
OFFICIAL
Page 4 of 10
 Resear
Resear
FOI
ch pap
23/24-1015
er
OFFICIAL
For Internal Use Only
significant reductions in fatigue, depression, anxiety and improvements in functional
impairment and physical activity.
Kuut et al (2024) performed a meta-analysis incorporating data from 8 randomised controlled
trials and including 1298 participants. They found statistical y significant effects on fatigue,
functional impairment and physical functioning. Ef ects were smal er for older people and
people with more severe functional impairment. The authors found no significant effects on
physical functioning for people with low levels of self-ef icacy. Of note, none of the studies
reviewed had low risk of bias and al 8 studies were conducted by the authors’ own research
group.
Bermpohl et al (2024) performed a meta-analysis incorporating data from 15 randomised
controlled trials and including 2015 participants. They found small to moderate effects on
fatigue, depression and anxiety. Of note, the studies reviewed were rated as either high risk of
bias or as having some concerns.
4.3 Exercise and physical activity
Regarding exercise programs, the NICE guidelines do not recommend graded exercise
programs or unstructured exercise programs. Instead, if the patient understands and requests
a personalised exercise program, the program should begin with activities below their baseline
level and ensure that they can tolerate that level for a period of time. The authors state:
The committee concluded any programme using fixed incremental increases in physical
activity or exercise (for example, graded exercise therapy), or physical activity or
exercise programmes that are based on deconditioning and exercise avoidance
theories, should not be offered to people with ME/CFS. The committee also wanted to
reinforce that there is no therapy based on physical activity or exercise that is effective
as a cure for ME/CFS (2021a, p.78).
These recommendations were controversial. Some researchers argued that the
recommendation against graded exercise therapy does not reflect the definitions of that
approach used in the studies that NICE reviewed, and ignores some studies that show benefit
of low intensity exercise for some people with ME-CFS (White et al, 2023). Wormgoor and
Rodenburg (2021) found some evidence that graded exercise therapy improves fatigue as
measured by participant self-report measures. However, objective measures of fitness, level of
physical activity and employment showed no benefit.
5. Communication difficulties in ME-CFS
Cognitive difficulties are either common in or essential to ME-CFS, depending on the set of
diagnostic criteria. Five of the nine sets of diagnostic criteria reviewed by NICE (2021b) include
word finding problems as an example of cognitive symptoms (Grach et al, 2023; Lim & Torpy,
2023; NICE, 2021a-b; Maksoud et al, 2020; Institute of Medicine, 2015). Grach et al (2023)
suggest that word finding and language processing problems could be a feature of post-
ME-CFS
Page 7 of 10
OFFICIAL
Page 7 of 10
 Resear
Resear
FOI
ch pap
23/24-1015
er
OFFICIAL
For Internal Use Only
exertional malaise, which is a core symptom of ME-CFS on several definitions. However, the
extent or severity of linguistic problems in ME-CFS is not clear. One study found around 75%
of subjects experienced difficulties with words, though the authors do not elaborate on the
type, frequency or severity of the difficulty (Institute of Medicine, 2015).
Evidence presented in a 2022 meta-analysis of cognitive impairments in ME-CFS shows an
uneven picture of linguistic ability (Sebaiti et al; 2022). The authors found a moderate to large
effect of ME-CFS on language processing speed (as measured by Colour/Word tests) and
long-term verbal memory (as measured by California verbal learning test recognition,
Weschler logic and reading tests). They found no significant effect on instrumental linguistic
skills (as measured by the Boston Naming Test and Weschler Adult Intelligence Test), short
term verbal memory (as measured by Digit Span Forward and Backward) or linguistic
efficiency (as measured by National Adult Test Reading and Weschler Adult Intelligence Test).
No studies were found that address management of language or communication impairment
for people with ME-CFS.
6. References
Barakou, I., Hackett, K. L., Finch, T., & Hettinga, F. J. (2023). Self-regulation of effort for a
better health-related quality of life: a multidimensional activity pacing model for chronic
pain and fatigue management.
Annals of medicine,
55(2), 2270688.
https://doi.org/10.1080/07853890.2023.2270688
Bateman, L., Bested, A. C., Bonil a, H. F., Chheda, B. V., Chu, L., Curtin, J. M., Dempsey, T.
T., Dimmock, M. E., Dowel , T. G., Felsenstein, D., Kaufman, D. L., Klimas, N. G.,
Komaroff, A. L., Lapp, C. W., Levine, S. M., Montoya, J. G., Natelson, B. H., Peterson,
D. L., Podel , R. N., Rey, I. R., … Yel man, B. P. (2021). Myalgic
Encephalomyelitis/Chronic Fatigue Syndrome: Essentials of Diagnosis and
Management.
Mayo Clinic proceedings,
96(11), 2861–2878.
https://doi.org/10.1016/j.mayocp.2021.07.004
Bermpohl, F. M. G., Kucharczyk-Bodenburg, A. C., & Martin, A. (2024). Ef icacy and
Acceptance of Cognitive Behavioral Therapy in Adults with Chronic Fatigue Syndrome:
A Meta-analysis. International journal of behavioral medicine, 10.1007/s12529-023-
10254-2. Advance online publication. https://doi.org/10.1007/s12529-023-10254-2
Deumer, U. S., Varesi, A., Floris, V., Savioli, G., Mantovani, E., López-Carrasco, P., Rosati, G.
M., Prasad, S., & Ricevuti, G. (2021). Myalgic Encephalomyelitis/Chronic Fatigue
Syndrome (ME/CFS): An Overview.
Journal of clinical medicine,
10(20), 4786.
https://doi.org/10.3390/jcm10204786
Ghali, A., Lacout, C., Fortrat, J. O., Depres, K., Ghali, M., & Lavigne, C. (2022). Factors
Influencing the Prognosis of Patients with Myalgic Encephalomyelitis/Chronic Fatigue
Syndrome.
Diagnostics (Basel, Switzerland),
12(10), 2540.
https://doi.org/10.3390/diagnostics12102540
ME-CFS
Page 8 of 10
OFFICIAL
Page 8 of 10
 Resear
Resear
FOI
ch pap
23/24-1015
er
OFFICIAL
For Internal Use Only
Grach, S. L., Seltzer, J., Chon, T. Y., & Ganesh, R. (2023). Diagnosis and Management of
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome.
Mayo Clinic proceedings,
98(10), 1544–1551. https://doi.org/10.1016/j.mayocp.2023.07.032
Institute of Medicine. (2015).
Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome:
Redefining an Il ness. Washington, DC: The National Academies Press.
https://doi.org/10.17226/19012.
Kuut, T. A., Buffart, L. M., Braamse, A. M. J., Csorba, I., Bleijenberg, G., Nieuwkerk, P., Moss-
Morris, R., Müller, F., & Knoop, H. (2024). Does the effect of cognitive behavior therapy
for chronic fatigue syndrome (ME/CFS) vary by patient characteristics? A systematic
review and individual patient data meta-analysis.
Psychological medicine,
54(3), 447–
456. https://doi.org/10.1017/S0033291723003148
Lim, W. T., & Torpy, D. J. (2023). Chronic Fatigue Syndrome. In K. R. Feingold (Eds.) et. al.,
Endotext. MDText.com, Inc.
Maksoud, R., du Preez, S., Eaton-Fitch, N., Thapaliya, K., Barnden, L., Cabanas, H., Staines,
D., & Marshall-Gradisnik, S. (2020). A systematic review of neurological impairments in
myalgic encephalomyelitis/ chronic fatigue syndrome using neuroimaging techniques.
PloS one,
15(4), e0232475. https://doi.org/10.1371/journal.pone.0232475
Moore, Y., Serafimova, T., Anderson, N., King, H., Richards, A., Brigden, A., Sinai, P., Higgins,
J., Ascough, C., Clery, P., & Crawley, E. M. (2021). Recovery from chronic fatigue
syndrome: a systematic review-heterogeneity of definition limits study comparison.
Archives of disease in childhood,
106(11), 1087–1094.
https://doi.org/10.1136/archdischild-2020-320196
National Institute for Health and Care Excellence. (2021a). Myalgic encephalomyelitis (or
encephalopathy)/chronic fatigue syndrome: diagnosis and management [NG206].
https://www.nice.org.uk/guidance/ng206
National Institute for Health and Care Excellence. (2021b). Myalgic encephalomyelitis (or
encephalopathy)/chronic fatigue syndrome: diagnosis and management: Identifying and
diagnosing ME/CFS [Evidence review].
https://www.nice.org.uk/guidance/ng206/evidence/d-identifying-and-diagnosing-mecfs-
pdf-9265183025
National Institute for Health and Care Excellence. (2021c). Myalgic encephalomyelitis (or
encephalopathy)/chronic fatigue syndrome: diagnosis and management: Non-
pharmacological management of CFS [Evidence review].
https://www.nice.org.uk/guidance/ng206/evidence/d-identifying-and-diagnosing-mecfs-
pdf-9265183025
Sanal-Hayes, N. E. M., Mclaughlin, M., Hayes, L. D., Mair, J. L., Ormerod, J., Carless, D.,
Hil iard, N., Meach, R., Ingram, J., & Sculthorpe, N. F. (2023). A scoping review of
'Pacing' for management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
ME-CFS
Page 9 of 10
OFFICIAL
Page 9 of 10
 Resear
Resear
FOI
ch pap
23/24-1015
er
OFFICIAL
For Internal Use Only
(ME/CFS): lessons learned for the long COVID pandemic.
Journal of translational
medicine,
21(1), 720. https://doi.org/10.1186/s12967-023-04587-5
Sebaiti, M. A., Hainselin, M., Gounden, Y., Sirbu, C. A., Sekulic, S., Lorusso, L., Nacul, L., &
Authier, F. J. (2022). Systematic review and meta-analysis of cognitive impairment in
myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Scientific reports,
12(1),
2157. https://doi.org/10.1038/s41598-021-04764-w
Seton, K. A., Espejo-Oltra, J. A., Giménez-Orenga, K., Haagmans, R., Ramadan, D. J.,
Mehlsen, J., & European ME Research Group for Early Career Researchers (Young
EMERG) (2024). Advancing Research and Treatment: An Overview of Clinical Trials in
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Future
Perspectives.
Journal of clinical medicine,
13(2), 325.
https://doi.org/10.3390/jcm13020325
Steiner, S., Fehrer, A., Hoheisel, F., Schoening, S., Aschenbrenner, A., Babel, N., Bellmann-
Strobl, J., Finke, C., Fluge, Ø., Froehlich, L., Goebel, A., Grande, B., Haas, J. P.,
Hohberger, B., Jason, L. A., Komaroff, A. L., Lacerda, E., Liebl, M., Maier, A., Mel a, O.,
… Scheibenbogen, C. (2023). Understanding, diagnosing, and treating Myalgic
encephalomyelitis/chronic fatigue syndrome - State of the art: Report of the 2nd
international meeting at the Charité Fatigue Center.
Autoimmunity reviews,
22(11),
103452. https:/ doi.org/10.1016/j.autrev.2023.103452
Vink, M., & Vink-Niese, A. (2023). The Draft Report by the Institute for Quality and Efficiency in
Healthcare Does Not Provide Any Evidence That Graded Exercise Therapy and
Cognitive Behavioral Therapy Are Safe and Effective Treatments for Myalgic
Encephalomyelitis/Chronic Fatigue Syndrome.
Diseases (Basel, Switzerland),
11(1), 11.
https://doi.org/10.3390/diseases11010011
White, P., Abbey, S., Angus, B., Bal , H. A., Buchwald, D. S., Burness, C., Carson, A. J.,
Chalder, T., Clauw, D. J., Coebergh, J., David, A. S., Dworetzky, B. A., Edwards, M. J.,
Espay, A. J., Etherington, J., Fink, P., Flottorp, S., Garcin, B., Garner, P., Glasziou, P.,
… Zeman, A. (2023). Anomalies in the review process and interpretation of the
evidence in the NICE guideline for chronic fatigue syndrome and myalgic
encephalomyelitis.
Journal of neurology, neurosurgery, and psychiatry,
94(12), 1056–
1063. https://doi.org/10.1136/jnnp-2022-330463
World Health Organization. (n.d.).
Chronic fatigue syndrome.
https://www.who.int/standards/classifications/frequently-asked-questions/chronic-
fatigue-syndrome
Wormgoor, M. E. A., & Rodenburg, S. C. (2021). The evidence base for physiotherapy in
myalgic encephalomyelitis/chronic fatigue syndrome when considering post-exertional
malaise: a systematic review and narrative synthesis.
Journal of translational medicine,
19(1), 1. https:/ doi.org/10.1186/s12967-020-02683-4
ME-CFS
Page 10 of 10
OFFICIAL
Page 10 of 10